Vital signs are amongst the first pieces of patient information available to you in the acute setting. They play a role in many of the decisions we make in emergency medicine. Unfortunately, vital signs can be influenced by a number of factors and there are many situations in which vital signs are less than reliable. Abnormal vital signs can be an indicator of an underlying pathology, a variant due to medication, or a result of the environment. Learning how to interpret them can be difficult, but it is a crucial skill to master in pursuit of providing excellent care.
This blog post will give you a basic approach to interpreting abnormal vital signs, including lists of possible etiologies, while also outlining some common pitfalls and misleading scenarios to be aware of. These lists are not comprehensive, but they will act as a good starting point by providing you with a conceptual framework that you can further refine through your clinical experiences. Although management is beyond the scope of this article, you will find suggested resources regarding the management of the important alterations discussed.
It is also important to note that although this article focuses on adults, pediatric vital signs require nuanced interpretation due to variance in normal ranges by age as well as the unique ability children have to compensate for pathological changes.
The five vital signs we will be covering include temperature, heart rate (HR), blood pressure (BP), oxygen saturation (O2 sat), and respiratory rate (RR).
Temperature
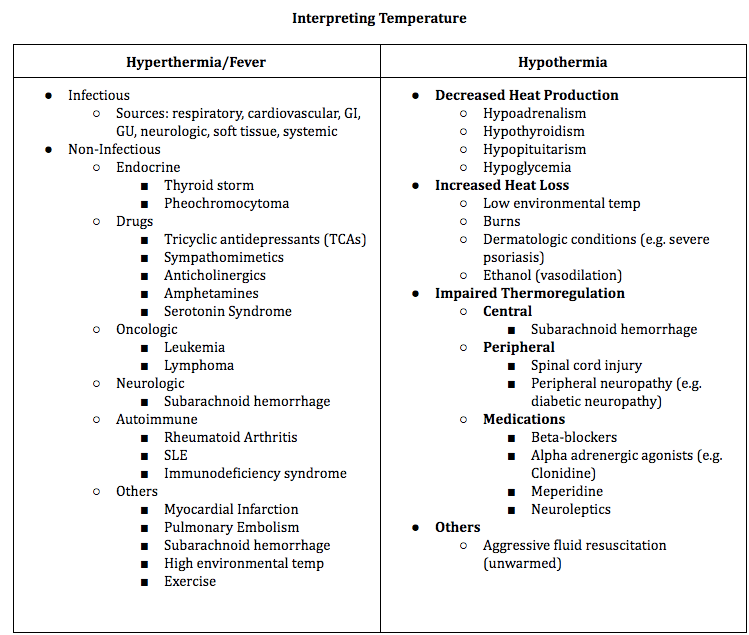
Temperature is controlled by the hypothalamus and varies throughout the day based on the circadian rhythm and environment. The normal range of temperature is considered to be from 36°C to 38°C. When body temperature is reduced, it is called hypothermia (generally less than 35°C). On the other hand, raised body temperature (above 38°C) can either be due to the body’s inability to dissipate heat (hyperthermia) or due to the production of pyrogenic molecules that raise body temperature (fever). Most temperatures above 41°C are due to hyperthermia, though fever can also raise the temperature to this level at times and should be considered.1
The causes of hyperthermia/fever can be categorized as infectious and non-infectious whereas hypothermia can be categorized by the causal mechanism including decreased heat production, increased heat loss, and impaired thermoregulation.2,3
| TEMPERATURE PITFALLS – Inability to Mount Fever & Masked Fever Older adults can have a baseline temperature that is 0.6 – 0.8° C lower than in younger adults. Additionally, in older adults, there is a decreased temperature response to infection due to age-related decreases in cytokine production, decreased hypothalamic sensitivity, and insufficient peripheral thermoregulation. These individuals are less likely to present with typical fever when fighting infection and can alternatively present with hypothermia. It is also vital to ask patients about any antipyretics taken that may mask a true fever, an important clue when working up a patient in the acute setting where information is limited as is. |
| For more information on approaching hypothermia, see this resource by EMBasic. The differential for fever is very broad. For a more comprehensive differential see this resource by WikiEM. Fever in the pediatric patient can be quite complex and is an important topic on its own. To learn more about how to approach pediatric fever, take a look at this resource by PediatricEM Morsels. |
Heart Rate
HR refers to the number of times the patient’s heart beats per minute and can be measured manually by palpating the patient’s pulse, or through various external and internal monitoring devices. A HR of 60 to 100 is considered normal for a healthy adult. A HR of more than 100 is considered tachycardia while less than 60 is referred to as bradycardia.
Tachycardia can be categorized as sinus tachycardia or a dysrhythmia whereas bradycardia can be divided into asymptomatic (due to variance in physiological baselines) and symptomatic.4,5

| HR PITFALLS – Relying on Monitoring Device & Masked Tachycardia The monitoring device often uses electrical signals to determine the patient’s HR. This method is not always reliable. For instance, if the patient has high t-waves, the device can sometimes pick these signals up as a second heartbeat, yielding a concerning heart rate that is double the patient’s actual HR. Remember that manually measuring the patient’s heart rate is the best source when possible. If your manual measurement is different from the reported HR, look at the patient’s ECG to identify where this discrepancy may be coming from. When patients take medications that slow their heart rate like beta-blockers, they may not reach a heart rate that is considered tachycardic despite being elevated from their baseline heart rate. A thorough medication history is important to be able to accurately interpret a patient’s heart rate. |
| Tachycardia is a complex topic, with each subsection filling a lecture of its own. Check out the following resources on sinus tachycardia and dysrhythmias. An approach to bradycardia can be found here on emDocs. |
Blood Pressure
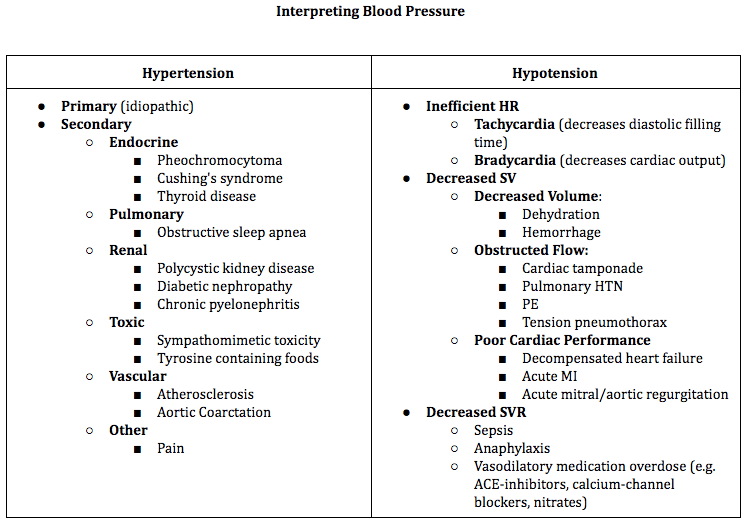
BP is the force that the patient’s circulating blood exerts on the walls of their vasculature. It is determined by cardiac output, blood volume, blood viscosity, systemic vascular resistance, and vessel compliance. Blood pressure is the product of cardiac output (CO) and systemic vascular resistance (SVR). Cardiac output in turn is a product of HR and stroke volume (SV). A good way to think about blood pressure is to consider the factors that can influence each of these elements.
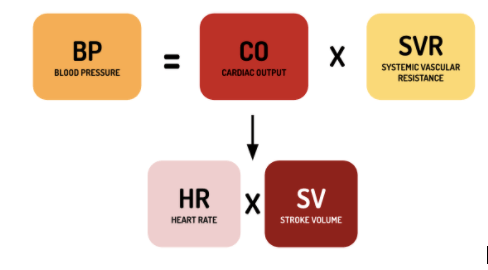
Despite the normal range of BP being SBP 90-120 and DBP 60-80, a patient’s baseline BP can vary widely from person to person. Elevated BP or hypertension is often a chronic disease managed in the primary care setting. In the ED, hypertension can be a clue regarding the patient’s presentation but it is also important to be able to identify hypertensive emergencies (BP >180/110) and manage them accordingly. Decreased BP or hypotension can have a multitude of causes and identification of the etiology is important when making resuscitation decisions. Referring to the above equations involving HR, SV, and SVR can be a good way to organize your thought process.
| BP PITFALL – Wrong Cuff Size The easiest way to optimize your blood pressure measurement is to use the correct cuff size. Using a cuff that is too small can yield a reading that is artificially high whereas a large cuff will yield an artificially low reading. The guideline is to use a cuff with a bladder length that is 80% of the patient’s arm circumference. The few minutes it might take to locate the appropriate cuff are worth it in order to have accurate information regarding your patient’s status. |
| Management of elevated blood pressure in the acute setting can be confusing. Take a look at this resource for a more in-depth discussion about hypertensive crises. An approach to hypotension by emDocs can be found here. |
Oxygen Saturation
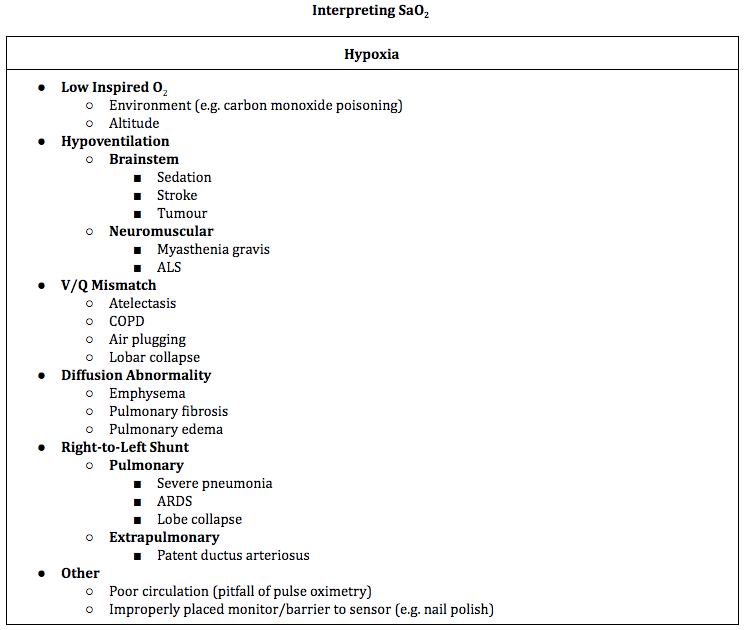
SaO2 is a measure of the fraction of saturated hemoglobin relative to total hemoglobin being assessed. In practice, this is generally measured with pulse oximetry, which provides an approximation of arterial SaO2. It is important to remember that SaO2 is an incomplete measure of a patient’s respiratory status. Despite measuring oxygenation (the process of introducing oxygen to the circulation), SaO2 sat does not assess ventilation (gas exchange). An arterial blood gas would be necessary to assess the patient’s ventilatory status.
Hypoxia is considered SaO2 <92% although there are different targets based on underlying disease states (e.g. 88 – 92% for patients with COPD). There are a number of causes for hypoxia that include environmental and pathological etiologies.6
| O2 SAT PITFALL – End Organ Perfusion A common misconception is that SaO2 is an indicator of end organ perfusion. A number of factors including anemia, hypovolemia, and peripheral vascular shutdown can all decrease end organ perfusion despite an SaO2 measurement of 100%. |
| Your management of hypoxia will vary based on the etiology but this resource provides a comprehensive review of possible interventions and prevention strategies. |
Respiratory Rate
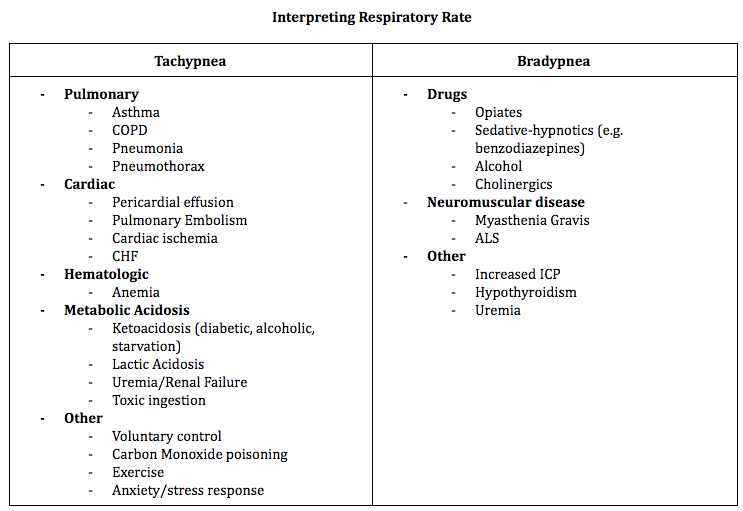
RR is the number of breaths a patient takes in a minute. RR is unique in that the patient can have voluntary control over their respiratory rate which adds nuance to how this vital sign is measured. The normal RR range is 12 to 20 breaths per minute. When RR is elevated (tachypnea) or lowered (bradypnea), it can be an early indicator of a patient’s status but can be influenced by a large number of factors. Respiratory drive is modulated by the neural central control system which sets the pace, the sensory input systems that modulate the pace, and the muscular effect system which transforms respiratory drive into the mechanical process of ventilation. Processes that affect any of these three components can influence RR.
| Your differential for tachypnea can be quite broad but this resource provides a more in-depth approach to investigating and managing tachypnea by emDocs. |
Putting it All Together
When you are presented with a patient’s vitals, it can be overwhelming trying to interpret all of the signs at once. Furthermore, these values can change during a patient’s time in the emergency department as their status changes. The concept of measuring orthostatic vitals is an excellent example of using interpreting vital signs serially and in conjunction with one another to assess for a hypovolemic state. Understanding the foundations and mechanisms behind each of these vital signs as well as the common pitfalls when it comes to measuring and interpreting them can help make this process easier.
Early warning scores, including the Modified Early Warning Score (MEWS) and National Early Warning Score (NEWS), have been developed to help assess a patient’s risk of adverse outcomes based on their vital signs. These scoring tools identify the recommended frequency of vital signs monitoring and level of care for the patient. Although early warning scores are not a substitute for methodically interpreting a patient’s vital signs, they are evidence-based tools that are built into many electronic medical records to account for the cognitive load associated with keeping track of these values when caring for multiple patients.7,8
Final Thoughts
Vital signs are a valuable source of information about a patient’s status early on in their encounter in the ED. It is important to cast a wide net when investigating why a patient’s vital signs may be abnormal and to consider a variety of systems. Medications can influence a number of vital signs by either causing an abnormality or masking one. Reassessment of a patient’s vital signs can be a useful indicator of response to therapy (e.g. fever resolution with antipyretics, or normotensive BP with fluid resuscitation). Whenever there are abnormalities in a patient’s vital signs, it is imperative that these abnormalities are either resolved or explained and accounted for prior to their departure from the department. Ultimately, vital signs are easily accessible initial clues to help direct your investigations and evaluate your patient’s status throughout their visit that you can take advantage of with the right skills.
Takeaways:
- Always account for or correct abnormal vital signs and document this process
- When an abnormal vital is measured, repeat the measurement and ensure that it has been measured correctly using the appropriate equipment for the patient
- A patient’s medication list as well as history of recent over the counter medication use can help account for certain abnormal vitals or unmask hidden abnormalities
- Maintain a broad differential involving multiple systems when considering the causes of abnormal vital signs
This post was edited and uploaded by Megan Chu.
- 1.Clifford K, Dy-Boarman E, Haase K, Maxvill K, Pass S, Alvarez C. Challenges with Diagnosing and Managing Sepsis in Older Adults. Expert Rev Anti Infect Ther. 2016;14(2):231-241. doi:10.1586/14787210.2016.1135052
- 2.Duong H, Patel G. statpearls. Published online March 18, 2020. http://www.ncbi.nlm.nih.gov/books/NBK545239/
- 3.Biem J, Koehncke N, Classen D, Dosman J. Out of the cold: management of hypothermia and frostbite. CMAJ. 2003;168(3):305-311. https://www.ncbi.nlm.nih.gov/pubmed/12566336
- 4.Gopinathannair R, Olshansky B. Management of tachycardia. F1000Prime Rep. 2015;7:60. doi:10.12703/P7-60
- 5.Gopinathannair R, Olshansky B. Management of tachycardia. F1000Prime Rep. Published online May 12, 2015. doi:10.12703/p7-60
- 6.Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: A Review of the 2018 GOLD Report. Mayo Clinic Proceedings. Published online October 2018:1488-1502. doi:10.1016/j.mayocp.2018.05.026
- 7.Subbe CP. Validation of a modified Early Warning Score in medical admissions. QJM. Published online October 1, 2001:521-526. doi:10.1093/qjmed/94.10.521
- 8.Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. Published online April 2013:465-470. doi:10.1016/j.resuscitation.2012.12.016
Reviewing with the Staff
This is a really comprehensive post that highlights the intricacies of vital signs interpretations. My only extension to this piece is that it is imperative to also fold in three general take home points:
Be wary of unexplained vital sign abnormalities when discharging a patient. Unexplained tachycardia can be super problematic. This can lead to repeat visits, or may be predictive of later admissions or worse outcomes.
Vitals signs are just numbers - remember to treat the patient not just the numbers! As much as there are “normal vital signs” at a population level, and that guidelines suggest certain targets - being too aggressive with any one adjustment can sometimes do more harm than good. For example, if an asymptomatic elderly patient who habitually has higher blood pressures, DO NOT try to emergently intervene to get their BP to 120/80. This may lead to hypoperfusion of their brain and do more harm than good. Know your patient’s historical trends and understand their physiologic leads. Exceptions to these rules would be acute hypertensive crises and/or intracranial hemorrhage - but for most medical students this will be wayyyy above your pay grade for now!
Develop your Gestalt by correlating with vitals and other clinical factors. As a junior clinician, your job is to consider how you can use vital signs or clinical decision tools like the MEWS to scaffold the development of your clinical gestalt. With experienced clinicians, these numbers are but one factor in a number of factors that can help them with diagnosis. If you aim for a career in emergency medicine, developing a “gut sense” (or Gestalt) about the way a patient looks sick or not can be a skill that you can develop over time - and can partially be guided by other experienced clinicians (eg Our experienced emergency nurses, RTs, PAs, NPS and docs) as well as informed by metrics like vital signs. Someday, with enough exposure and experience your system 1 diagnostic reasoning will kick in, allowing you to “eyeball” patients too.



