This updated episode of CRACKCast covers Rosen’s Chapter 018, Diplopia (9th Ed.). This podcast will provide you with a simplified ED approach requiring half the thinking during the workup of double vision.
Shownotes – PDF here
[bg_faq_start]Rosen’s in Perspective
Welcome back to another episode of CRACKCast. Today, we will spare you the typical
introductory case as the content presented below is pretty dense. We will be reviewing a fairly
common problem in today’s podcast – diplopia. Interestingly, diplopia can have a myriad of
causes, and, when present, can be an indicator that something pretty serious is occurring in that
patient. We will go about giving you a good way to conceptualize diplopia and teach you what
you need to know to best interview, examine, and work up the next patient seeing double. So,
sit back, take a sip of your coffee, and enjoy the ride!
Core Questions:
[bg_faq_start][1] What is diplopia and how is it classified?
Diplopia, the perception of double vision, is classified in many ways. However, Rosen’s breaks it
down into two simple categories that will help you formulate your initial differential. It’s simple:
Monocular Diplopia
- Double vision that exists from dysfunction in one eye. Monocular diplopia persists even
when the unaffected eye is closed. - Monocular diplopia is an ophthalmologic issue, resulting from distortions in the path of
light through the eye or buckling of the retina itself.
Binocular Diplopia
- Double vision secondary to misalignment of the visual axes. Binocular diplopia abates
when either eye is closed - Binocular diplopia can arise from several problems:
- Mechanical orbitopathy
- Cranial Nerve palsy
- Proximal Neuraxial Process
- Systemic neuromuscular process
[2] What four questions help clinicians delineate the potential cause of a patient’s diplopia?
The history in a patient with diplopia is profoundly important, and in some cases, will be all you
need to make your diagnosis. During your next clinical interaction with a patient complaining of
double vision, ask yourself and the patient the following:
- What was the cadence of onset of symptoms?
a. Rapid onset, often with maximal symptoms immediately, often points to an
ischemic cause of the patient’s symptoms
b. Fluctuating diplopia may point to transient ischemia or neuromuscular
pathologies causing the patient’s symptoms - What is the directionality and orientation of diplopia and what aggravates it?
a. Defined as either vertical, horizontal, or torsional - Is there any associated pain with diplopia?
a. Points to potential inflammatory or infectious causes of the patient’s symptoms - Are there any systemic symptoms other than diplopia that are present?
a. May lead you to a diagnosis of a systemic illness causing diplopia
[3] What are the cardinal directions of gaze and how are they tested?
We are going to take you back in time to the clinical examination course in medical school for
this question.
There are six cardinal movements of gaze. Each cardinal direction marks the point at which the
extraocular muscle and the nerve supplying it have their maximal effect. When visualizing it,
think of a six-spoke asterix or an “H” pattern. Each corner of the asterix or “H” denotes one of
the cardinal directions of gaze. The following table should help you think about it a bit better:

Now, we are humble practitioners of Emergency Medicine here on CRACKCast, so to simplify
things, you can think about it this way:
- Every extraocular movement is controlled by CN III (oculomotor nerve) EXCEPT for
looking toward the temple (CN VI or the abducens nerve) or at the tip of the nose (CN IV
or the trochlear nerve)
[4] Outline the physical exam for the patient with monocular and binocular diplopia.
So, let’s break it down. Here is our approach to the physical examination for the patient seeing double.
Monocular Diplopia
Remember, this is exclusively a problem of the eye itself. So, you are going to do a thorough ophthalmologic examination including:
- Visual acuity
- Cardinal directions of gaze
- Peripheral field testing
- Intraocular pressure testing
- Pupillary examination
- Direct response
- Consensual response
- Swinging light test
- Fundoscopy
- Slit Lamp Exam
Binocular Diplopia
Now things get a little more complex, but if you think about the four mechanisms that cause binocular diplopia, things get a little easier
Remember, binocular diplopia can be caused by:
- Mechanical orbitopathies
- Cranial nerve palsies
- Neuraxial lesions
- Systemic processes
Knowing this, we here at CRACKCast recommend the following:
Detailing neurologic examination, evaluating
- Cranial nerve testing
- Cerebellar testing
- Examination of the motor system
- Examination of sensation
- Reflex testing
- Head and neck examination
[5] Outline the DDx for monocular diplopia?
While not an all-inclusive list, the following is a good DDx for monocular diplopia:
- Keratoconjunctivitis sicca
- Corneal abrasions/defects
- Cataracts
- Lens dislocation
- Macular Disruption
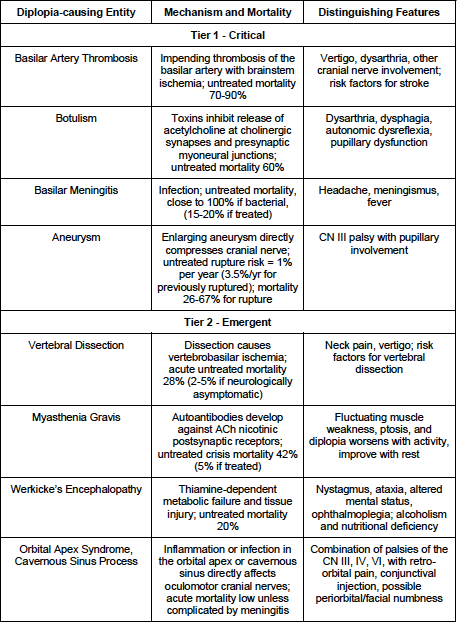
[6] Outline the DDx for binocular diplopia? [Table 18.1]
While not an all-inclusive list, the following is a good DDx for monocular diplopia:
The following is taken from Rosen’s 9th Edition. Please see the text for a more complete table.
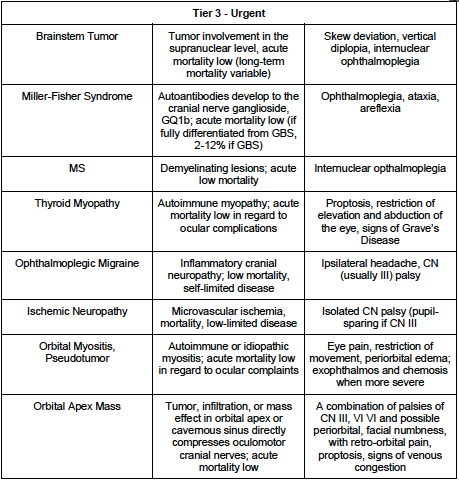
[7] Detail the different oculomotor palsies. [Figure 18.3]
This table was adapted from Figure 18.3 in Rosen’s 9th Edition. Please see the textbook for the
accompanying images.

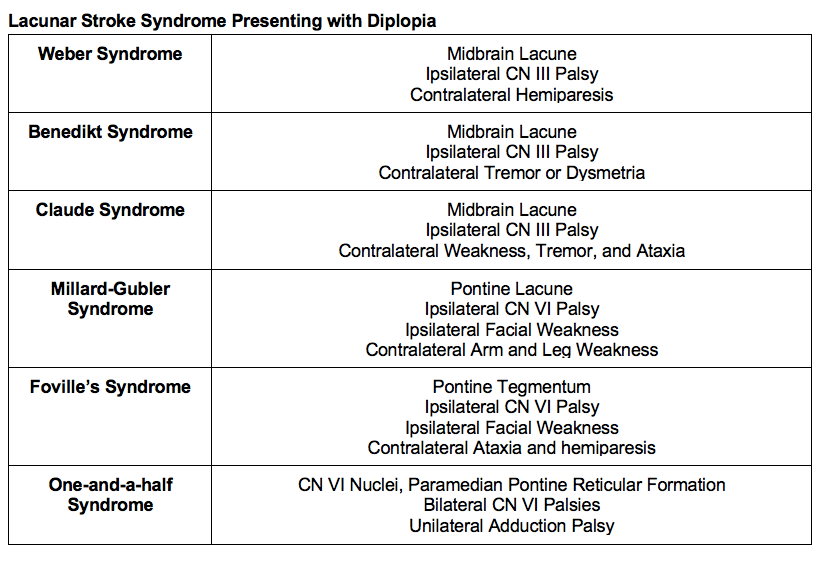
[8] Detail the various lacunar stroke syndromes. [Box 18.1]
This is a box, folks. Strap in for some intense neurology learning!
This table is adapted from Box 18.1 in Rosen’s 9th Edition. Please reference the textbook for
more information.
[9] Define internuclear ophthalmoplegia.
As per Rosen’s 9th Edition:
An internuclear ophthalmoplegia is defined as having an inability to adduct the eye on one side
in the contralateral direction during lateral gaze that resolves during convergence, implicates a
lesion in the medial longitudinal fasciculus.
This physical examination finding is typically seen in patients with multiple sclerosis. The long
and short of it is, the affected eye is unable to adduct when looking to the side opposite it (i.e.,
one cannot adduct the right eye when following the examiners finger laterally to the left, and
vice versa).
[10] What ancillary tests are required for the patient presenting with diplopia? [Figure 18.4]
Ancillary tests ordered are largely dependent on whether or not the patient has monocular or
binocular diplopia.
In patients with monocular diplopia, you may not need ANY ancillary testing. If present, they will
likely simply need a referral to your friendly neighbourhood Ophthalmologist.
Rosen’s 9th Edition has a pretty tight diagnostic algorithm for patients with diplopia presenting to
the ED (reference the textbook for the original figure), but it basically states the following:
- For patient with a suspected restrictive mechanical
orbitopathy:
- Get a contrast-enhanced CT or MRI of the orbits
- For patients with isolated nerve palsies:
- If they have typical microvascular ischemia CN III palsy (sparing of the pupil, Hx DM/HTN, no other focal neurological deficits), you can consider discharge with referral to neuro-Ophthalmology
- If they have exam features not consistent with CN III palsy or other oculomotor cranial nerve palsies, MRI/CT of the brain
- For patients with multiple CN palsies of the
III/IV/VI:
- Get a contrast-enhanced CT or MRI of the brain/orbits
- For patients with diplopia and other neurologic
deficits confined to the brainstem:
- Get a MRI/MRA brain or CT/CTA brain and neck
- Consider LP for meningitis
- For patients with neurologic deficits consistent
with neuropathic syndrome with brainstem and cranial nerve involvement:
- Treat empirically for the suspected entity (e.g., botulism, Wernicke’s, Miller Fisher Syndrome (MFS))
- Consider screening MRI
- Consider LP for MFS
- For patients with symptoms consistent with a
neuromuscular disorder:
- Perform the ice test or Tensilon test
WiseCracks:
[bg_faq_start][1] What are the most common oculomotor palsies and what causes them?
Answer:
The most common oculomotor nerve palsy is CN VI (abducens nerve). Second is CN III
(oculomotor nerve). Third most commonly affected oculomotor nerve palsy is CN IV (trochlear
nerve).
CN VI is most commonly affected by tumors, elevated ICP, and microvascular ischemia. It’s
particularly long course makes it vulnerable to damage.
CN III is most commonly affected by diabetic or hypertensive vasculopathies as well as
aneurysms of the posterior communicating, basilar, superior cerebellar, posterior cerebral, and
cavernous internal carotid arteries.
CN IV is most commonly affected by trauma abutting against the tentorium and vascular
causes.
[2] What is orbital apex syndrome?
Answer:
Orbital Apex Syndrome is a poorly-defined term, but generally refers to a constellation of
multiple oculomotor nerve palsies, diminished vision, and inflammation caused by masses
and/or venous congestion in the ocular apex or cavernous sinus
[3] What is the “rule of the pupil” and how reliable is it?
Answer:
According to Rosen’s 9th Edition, the rule of the pupil states that in the patient with an otherwise
complete CN III palsy (complete ptosis, completely down-and-out orientation of the afflicted
eye), if the pupil has normal size and reactivity, there is no compressive source (e.g., expanding
aneurysm) of the nerve palsy.
This being said, this is more of a guideline, because clinical medicine is never perfect. You
cannot use this to “rule in” a compressive cause of a neuropathy. Up to 50% of patients with
diabetic or hypertensive microvascular ischemia will have will have pupillary involvement. This is
thought to be because these patients have some degree of autonomic neuropathy.
[4] Detail the physical exam maneuvers used to identify patients with
myasthenia gravis.
Answer:
- Fatigability of Upward Gaze
a. First, the patient is to maximally close their eyes and hold it for 5-10 seconds.
Then, have the patient fix their gaze upward at your finger and hold it there. The
patient’s degree of ptosis will worsen if the test is positive.
b. 80% Sensitive
c. 63% Specific - Ice Test
a. Based on the fact that neuromuscular transmission occurs faster at lower
temperatures
b. As per UpToDate:
i. In the ice pack test, a bag (or surgical glove) is filled with ice and placed
on the closed lid for two minutes. The ice is then removed and the extent
of ptosis is immediately assessed. Improvement in ptosis is a positive test
result (defined by a > 2mm improvement in palpebral opening). Make
sure to provide forehead pressure to prevent contribution from the
frontalis muscle.
c. 80% Sensitive
d. 25% Specific
Uploaded and copyedited by Chloe LaBrie and Ryan Fyfe-Brown



