Lucas is a 26 year old male who presents to the ED by his parents for bizarre behaviour and increasing aggression at home. He has a history of IV drug use but is not forthcoming about which drugs he has used and how recently he has used them. There are two hospital security employees behind him. He is frequently looking behind and around him, and appears dishevelled and unkempt. Lucas appears quite anxious and keeps saying “Where am I? Get off of me!”.
What is agitation and how can it present?
The term “agitation” can refer to an individual who is worried, anxious, upset, excited, or violent. In a clinical context, agitation can present in a spectrum . Patients often have repetitive motor activity (foot tapping, hair pulling, fiddling), and repetitive speech (“I’ve got to get out of here, I’ve got to get out of here”). Increased irritability, anxiety, responsiveness, restlessness and aggression have been associated with agitation.1 The course of agitation can be fluctuating, and patients can report feelings of mental distress and inner tension.2
Agitation is not a diagnosis, but a manifestation of many possible underlying pathologies. Only by safely de-escalating the agitated patient can we begin to address these underlying issues and understand the pathology behind their presentation.3 The etiology of a patient’s agitation will be discussed further in this module, however one should understand that these etiologies can be wide ranging, and also be impacted by their environment, social and medical history, genetics, among other factors. Some common causes of agitation in the ED include acute substance intoxication, substance withdrawal, psychiatric illness, delirium and dementia.4
Agitated patients can escalate to aggressive or violent behaviour, posing a risk to themselves, other patients, and hospital staff. A state of agitation can also be traumatizing for the patient to experience, and is considered an acute emergency requiring immediate intervention.1 It is thus important for any medical professional to understand how to safely, effectively, and compassionately deal with the agitated patient.
We hope to leave readers more comfortable dealing with these common yet extremely important situations in the ED, all while keeping the 4 objectives of the American Association of Emergency Psychiatry (AAEP) at the forefront1:
- Ensure the safety of the patient, staff, and others in the area.
- Help the patient manage their emotions and distress and maintain or regain control of their behaviour.
- Avoid the use of restraints when at all possible.
- Avoid coercive interventions that escalate agitation.
We must always remember that at the end of the day, our patients are human, and should be treated with respect and compassion at all times.
De-escalation
Verbal de-escalation is one of the most important skills to have in the Emergency Department. Effectively defusing an escalating situation is often the key to preventing a potentially dangerous situation for both staff and patients from occurring. Furthermore, an effective practitioner will be able to avoid serious interventions like involuntary restraints and medications, and be able to preserve patient autonomy. Patients put in restraints are more likely to be put into psychiatric facilities, and have longer inpatient lengths of stay.1 However, it is also important to note that safety is paramount; while the following approach reviews valuable tools in managing agitated patients, serious concern for the team’s safety should trigger escalation of resources and interventions.
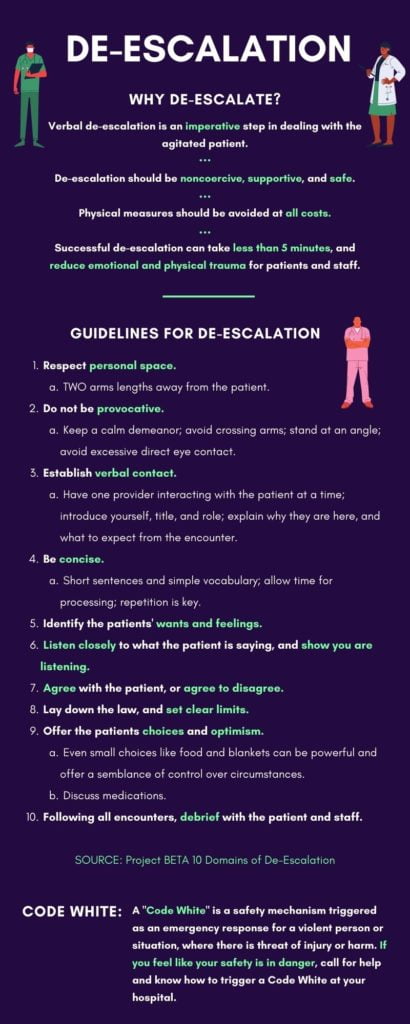
De-escalation should be noncoercive, supportive, and safe, and physical measures should be avoided at all costs. While chemical or physical restraints may be necessary in certain circumstances, verbal and non-verbal communication is almost always essential in engaging the patient in de-escalation. Staff and patients are less likely to get hurt when physical confrontation is averted, and the de-escalation process can be less emotionally and physically traumatizing for the patient and healthcare staff. Well trained staff can have patients successfully engage in these encounters in less than 5 minutes.1
Guidelines for general de-escalation
In the literature around de-escalation in the ED, the AAEP’s Project BETA1 is one of the best recognized guidelines to follow. The AAEP created the project BETA to shape this new practical and non-coercive approach to de-escalating agitated patients, regardless of the underlying etiology. Their General De-Escalation guidelines establishes 10 domains of de-escalation, which are summarized below with examples of how to implement each effectively in the ED.1
- Respect personal space
a. Position yourself at least 2 arms lengths away from the patient. This not only makes the patient and staff feel safe, but allows the staff to move away should the patient get violent. - Do not be Provocative
a. Maintain a calm demeanour and open body language
i. Keep hands visible and unclenched; avoid crossing arms.
ii. Stand at an angle from the patient so as to not appear confrontational. iii. Avoid excessive direct eye contact. - Establish Verbal Contact
a. Have only one provider interact with the patient at a time; orient the patient to where they are, why they are in the hospital, and what to expect from the encounter. - Be Concise
a. Use short sentences and simple vocabulary, allow them time to respond before continuing. Repetition is key – repeat your message until it is heard. - Identify Wants and Feelings
a. Some examples of wants: medication, administrative intervention, intervening with a loved one, the desire to talk to an empathic listener. - Listen closely to what the patient is saying
a. Active listening – verbal acknowledgement, body language, repeating back, clarifying statements.
b. Use Miller’s Law: “To understand what another person is saying, you must assume that it is true and try to imagine what it could be true of.” - Agree, or agree to disagree
a. Agree with the truth (Patient complains about the temperature, you say “yes it is quite cold in here, could we get you a blanket?”).
b. Agree in principle (Patient believes they have been treated unfairly, you say “I believe that everyone should be treated fairly”).
c. Agree with the odds (Patient is upset about waiting to see the psychiatrist, you say “odds are that other patients would be upset as well”). - Lay down the law and set clear limits
- Offer choices and optimism
a. Offering choices – even small choices (i.e. food, magazines, blankets, access to phone) can be powerful, and can offer empowerment and a semblance of control over their circumstances.
b. Discuss medications: for example, phrases such as “You seem stressed out – I think you could benefit from some medication to help calm you down” or “I think you need some medication to help calm you down – would you prefer a pill or injection?”. - Debrief the patient and staff
a. Debrief with patient:
i. Explain why the intervention was necessary.
ii. Ask what can be done by the staff in the future to help the patient stay in control.
iii. Importantly, debrief with the patient’s family who may have witnessed this traumatic incident.
b. Debrief the staff:
i. Discuss what went well, what didn’t, and what could be improved.
ii. Check in with staff – this can be a traumatic experience for them as well.
This can be a lot of information to remember, especially when in a stressful situation such as that when dealing with an agitated patient. At the end of the day, it is important to remember above all that these patients are human, and must be treated with respect and compassion. Ask them questions, make them feel safe, comfortable, and heard. These patients are likely scared and disoriented, and it is your job to work with them to help them feel back in control, not to work against them. Words are powerful tools that can more often than not de-escalate these difficult situations in a way that provides the least trauma and maintains a patient’s humanity.
Code White
Safety is paramount when treating potentially agitated and violent patients in the hospital setting. The Code White is a safety mechanism triggered as an emergency response for a violent person or situation, where there is threat of injury or harm. While comfort with de-escalation techniques is important, keep your own safety at the forefront as well; if you feel like your safety is in danger call for help and know how to trigger a Code White.
Despite your best efforts in de-escalating the situation, Lucas becomes increasingly agitated and paranoid, now starting to break away from the team of nurses and physicians. He begins to yell at staff and refuses to cooperate with any questioning. In the next post, we will discuss indications for chemical and physical restraints, and what else we should consider in our work-up of the agitated patient.
Further Reading on CanadiEM:
- https://canadiem.org/violence-and-agitation-in-the-emergency-department/
- https://canadiem.org/the-agitated-patient-in-the-ed-part-1/
- https://canadiem.org/the-agitated-patient-in-the-ed-part-2/
You can download the infographics for this post here and here.
This post was copy-edited by Casey Jones (@CaseyMAJones).
References
- 1.Richmond J, Berlin J, Fishkind A, et al. Verbal De-escalation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA De-escalation Workgroup. West J Emerg Med. 2012;13(1):17-25. doi:10.5811/westjem.2011.9.6864
- 2.Siddiqui W, Gupta V, Huecker MR. Agitation. StatPearls; 2021. https://www.ncbi.nlm.nih.gov/books/NBK493153/
- 3.Helman A. Emergency management of the Agitated Patient. Emergency Medicine Cases. https://emergencymedicinecases.com/emergency-management-agitated-patient/
- 4.Moore G, Pfaff J. Assessment and emergency management of the acutely agitated or violent adult. UpToDate. https://www.uptodate.com/contents/assessment-and-emergency-management-of-the-acutely-a gitated-or-violent-adult
Reviewing with the Staff
The agitated patient spans a range of bio-psycho-social challenges to themselves, physicians, nurses and allied healthcare staff.
Often stigmatized, their presentation can mask severe underlying pathology requiring timely intervention. While protecting the ED team is paramount, the main focus should remain with the patient. A calm, measured approach to de-escalation, restraints and sedation is necessary. A compassionate, open-minded approach to their subsequent management and disposition will ensure the best outcome for all involved.




