This updated episode of CRACKCast covers Rosen’s Chapter 014, Confusion (9th Ed.). Confusion is a symptom experience by all at some point or another. Confusion has a spectrum of severity and in the Emergency Department it is associated with high rates of mortality. This podcast will give you the tools to identify the cause of your patient’s alteration and help guide your management.
Shownotes – PDF here
[bg_faq_start]Rosen’s in Perspective
This episode is all about confusion. This is an acute alteration in higher cortical functions (memory, attention, or awareness). Remember to differentiate from coma (unrousable) and stupor (drowsy but rousable) – see our last episode for everything you ever wanted to know about altered LOC. Confusion is a symptom (like dyspnea, chest pain, etc) that can have a spectrum of severity – this ranges from mild short term memory difficulty to complete inability to relate to the environment, AKA delirium. There is evidence that we are not particularly great at diagnosing delirium in the ED. Delirium is essentially acute brain failure, and has significant effects on mortality and morbidity.
[bg_faq_end]Core Questions:
[bg_faq_start][1] Define confusion.
Per Rosens:
“The term confusion connotes an acute alteration in higher cerebral functions, such as memory, attention, or awareness. The ability to sustain and focus attention is impaired.”
[2] What is your differential diagnosis for the confused patient?
Critical
- Failure to oxygenate
- Failure to ventilate
- Hypoglycemia
- Elevated intracranial pressure with impending herniation
Emergent
- Systemic diseases
- Electrolyte and fluid disturbance
- Endocrine disease—thyroid, adrenal
[3] Differentiate between organic and functional causes of confusion. (See Table 14.1)
Organic
- History
- Acute onset
- Any Age
- MSE
- Fluctuating level of consciousness
- Disoriented
- Attention disturbances
- Poor recent memory
- Hallucinations – visual, tactile, auditory
- Cognitive changes
- Physical Examination
- Abnormal vital signs
- Nystagmus
- Focal neurological signs
- Signs of trauma
Functional
- History
- Onset over weeks to months
- Onset age; 12-40 years
- MSE
- Alert
- Oriented
- Agitated, anxious
- Poor immediate memory
- Hallucinations, usually auditory
- Delusions, illusions
- Physical Examination
- Normal vital signs
- No Nystagmus
- Purposeful movement
- No signs of trauma
[4] What is the Quick Confusion Scale (QCS) and how is it calculated? (See Figure 14.2)
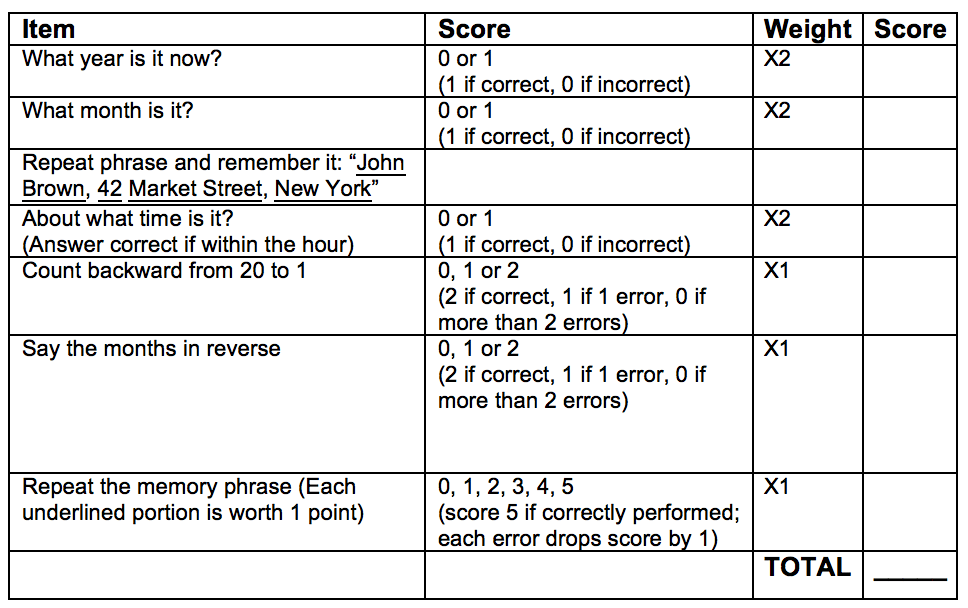
The final score is the sum of the totals. A score less than 15 indicates altered cognition and need for further evaluation.
[5] What is the Brief Confusion Assessment Method (bCAM) and how is it used? (See Figure 14.4)
bCAM differs from CAM in that the bCAM allows for early stoppage for positive features. The content of the rule is more or less the same. Memory aid – think AIDS –
• Acute onset and fluctuating course
• Inattention (months backwards)
• Disorganized thinking (will a stone float on water)
• Sensorium altered/altered LOC (GCS)
CAM/bCAM positive if Feature 1 and 2 plus either 3 or 4 present
[6] What is the Mini-Mental State Examination (MMSE) and how is it scored?
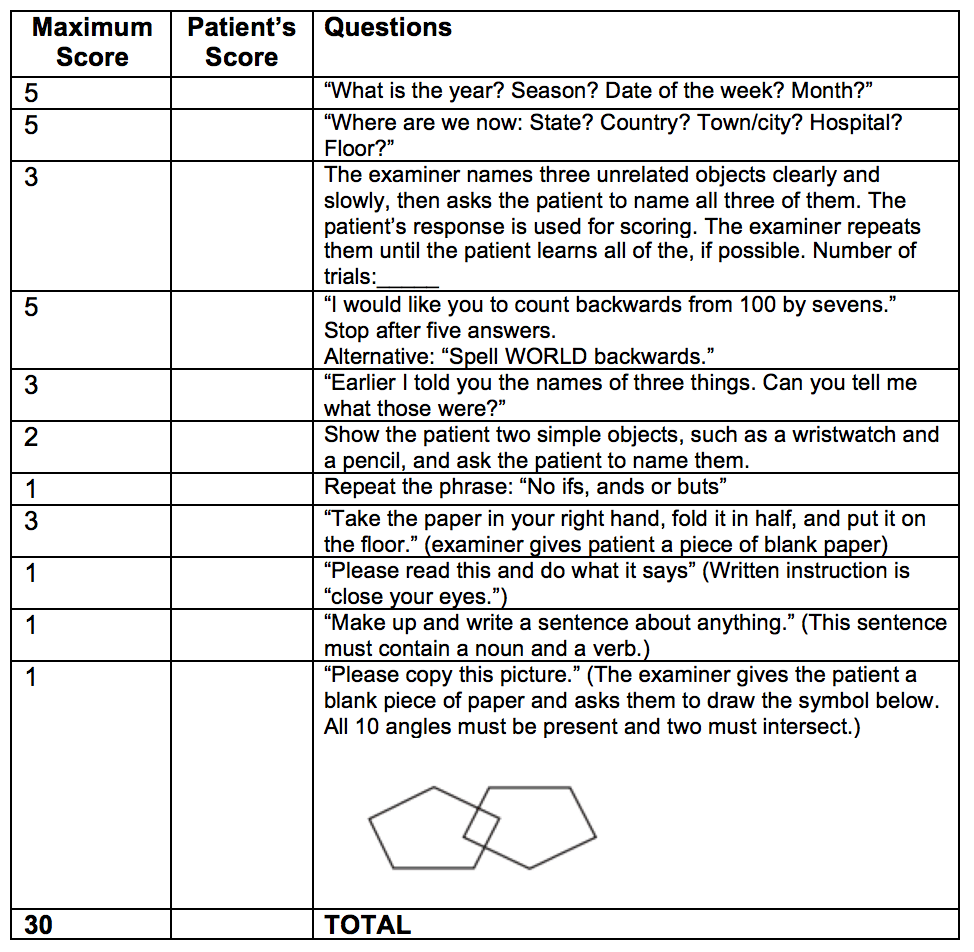
In general – score ≤ 23 = cognitive impairment – however adjustments can be made for age, education level, etc.
[7] What ancillary tests are used when working up the confused patient?
- Full set of vitals
- Don’t forget bedside glucose
- Further testing as directed by
history and physical
- Concern for infection – septic workup
- CBC, Electrolytes, and renal function
- VBG
- Liver function and liver enzymes
- TSH
- Cardiac enzymes and ECG
- Tox assays, co-oximetry if suspicion for ingestions/CO/intoxication
- CT head if concern for trauma, localizing deficit, mass, etc.
- LP in certain circumstances (eg negative workup with persistently altered LOC, concern for SAH, meningitis, encephalitis etc).
- ± inpatient MRI…
[8] What is the role of thiamine in the treatment of the acutely confused patient?
Quick summary from UpToDate…
- Wernicke’s encephalopathy is difficult to diagnose
- Untreated – most patients progress to coma and death (or Korsakoff’s)
- Thiamine is a safe and inexpensive antidote. (extremely rare AE’s include bronchospasm and anaphylaxis).
- Thiamine dosing tips
- parenteral preferable to oral (more consistent absorption)
- Dose 500mg IV TID x 2 days then 250mg IM daily x 5 days
- Administration of glucose without thiamine can precipitate or worsen WE – so give thiamine before glucose.
The first sign of improvement with thiamine is resolution of ocular signs over hours to days. Gait ataxia resolves typically along with vestibular dysfunction. Confusion resolves over days to weeks.
[bg_faq_end]WiseCracks:
[bg_faq_start][1] What simple tests can you use to assess concentration at the bedside?
While assessment of confusion or delirium can take up a decent portion of your clinical encounter, you can assess concentration (and thus do a quick screen for confusion) relatively quickly. So, next time you have your next patient that is suspected of being confused, consider asking the following:
- Repeat digits forward and backward
- The patient should be able to
repeat 5-6 digits forward (e.g., “repeat the following digits in the order that
I have given them to you: 1,2,3,4,5,6)
- The patient should be able to repeat 4 digits backward (e.g., “Now, repeat the last four numbers I gave you in reverse order: 4,3,2,1)
- Listing the months in reverse order OR spell a commonly used backward
- A patient who can sustain concentration should be able to do this with relative ease
[2] What treatments should be used for the patient with acute hypoglycemia causing confusion?
Sugar!
1 amp D50 IV with consideration for dextrose infusion if persistently low BGMs/rebound hypoglycemia.
Give thiamine at time of glucose administration in the appropriate clinical context.
Feed them when awake (complex carbohydrates and all that good stuff).
[3] List 5 emergent and 4 critical diagnoses that cause confusion.
Critical
- Failure to oxygenate
- Failure to ventilate
- Hypoglycemia
- Elevated ICP with impending herniation
Emergent
- Toxic ingestion/Substance withdrawal
- Infection (esp. meningitis/encephalitis)
- Hypo/hyper calcemia, hepatic encephalopathy, uremia, etc.
- Endocrine disease (thyroid/adrenal)
Structural brain lesion (stroke/bleed/mass)
[bg_faq_end]Uploaded and copyedited by Chloe Labrie.