This updated episode of CRACKCast covers Rosen’s Chapter 019, Red and Painful Eye (9th Ed.). This podcast assists with the extensive differential and specific management plans to the inflamed, painful eye in the ED. Take it slow, this figure and box dense material can be an eye sore when read.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Ocular pathology represent, for some, the most frightening diseases out there. And while the vast majority of cases that you will see in the ED will not be vision-threatening, you have to keep your eyes peeled. This episode of CRACKCast reviews Chapter 19 in Rosen’s 9th Edition – Red and Painful Eye. We will cover all of the pertinent information to best equip you for your next ED shift. We will start by giving you a solid approach to the history and physical examination for the patient complaining of having an angry peeper. Then, we will give you a solid differential to consider for patients with ocular complaints. Last, we will share some short snappers to look like a rockstar during your next consultation with your friendly neighbourhood Ophthalmologist.
So, sit back, take a sip of your coffee, and jump on in. This is a bit of a long one, so don’t be afraid to take it in chunks. As always, be sure to use this as an adjunct for your learning. Reference the text, run through the flashcards, listen to the podcast, rinse, and repeat. Spaced repetition is key!
[bg_faq_end]Core Questions:
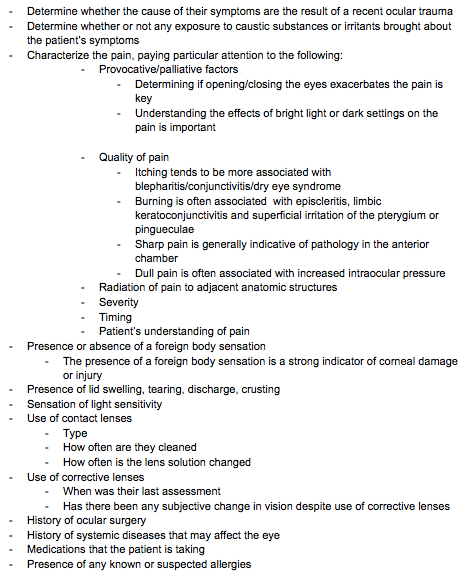
[bg_faq_start][1] Detail the pertinent points to review when taking the history of a patient presenting with a red and painful eye [Box 19.2]
Of course, everyone will have their own approach to taking a clinical history to elucidate the cause of the patient’s red and painful eye. However, it is important that everyone do their best to clarify the following points:
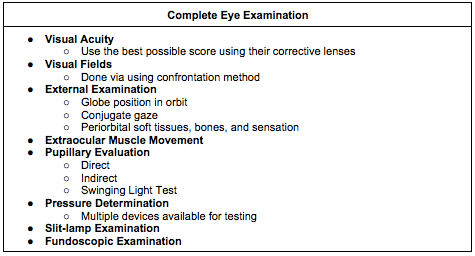
[2] Outline an approach to the ocular physical examination [Box 19.3]
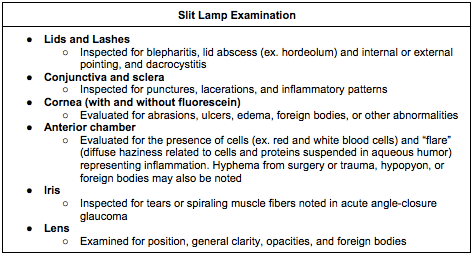
[3] Outline the components of the slit lamp examination [Box 19.4]
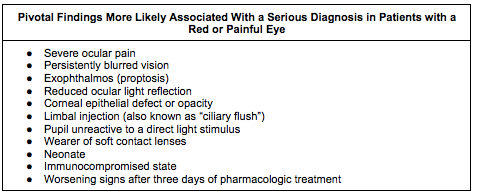
[4] What signs and symptoms, if present, likely indicate the presence of serious ocular pathologies [Box 19.1]
[5] What is a relative afferent pupillary defect and what conditions cause it?
Ahhh, the RAPD. A physical examination finding that pops up on every medical school, in-training, and Royal College answer sheet from time to time. And while we often continually review it, its definition and associated conditions often elude us come test time. So, review this often and take time to truly scrutinize the physiology here so this important concept solidifies in your mind.
A relative afferent pupillary defect, or RAPD, is defined as a pathologic dilation of both eyes when a bright light is swung from the patient’s normal eye to affected eye.
Let’s break it down here. A RAPD indicates a pathology in the afferent pathways that allow for consensual pupillary restriction to take place. So, information, at least in part, is not being transmitted along the afferent pathway of one eye. So, when you shine a light in the affected eye, there will be some degree of consensual constriction of both pupils. When you then swing the light to the unaffected eye, the pupils will restrict to an even greater degree, as there is no impediment to the neural impulses along that tract. When you then swing the light back to the affected eye, the eyes will actually dilate, as the stimuli that result in consensual reaction are running along a flawed neural pathway.
Some conditions that can cause a RAPD are the following:
- Vitreous hemorrhage
- Retinal detachment
- Retinal ischemia
- Optic neuritis
[6] List ten causes of increase intraocular pressure
This in no way is a comprehensive list, but should give you some accolades on your next off-service ophthalmology rotation:
- Acute angle-closure glaucoma
- Open-angle glaucoma
- Vitreous hemorrhage
- Orbital cellulitis/abscess
- Retrobulbar hemorrhage
- Hyphema
- Iritis with hypopyon
- Chronic steroid eye drop use
- Enopthalmitis
- Incorrect measurement technique
- Ocular malignancy
- Vomiting
- Ocular trauma
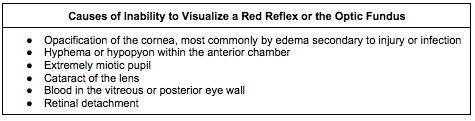
[7] List five causes for an absent red reflex [Box 19.5]
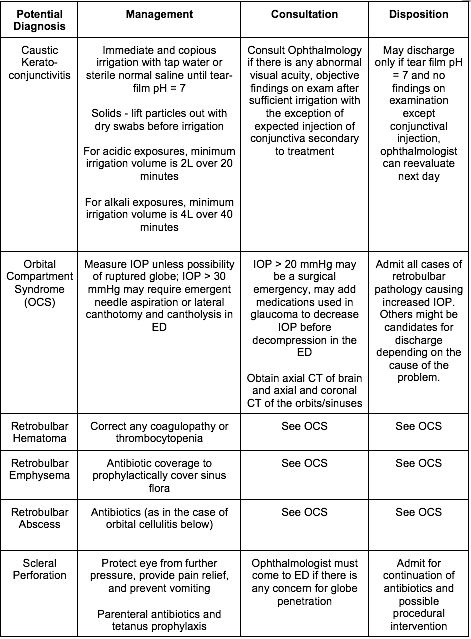
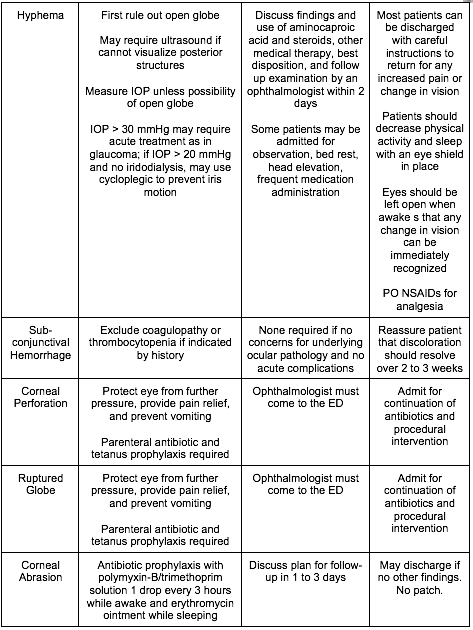
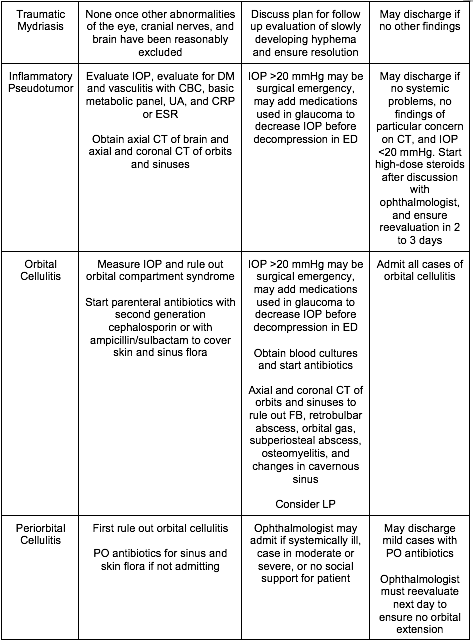
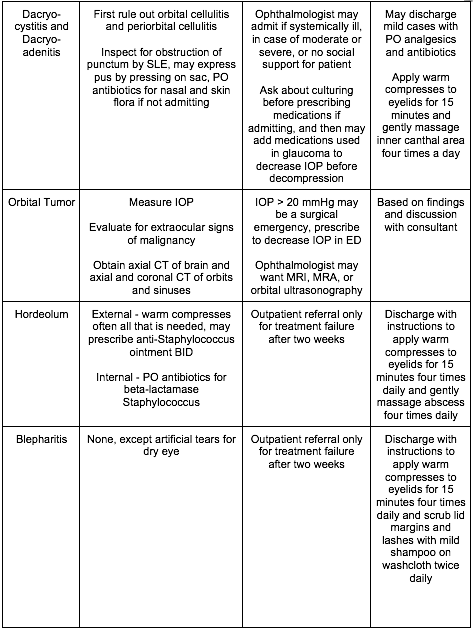
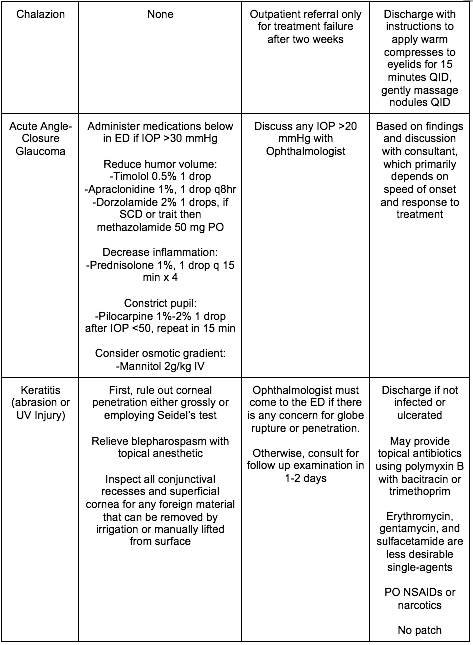
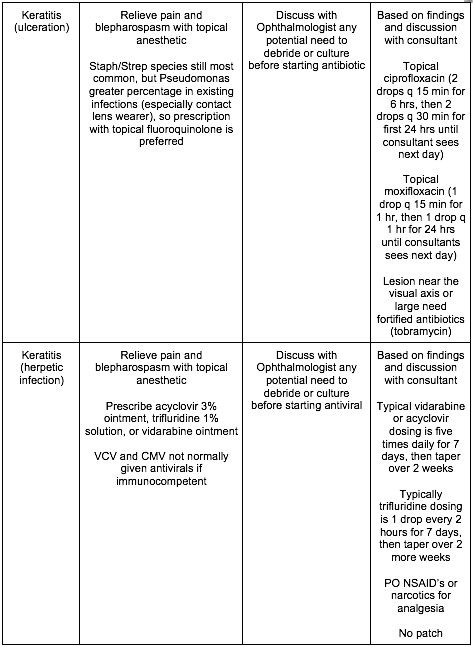
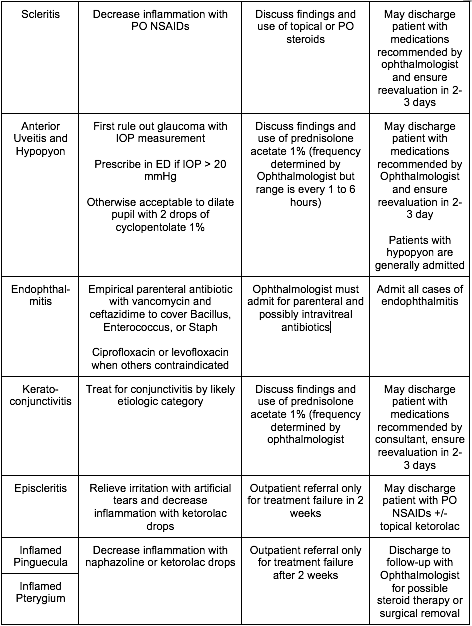
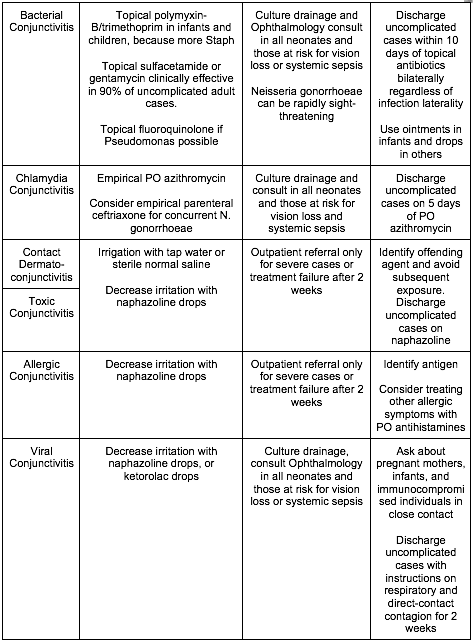
[8] Name three critical, emergent, urgent, and non-urgent causes of the red and painful eye and describe their treatment? [Figure 19.8]
WiseCracks:
[bg_faq_start][1] What are the fundoscopic findings of a central retinal artery occlusion?
Remember, think of a central retinal artery occlusion (CRAO) in the patient with painless acute onset vision loss. On fundoscopic exam, look for the following:
- General pallor of the retina
- Attenuation of the retinal arteries
- Attenuation of the retinal veins
[2] What is the pinhole test and what visual disturbances does it correct?
The pinhole test is a commonly-employed exam technique that is used by ophthalmologists to eliminate the influence of refractive errors that result in visual disturbances. By making the patient look through several small holes poked through a piece of paper, only light beams that enter the lens perpendicularly are allowed to pass. Thus, the influence of refractive errors are eliminated.
If the patient’s visual acuity does not improve with the pinhole test, they have a non-refractive visual deficit, and as such, you should do additional testing. If it corrects, your patient may just need a set of coke bottle glasses!
[3] What are the three most common causes of an irregularly shaped pupil?
- Blunt or penetrating trauma
- Previous surgery
- Synechiae from prior iritis or other inflammatory conditions
[4] What is Seidel’s Test and what condition does it identify?
Seidel’s Test is a non-invasive way to determine if there has been a corneal perforation. After instillation of the fluorescein dye, look at the patient’s eye under the cobalt blue light. If you see a waterfall-like flow from a portion on the cornea, the test is positive, indicating that aqueous humor is flowing through a corneal defect diluting and displacing the dye.
[bg_faq_end]Uploaded and copyedited by Ryan Fyfe-Brown



