Our latest collaboration will see the publication of classic episodes of Emergency Medicine Cases published on CanadiEM. First10EM is an exceptional blog developed by fellow Canadian emergency physician, Dr. Justin Morgenstern. In the first episode of First10EM Classics on CanadiEM, Justin provides an approach to life-threatening asthma in the ED. -CanadiEM Editor Brent Thoma
The Case
A 16 year old female with a history of severe asthma is brought to your community emergency department after a week of respiratory symptoms that have suddenly become much worse. She has been admitted to hospital 4 times this year, including one visit to the ICU. Her respiratory rate is 45 and she is using every accessory muscle she has, but she doesn’t appear to be moving much air. In fact, her lungs are silent to auscultation. She looks tired and the monitor shows her vitals as a heart rate of 140, blood pressure of 99/60, and an oxygen saturation of 88%.
Immediate management of severe asthma in the ED
This patient is very sick with a history, vitals, and exam findings consistent with severe asthma and requires resuscitation. We all know the ABCs of resuscitation, but ‘A’ does not always need to be immediately addressed. Asthma is a respiratory problem not an airway problem. Unless the patient arrives in arrest, there is no reason to intubate immediately. Adding plastic to the airway only makes things worse.
The immediate action is to start oxygen and bronchodilators. In the severely ill asthmatic I don’t spend too much time debating the finer points of evidence based medicine. Give both albuterol (salbutamol for most countries) and ipratropium bromide. Also, stick to nebulizers in these patients.
- Oxygen: Asthmatic patients do not typically require a lot of supplemental oxygen. I apply nasal prongs to everyone, but typically skip the face mask because it is going to be replaced with a nebulizer anyway. Of course, nebulize with oxygen.
- Albuterol (and lots of it): You can give 5mg doses repeatedly or run a continuous nebulizer at 10-20mg/hr. It doesn’t really matter, as long as you get as much beta-2 agonist into the lung as possible.
- Ipratropium bromide: 500mcg nebulized every 20 minutes for 3 doses (don’t stop the albuterol nebulizer – mix the two together)
After oxygen and bronchodilators are started, my nurses hook the patient up to cardiorespiratory monitors and place 2 IVs. This often occurs simultaneously, as we have a large team in resus. However, if you are working with a smaller staff prioritize the breathing meds over the IV. I start a 20ml/kg bolus of my favorite crystalloid as soon as I have IV access because essentially all patients with severe asthma are dehydrated and they are also prone to hypotension when switched to positive pressure ventilation.
The definitive treatment of all asthma patients is corticosteroids. EBM nerds can wax on about oral and parenteral steroids being equivalent, but these patients need their steroids fast so they are getting them IV. Steroids will take a minimum of 6 hours to have a noticeable effect. Therefore, they are unlikely to help you in the resus room, but the earlier they are given the earlier then are able to work. In the critically ill asthma patient, other therapies (e.g. RSI medications, IV fluids, vasopressors, non-invasive ventilation) may be prioritized over steroids. Focus on the therapies that will help the patient immediately, but get a dose of intravenous steroids on board as soon as you have a minute. Any corticosteroid should be fine, methylprednisolone 125mg IV and hydrocortisone 100mg IV are used most commonly.
The final medication that I routinely include in the management of life threatening asthma is magnesium. That may be a controversial statement and I certainly do not use magnesium in asthma patients who aren’t actively dying, but there is a modicum of evidence that the sicker you are the more likely magnesium is to help you. The dose of magnesium sulfate is 2 grams IV repeated up to 3 times in the first hour.
If the patient is not improving with these first line therapies, I consider two second line medications: epinephrine and ketamine.
Epinephrine in the management of severe asthma
Epinephrine has a theoretical advantage for asthmatics who have not quickly responded to beta-2 agonists: it will act as an alpha agonist which may help decrease airway edema as well as providing additional beta-2 agonism. Epinephrine can be safely given to asthmatic patients of any age (see Cydulka 1998 in references). Some practitioners will use terbutaline instead of systemic epinephrine, and that is reasonable, but I prefer epinephrine because it is common medication we are all very comfortable dosing, it adds alpha effects, and I can provide push doses if needed.
Nebulised epinephrine
- 0.5ml of 2.25% racemic epinephrine
- 5ml of 1:1000 L-epinephrine
Systemic epinephrine
- IM 0.5mg
- IV infusion – start at 5mcg/min and titrate to effect
- Quick epinephrine drip: 1 mg of epinephrine in a 1L bag of saline. This results in a concentration of 1mcg/mL. Therefore a 60ml/hr infusion will give you 1 mcg/min
- Terbutaline can be used instead (10mcg/kg initial bolus over 10 minutes, then 0.4mcg/kg/min)
Ketamine (+/- Delayed Sequence Intubation) and BiPAP in the management of severe asthma
If the patient is agitated (probably secondary to hypoxia) ketamine is my agent of choice, theoretically as part of a delayed sequence intubation. Ketamine is used to treat agitation, allow for proper pre-oxygenation of the patient, and get the rest of the medications on board. Non-invasive positive pressure ventilation can be used as part of this pre-oxygenation. There are reports of patients improving after the combination of ketamine and BiPAP, obviating the need for intubation. The plan is to use ketamine to pre-oxygenate and buy time to prepare for a safe, controlled intubation.
If the patient is not improving with maximal medical management, it is time to start thinking about positive pressure ventilation and intubation. A common teaching is: when thinking about intubating an asthma patient, wait, and then wait some more, and then continue to wait, but don’t wait too long. If you are considering intubation, BiPAP should almost certainly be tried first. Remember that putting a piece of plastic in the trachea does nothing to help these patients. In fact, it increases airway resistance and dead space. The reason you considering intubation is because of respiratory fatigue and BiPAP can provide exactly the pressure support that these patients need.
Key points for the use of NIPPV in the management of severe asthma:
- These patients need to be constantly reassessed
- All of your intubation equipment should be ready at the bedside
- The benefit of BiPAP comes from the pressure support. Start around 8-10mmHg
- Set the PEEP low (1-2) – some clinicians recommend no PEEP at all if your machine will allow
- Continue providing beta2 agonists and the full kitchen sink of medical management. NIPPV only allows the patient to temporarily rest their respiratory muscles, it does not solve the underlying asthma pathophysiology.
If BiPAP doesn’t work and you have waited longer than you feel comfortable, the patient may need to be intubated. In emergency medicine, we love the airway, but asthma is one scenario that we should be wary of grabbing a laryngoscope. Why? Well, in addition to the normal critical care sympathetic tone that we will obliterate with our sedative, these patients are generally hypovolemic and have significant lung hyperinflation which limits venous return. This physiology sets them up for hemodynamic collapse. Add to that hypercapnea, acidosis, and hypoxia and it is not hard to understand why the chances of a peri-intubation arrest are so high.
Intubating patients with severe asthma
There are some reasonable arguments to be made for an awake intubation, however, in this critically ill patient I want to stay within my comfort zone and ensure I am ideally set up for first pass success. Therefore, I use rapid sequence intubation. First, I prepare for post-intubation hypotension. I begin a fluid bolus. Either my nurse has prepared an epinephrine drip (if it wasn’t already running) or I have push dose epinephrine drawn up and ready. I have also pre-set my ventilator so there aren’t any mistakes.
Rapid Sequence Intubation
- Nasal cannula on at set at 15L/min for a no desat approach to intubation with apneic oxygenation
- Pristine patient positioning
- Ketamine 1.5mg/kg
- Rocuronium 1.5mg/kg
- Use a large endotracheal tube (this makes ventilating the patient easier and facilitates suction and bronchoscopy by our ICU colleagues)
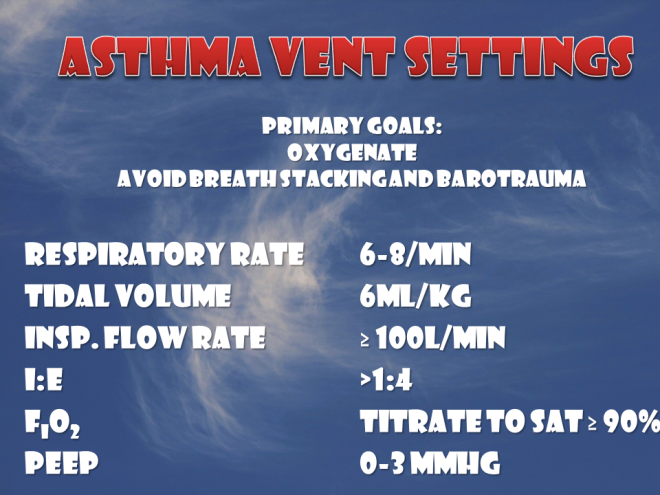
Unfortunately, passing the tube is only the beginning of your problems. We often ignore the vent and allow our RTs to be the experts. This is a situation where the wrong vent settings can kill the patient. They are at risk for barotrauma, volutrauma, and hemodynamic compromise from impaired venous return. The ventilator settings are essential.
Ventilator Settings
The goals are to main oxygenation while minimizing dynamic hyperinflation and barotrauma. The key is to allow as much time as possible to the patient to exhale. This will almost always require accepting some degree of hypercapnia. I would recommend starting with the following settings:
- Respiratory rate low (6-8/min) to start
- Small tidal volumes (6ml/kg of ideal body weight)
- Fast inspiratory flow rate (≥ 100L/min) to allow a long expiratory time (I:E >1:4 ie inspiratory to expiratory ratio of 1:4 or more)
- FiO2 100% initially then titrated down to keep sats > 90%
- Minimal or no PEEP (≤5)
- The ventilation mode does not matter to me initially because the patient will be paralyzed and sedated. However, be very careful if using assist control mode because if the patient is distressed and starts breathing on their own, they can quickly increase their respiratory rate, decrease their I:E ratio, limit their ability to exhale, and rapidly increase intrathoracic pressure through breath stacking.
- We are allowing hypercapnia to prevent significant autoPEEP and barotrauma. This can be very distressing, so significant sedation is required. A goal of a plateau pressure of less than 30mmHg is ideal (ask the RT if you are unsure how to check this – it requires measurement of pressures during a pause of ventilation during the expiratory phase). If the plateau pressure is too high, decreasing the respiratory rate can help.
Rescue options in the management of asthma
If, despite all of the above, your patient continues to worsen, there are several rescue options to consider. As these intervention goes beyond the ED, I will not cover them in detail.
Inhalational agents (isoflurane or sevoflurane) in the management of asthma
These agents are very effective bronchodilators that can be provided by our anesthesia colleagues who are usually happy to help.
ECMO (Extracorporeal Membrane Oxygenation)
Removing the lungs from the equation while continuing to treat the underlying inflammation and bronchospasm seems to make sense. There are obviously no randomized control trials to support the practice (fortunately, asthma this severe is not common), but there are a number of case reports. If your center has an ECMO team, it is probably worth getting them on the phone to discuss the patient.
Other
Some algorithms include Heliox for status asthmaticus but I did not include it in this post because there is little evidence to support it. The key problem for patients with life-threatening asthma is that the maximum FiO2 of Heliox is 40%, which may be inadequate for oxygenation. The authors of the Cochrane review on the topic conclude: “at this time, heliox treatment does not have a role to play in the initial treatment of patients with acute asthma”, but admit that there may be a role in patients with more severe airway obstruction, and, as always, note that more study is needed.
IV beta2 agonists are another treatment that is often discussed. There are two Cochrane reviews that conclude that there is very little evidence to support this. Unfortunately, trials generally don’t include the severely ill who are unable to tolerate inhaled beta2 agonist and those are the patients most likely to benefit from an IV route.
[bg_faq_start]Pediatric Dosing
This post focused included standard doses for adult patients, but it also can be seen in younger children. This section summarizes the dosing of the medications recommended above in children.
- Albuterol continuous nebulizer: 0.3mg/kg/hr OR:
- 5-10kg: 10mg/hr
- 10-20kg: 15mg/hr
- 20kg: 20mg/hr
- Albuterol intermittent nebulizer: 0.15mg/kg/dose OR:
- <2 years: 1.25mg/dose
- 2-5 years: 2.5mg/dose
- 5 years: 5mg/dose
- Ipratropium bromide
- <20kg: 250mcg/dose
- 20kg: 500mcg/dose
- IV fluid bolus: 20ml/kg
- Hydrocortisone: 3-5mg/kg
- Methylprednisolone: 1-2mg/kg IV
- Magnesium sulfate: 50mg/kg repeated up to 3 times in first hour
- Epinephrine nebulized:
- 0.05 mL per kg (maximal dose: 0.5 mL) of racemic epinephrine 2.25%
- 0.5 mL per kg (maximal dose: 5 mL) of L-epinephrine 1:1,000
- Epinephrine IM: 0.01mg/kg (max 0.5mg)
- Epinephrine IV: Start at 0.1-0.5mcg/kg/min
Visual Summary
Conclusion
Most asthma deaths are the result of poorly controlled disease that slowly deteriorates over days to weeks. Obviously, the best intervention for these patients would occur long before they arrive in extremis. This is the reason to take all asthma seriously and ensure every patient has follow-up and access to necessary medications.
Note 1: I was inspired by Salim Rezaie (@srrezaie) of REBEL EM to make some summary images for this post. They certainly aren’t up to Salim’s standards yet – but I will keep trying.
Note 2: This post was initially publisehd on First10EM on August 18, 2015. It was revised and republished on CanadiEM on April 1st, 2016 as part of a collaboration between CanadiEM and First10EM.
Other FOAMed Resources
The Crashing Asthmatic REBELCast
When the patient can’t breathe, and you can’t think: The emergency department life-threatening asthma flowsheet onEmergency Medicine Updates
EMCrit Podcast 15 – the Severe Asthmatic. Ventilator Management for the Asthmatic or COPD Patient, and Delayed Sequence Intubation (DSI) on EMCrit
Asthma…The Music Of The Night and Asthma and the Vent on thePEM ED podcast
Mechanical Ventilation for Severe Asthma on Pediatric EM Morsels
Pediatric Severe Asthma on the SCCM iCritical Care PodCast
A few more with an EBM focus:
The Crashing Asthmatic and The 3MG Trial on Emergency Medicine Ireland
JC: Does Magnesium work in asthma? on St. Emlyn’s
EBM Acute Asthma on Life in the Fastlane
Asthma Medications: where’s the evidence? on EMPEM.org
[bg_faq_end][bg_faq_start]References
- Holley AD, Boots RJ. Review article: management of acute severe and near-fatal asthma. Emerg Med Australas. 2009; 21(4): 259-68. PMID: 19682010 [Free Full Text]
- Stanley D, Tunnicliffe. Management of life-threatening asthma in adults. Contin Educ Anaesth Crit Care Pain. 2008;8(3): 95-99 [Free Full Text]
- Papiris S, Kotanidou A, Malagari K, Roussos C. Clinical review: severe asthma. Crit Care. 2002; 6(1): 30-44. PMID: 11940264 [Free Full Text]
- Wener RR, Bel EH. Severe refractory asthma: an update. Eur Respir Rev. 2013; 22(129): 227-35. PMID: 23997049 [Free Full Text]
- Shlamovitz GZ, Hawthorne T. Intravenous ketamine in a dissociating dose as a temporizing measure to avoid mechanical ventilation in adult patient with severe asthma exacerbation. J Emerg Med. 2011; 41(5): 492-4. PMID: 18922662
- Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012; 59(3): 165-75.e1. PMID: 22050948
- Weingart SD, Trueger NS, Wong N, Scofi J, Singh N, Rudolph SS. Delayed sequence intubation: a prospective observational study. Ann Emerg Med. 2015; 65(4): 349-55. PMID: 25447559
- Soroksky A, Stav D, Shpirer I. A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest. 2003; 123(4): 1018-25. PMID: 12684289
- Cydulka R, Davison R, Grammer L, Parker M, Mathews J 4th. The use of epinephrine in the treatment of older adult asthmatics. Ann Emerg Med. 1988; 17(4): 322-6. PMID: 3354935
- Travers A, Jones AP, Kelly K, Barker SJ, Camargo CA, Rowe BH. Intravenous beta2-agonists for acute asthma in the emergency department. Cochrane Database Syst Rev. 2001: CD002988. PMID: 11406055
- Travers AH, Milan SJ, Jones AP, Camargo CA Jr, Rowe BH. Addition of intravenous beta(2)-agonists to inhaled beta(2)-agonists for acute asthma. Cochrane Database Syst Rev. 2012; 12: CD010179. PMID: 23235685
- Rodrigo G, Pollack C, Rodrigo C, Rowe BH. Heliox for nonintubated acute asthma patients. Cochrane Database Syst Rev. 2006; : CD002884. PMID: 17054154