This episode of CRACKCast covers Chapter 193 in Rosen’s Emergency Medicine (9th Ed.) – Weapons of Mass Destruction. Although attacks involving WMD’s are relatively uncommon, being thoroughly prepared for these events will prove invaluable for the community affected. Sit tight and listen in to make sure you are ready if the unthinkable should happen.
Shownotes – PDF here
[bg_faq_start]Key concepts
- Emergency department (ED) preparedness for a radiation incident should address decontamination (an external freestanding decontamination unit is best), triage, staff safety, personal protective equipment (PPE), and diagnostic procedures that emphasize radiation monitoring. It is important that emergency personnel know their radiation safety officer.
- Management of acute life-threatening conditions takes priority over radiation-associated issues.
- Aerosol dispersal is a likely route that terrorists may use to deploy biologic weapons, so victims will present primarily with respiratory complaints.
- In addition to “flulike” symptoms, anthrax typically causes mediastinal widening, pulmonary consolidation, and pleural effusions best seen on chest computed tomography (CT) scans.
- Smallpox can spread in a hospital environment; thus, patients thought to have smallpox should be admitted to locations separated from the rest of the hospital.
- Decontamination is a key activity in the management of patients exposed to chemical agents, and hospitals should provide this intervention.
- Nerve agents are organophosphates, and patients exposed to these agents are treated with large doses of atropine (repeated frequently), pralidoxime, and benzodiazepines.
Rosen’s in perspective
Besides managing the injuries and illnesses from common disasters such as earthquakes and airplane crashes, emergency clinicians should also have competence in treating victims generated by terrorist attacks with nuclear, biologic, chemical, or high-energy explosive weapons.
The military uses the acronym CBRNE, pronounced “see-burn-ee,” referring to chemical, biological, radiological, nuclear, and explosive agents.
This chapter uses weapons of mass destruction (WMD) because of its wide acceptance and familiarity. – Rosen’s 9th ed., Ch 193
[bg_faq_end]Core questions
[bg_faq_start][1] List 6 potential agents that may be used as weapons of mass destruction
- See Rosen’s box 193.1 for original
- Potential agents of high concern for use as weapons of mass destruction
- Chemical
- Nerve agents: sarin, soman, tabun, VX
- Mustard agent
- Biologic
- Anthrax
- Plague
- Smallpox
- Botulism
- Viral haemorrhagic fever
- Tularaemia
- Radiologic
- Simple device
- Dispersal device
- The CDC lists Category A (high threat) agents:
- anthrax [Bacillus anthracis],
- botulism [Clostridium botulinum toxin],
- plague [Yersina pestis],
- smallpox [variola major],
- Tularemia [Francisella tularensis],
- viral hemorrhagic fevers [filoviruses (eg, Ebola, Marbug)]
- arenaviruses [eg, Lassa, Machupo]),
- Chemical
[2] List 6 features of weapons of mass destruction threats that make them unique
- See Rosen’s box 193.2 for original
- Fear of unknown or unfamiliar
- Lack of training for hospital personnel
- Lack of equipment, including personal protective equipment (PPE) and diagnostic aids
- Potential for mass casualties
- Psychological casualties
- Crime scene requiring evidence collection and interaction with law enforcement
- Potential for ongoing morbidity and mortality (dynamic situation)
- Others
- Public doesn’t know
- Professional don’t know
- No resources
- Huge numbers
- Psychological stress
- Massive uncontainable crime scene
- Ongoing damage and dynamic destruction
[3] Describe 6 signs suggesting biologic weapon deployment
- By convention, biological weapons are divided into three groups: bacteria, viruses, and toxins.
- A characteristic shared by these agents is their ability to be dispersed as an aerosol. Because this is the most effective means to expose a large population, aerosol dispersal is the route for most WMD.
- Patients exposed to biologic agents usually present with vague symptoms associated with an influenza-like illnesses. (typically out of the normal flu season).
- See Rosen’s box 193.3 for original
- Syndromes
- Pulmonary symptoms, pneumonia
- Rashes
- Sepsis syndrome
- Influenza symptoms
- Epidemiology
- Multiple, simultaneous events
- Dead animals
- Large numbers of patients with high toxicity and death rate
- Clusters of patients with pulmonary or dermatologic syndromes
- Syndromes
[4] What are recommendations for prevention of In-Hospital Transmission of Contagious Agents
- Ensure ample hospital notification that a suspected case is arriving
- Recommendations for prevention of in-hospital transmission of contagious agents (see Box 193.4 for original)
- Isolate patient in single room with adjoining anteroom
- Have handwashing facilities and personal protective equipment (PPE) available in anteroom
- Use negative air pressure if possible
- Use strict barrier precautions: PPE, gowns, globes, high-efficiency particulate air (HEPA) filter respirators, shoe covers, protective eyewear
- Alert hospital departments that generate aerosols: laboratory centrifuges, pathology autopsies
[5] Describe the 2 typical presentations of Anthrax. What are typical CXR findings? How is each type of anthrax treated?
Bacillus anthracis, a gram-positive spore-forming bacterium, is the causative agent of anthrax (“woolsorter’s disease”).
The spores are extremely hardy and can survive for years in the environment. The disease is caused by exposure to the spores, not the bacilli in their vegetative state. It is normally a disease of sheep, cattle, and horses and is rarely seen in developed countries because of animal and human vaccination programs.
Disease in humans can occur when spores are inhaled, ingested, or inoculated into the skin. The spores germinate into bacilli inside macrophages. The bacteria then produce disease by releasing toxins (eg, protective antigen, edema factor, and lethal factor) that cause edema and cell death.
- The forms (both are CLINICAL diagnoses)
- Inhalational form – most lethal
- Spores get into the lungs
- After phagocytosis by macrophages, the spores germinate and are transported to the tracheobronchial lymph nodes, where the bacteria multiply.
- During the next 2 to 10 days, patients have an influenza-like illness, with malaise, fever, and nonproductive cough. This initial phase can be delayed for more than 1 month in some patients. Within 24 to 48 hours, abrupt deterioration occurs, with overwhelming sepsis, shock, hemorrhagic mediastinitis, dyspnea, and stridor.
- A chest radiograph obtained at this time may show a widened mediastinum and hilar adenopathy, but typical radiographic findings are not dramatic and could be missed (presenting as a pulmonary consolidation or effusion).
- Death usually results within 3 days, and 50% of patients have hemorrhagic meningitis. Human-to-human transmission has not been reported with inhalational anthrax.
- Treatment
- IV antibiotics
- Anthrax immunoglobulin
- Antibody based therapies with raxiacumab
- Cutaneous form
- Spores introduced into the skin (patients already have open wounds or abrasions)
- After an incubation period of 1 to 5 days, a papule develops, progressing to form a large vesicle during the next several days. Severe edema occurs around the lesion and is associated with regional lymphadenitis. The lesions are not tender, and the patient may or may not be febrile. After approximately 1 week, the lesion ruptures, forming a black eschar (thus the name anthrax, from the Greek word for “coal”).
- In the next 2 or 3 weeks, either the eschar sloughs off and the illness is over or the organism disseminates and the patient dies. Antibiotics do not affect the course of local disease but are used to prevent dissemination and death.
- TREATMENT = PO antibiotics
- Gastrointestinal (mesenteric lymphadenitis) and oropharyngeal (cervical lymphadenitis) forms also exist.
- Inhalational form – most lethal
A few important points:
- These consensus recommendations include fluoroquinolones and tetracycline for all children, regardless of age. Balancing the potential risks of such drugs against the consequences of infection by drug-resistant anthrax strains, the benefits justify the recommendations. Nontoxic victims with cutaneous anthrax can be treated as outpatients with oral ciprofloxacin or doxycycline for 7 to 10 days.
- Victims with inhalational, cutaneous, or gastrointestinal disease and toxicity require intravenous therapy with ciprofloxacin or doxycycline plus at least one other antibiotic (eg, linezolid, clindamycin, or an aminoglycoside) that inhibits protein synthesis. If meningitis is present, a third antibiotic is added that can penetrate the central nervous system (meropenem).
- Treatment is to continue for 60 days or until the patient has received three doses of the anthrax vaccine, given on days 0, 14, and 28. The complete vaccine course requires 18 months.
For postexposure prophylaxis, oral ciprofloxacin (500 mg) or doxycycline (100 mg) twice a day is recommended. Amoxicillin can be substituted if sensitive strains are identified. Antibiotic prophylaxis is to continue for 60 days or until patients have received at least three doses of the vaccine.
See also Box 193.5 – Treatment of Anthrax
- Cutaneous Anthrax Without Toxicity
- Adults
- Ciprofloxacin, 500 mg PO bid; or doxycycline, 100 mg PO bid; oramoxicillin, 500 mg PO tid
- Children
- Ciprofloxacin, 20 to 30 mg/kg/day PO divided bid (maximum 1 g); ordoxycycline, 4.4 mg/kg/day PO divided bid (maximum 200 mg); or amoxicillin, 20 to 40 mg/kg/day PO divided tid (maximum 1500 mg)
- All doses are given for 7 to 10 days.
- Adults
- Inhalational, Cutaneous, or Gastrointestinal Anthrax with toxicity
- For adults and children, consider the antibody-based therapies raxibacumab and anthrax immune globulin in addition to IV antibiotics.
- Adults
- Ciprofloxacin, 400 mg IV every 12 hours; ordoxycycline, 100 mg IV every 12 hours; or penicillin G, 4 million units IV every 4 hours
- For patients without meningitis, add a second drug that inhibits protein synthesis, such as linezolid or clindamycin. For patients with meningitis, add a third drug to this regimen that penetrates the CNS, such as meropenem.
- Children
- Ciprofloxacin, 20 mg/kg/day IV divided every 12 hours (maximum 800 mg); or doxycycline, 4.4 mg/kg/day IV divided every 12 hours (maximum 200 mg); orpenicillin G, 250,000 to 400,000 units/kg/day IV divided every 4 hours (maximum 24 million units)
- For patients without meningitis, add second drug that inhibits protein synthesis, such as linezolid or clindamycin. For patients with meningitis, add a third drug to this regimen that penetrates the CNS, such as meropenem.
- All doses are given until toxicity resolves, then switch to oral form. Treat for 60 days or until the patient receives three doses of vaccine.
- Postexposure Prophylaxis
- The same drugs and dosage are prescribed as for cutaneous anthrax without toxicity. Treat for 60 days or until the patient receives three doses of vaccine.
Sputum culture, Gram’s stain, and blood cultures are not helpful until late in the course of the disease. Tests to confirm the diagnosis of inhalational anthrax include the polymerase chain reaction for identification of anthrax markers in pleural fluid, serologic detection of immunoglobulin to protective antigen, and immunohistochemical testing of biopsy specimens. [Rosen’s 9th Ed, Ch 193]
[6] How is the plague transmitted? What are the 2 typical presentations of the plague? How is each treated?
- Inhalational, Cutaneous, or Gastrointestinal Anthrax with toxicity
- For adults and children, consider the antibody-based therapies raxibacumab and anthrax immune globulin in addition to IV antibiotics.
- Adults
- Transmitted via
- Plague is caused by Yersinia pestis, a gram-negative bacillus. It is normally a disease of rodents that is transmitted to humans through the bite of an infected flea or by inhalation.
- The bacteria do not form spores and die rapidly in the environment. However, they are viable for days in dry sputum, flea feces, and human remains. Dogs are relatively resistant to infection, but cats are highly susceptible and could form a reservoir for maintaining the disease in a human population. Recovery is followed by temporary immunity.
- Presentations: classic presentation = fulminant gram -ve pneumonia with massive hemoptysis
- Three forms of the disease exist: pneumonic, bubonic, and septicemic plague.
- All three forms require antibiotics: Just think “CDC”
- Ciprofloxacin
- Doxycycline
- Chloramphenicol
- Even children get all these drugs despite the usual hesitation to traditionally give kids cipro (risk of arthro and chondrotoxicity) and doxy (risk of yellow tooth discolouration and dental enamel hypoplasia.)
- The two typical presentations of the plague
- Primary pneumonic plague: bacilli inhaled into the lungs through an aerosolized biological WMD
- After an incubation period of 2 or 3 days, victims have sudden onset of fever, chills, and an influenza-like illness. This is followed within 24 hours by a fulminant pneumonia associated with hemoptysis, systemic toxicity, respiratory failure, circulatory collapse, and death. The pneumonia is classically lobar, but any x-ray pattern is possible, including acute respiratory distress syndrome. Six percent to 10% of victims have plague meningitis. Coagulation abnormalities and hepatocellular injury occur. The coagulopathy is characterized by ecchymoses, disseminated intravascular coagulation, and acral gangrene (“black death”). The gangrene is caused by bacterial production of the coagulase enzyme in areas of the body where the temperature drops below 98.6° F (37° C). This induces blood to clot in fingers, toes, and the nose, with resultant infarction and gangrene. If the victims survive, long-term rehabilitation is required. Pneumonic plague is transmissible human to human.
- Require full respiratory isolation
- Treatment
- IV “CDC” drugs
- Add streptomycin and gentamicin
- Bubonic plague: Yersinia pestis is inoculated into the skin from a FLEA BITE
- In 2-3 days they migrate to a LYMPH NODE
- Cause massive regional lymphadenopathy, tenderness, NECROSIS
- These are the large, tender nodes. AKA: BUBOES
- Groin, axilla, cervical
- Systemic symptoms- fevers, chills, weakness, toxicity.
- I+D is not recommended.
- These people can develop septicemic plague or secondary pnuemonic plague
- Shock, DIC, coma, death.
- Direct human-to-human transmission does not occur with bubonic or septicemic plague. However, both of these conditions can lead to secondary pneumonic plague, which is communicable. Therefore, initial isolation (for the first 48 hours) is recommended for all patients with plague.
- Prophylaxis
- The mainstay of prophylaxis against plague remains oral antibiotics. A vaccine exists but has no value in an acute outbreak. It is effective only against bubonic disease and takes several months to impart immunity. The drugs for prophylaxis are tetracycline, doxycycline, ciprofloxacin, chloramphenicol, and possibly trimethoprim-sulfamethoxazole for children.
- See Box 193.6 for Treatment of Plague
- Parenteral Therapy
- Adults
- Streptomycin: Although streptomycin is recommended as first-line treatment, it may not be readily available.
- 1g IM bid
- Gentamicin, 5mg/kg once daily IM or IV
- Doxycycline, 100mg IV bid
- Ciprofloxacin, 400mg IV bid
- Chloramphenicol, 25mg/kg IV qid
- Children
- Streptomycin, 15mg/kg IM bid (maximum 2g/day)
- Gentamicin, 2.5mg/kg IM or IV tid
- Doxycycline, 2.2mg/kg IV bid (maximum 200mg/day)
- Ciprofloxacin, 15mg/kg IV bid (maximum 800mg/day)
- Chloramphenicol, 25mg/kg IV qid
- Pregnant Women
- Same as above but exclude streptomycin and chloramphenicol
- Oral Therapy
- Adults
- Doxycycline, 100mg bid
- Ciprofloxacin, 500mg bid
- Chloramphenicol, 25mg/kg qid
- Children
- Doxycycline, 2.2mg/kg bid (maximum 200mg/day)
- Ciprofloxacin, 20mg/kg bid (maximum 1g/day)
- Chloramphenicol, 25mg/kg qid
- Pregnant Women
- Same as above but exclude chloramphenicol
- Adults
- Adults
- Parenteral Therapy
- Primary pneumonic plague: bacilli inhaled into the lungs through an aerosolized biological WMD
Wisecracks
[bg_faq_start][1] Why are children at higher risk of death from WMD?
- Children are particularly vulnerable to these weapons.
- They breathe at a faster rate than adults do, increasing their relative exposure to aerosolized agents.
- Some chemicals, such as sarin, are heavier than air, so they tend to accumulate at the level where children are more likely to inhale them. Children have a greater surface area–to–volume ratio and their skin is thinner. This makes them more susceptible to agents that act on or through the skin. They have smaller fluid reserves and higher metabolic rates.
- Therefore, they are more vulnerable to dehydration from vomiting and diarrhea and suffer increased toxicity from a given exposure, such as to radioactive iodine.
[2] What are components of ED preparedness for chemical weapons of mass destruction?
- See Rosen’s Box 193.7 for Emergency Department Preparedness for Chemical Weapons of Mass Destruction
- Community-based hospital planning
- Personnel trained in recognition, mass casualty triage, and treatment
- Decontamination facility with protocols (e.g. runoff water, warm water)
- Personal protective equipment (PPE) readily accessible and compliant with regulations
- Rapid access to antidotes, cyanide kits, and anticonvulsants
- Hospital incident management system in place
- Knowledge of how to access experts quickly
- Could think about this as an outside-in or extrinsic vs. intrinsic support you’d imagine needing for a big disaster.
- Planning
- Place
- Stuff
- Staff
[3] Describe a basic ER protocol for handling radiation exposure / casualties (review)
- Although Russia acknowledges that 50 to 100 of its 1-kiloton “suitcase” nuclear weapons are missing, the problems of purchasing, moving, and detonating these devices are formidable.
- Sabotage at nuclear power stations is possible, but given tight security, multiple safety systems, and thick concrete housings surrounding the reactors, the threat is probably low.
- Instead, simple radiologic devices, such as those used by hospitals for radiation therapy, are thought to be the source of choice.
- See Episode 146 for all the details, but in summary:
- Victims presenting to the ED will suffer from three types of exposure: irradiation, internal contamination, and external contamination.
- The external contamination type can be easily dealt with via external decontamination, the internal contamination is more difficult. Again any immediate life threats should be treated ASAP. (a patient in acute distress from a myocardial infarction or urosepsis would be triaged ahead of a radiation victim with stable vital signs, regardless of the dose received.)
- Hospitals should be prepared to decontaminate patients because historical data suggest that up to 80% of patients do not receive this intervention before arrival.
- Activate your local ER response plan and notify your administration
- Try and find who your radiation officer is
- All staff to wear PPE
- Regular gown, double gloves, mask, boots
- Decontamination warm zone – BEFORE ENTERING THE HOSPITAL!!!
- Remove all contaminated clothes, spray patients off, then wash with soap and water, place clothing in plastic bags
- Cover wounds with sterile dressings
- Patients should wear gowns and donne a surgical cap
- Watch for patients at risk for internal contamination:
- Internally contaminated patients present a therapeutic challenge because they have radioactive material inside their bodies (eg, lungs and gastrointestinal tract) or incorporated into their cells. They should be placed in an isolation room where all secretions and body fluids can be collected. Various medications are available for administration to internally contaminated patients and can limit uptake or facilitate removal of certain radioactive elements. These medications include Prussian blue (Radiogardase) for cesium and thallium ingestions and diethylenetriaminepentaacetic acid (DTPA) for plutonium exposure.
- Ideally all staff should be wearing dosimeters, which would be followed by the radiation officer
- Safety and quality review process after the incident
- Repeat training and disaster preparedness education
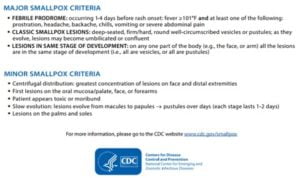
[4] Differentiate between chickenpox and smallpox
- Smallpox, eradicated in 1980. Stored in Russia and USA, though many samples are unaccounted for. It serves as a very deadly WMD given that no humans are immunized against it.
- Highly infectious and easily aerosolized.
- It can survive for 24 hours, and possibly 48 hours, in the environment. The occurrence of smallpox in hospital employees whose only exposure was handling of laundry from infected people is testimony to its viability. Approximately 30% of exposed people become ill. One infected person has the potential to infect up to 20 other individuals. People are infectious from the time the rash first appears until the scabs fall off (1 or 2 weeks). Anyone exposed to smallpox should be closely monitored by public health authorities for 17 days to rule out infection.
- Smallpox has various forms: variola minor and variola major (the classic form with high mortality).
- Two other forms of the disease, hemorrhagic and malignant (or flat) smallpox, are seen in 10% of cases; the mortality rate is greater than 90%.
- The smallpox rash can take any of these forms:
- Petechiae and hemorrhage (HF)
- Soft, flat lesions with no progression to pustules (MF)
- Maculopapular rash progressing to a vesicular and pustular rash
- The infection begins when the virus is inhaled. After migrating to regional lymph nodes, the virus replicates for 3 or 4 days and then asymptomatically spreads to the spleen, bone marrow, other lymphoid tissue, and liver. A second viremia occurs 8 to 12 days later and is associated with fever, prostration, and headache. Mental status changes can occur. During this phase, which lasts 2 or 3 days, the virus localizes to the skin and pharyngeal mucosa. A maculopapular rash soon appears, which becomes vesicular and finally pustular.
- In contrast to chickenpox, the rash first appears on the face and forearms, later spreading to the legs and trunk. All the lesions in any one area of the body are at the same stage. During the next 8 to 14 days, the pustules crust over and separate from the skin, leaving pitted scars.
- Highly recommend this resource from the CDC:
[5] How are nerve agents treated (3 drugs)?
- Unlike biological WMD, these chemical agents manifest within a few hours of contact. The challenge is decontamination and treatment.
- The four basic classes of chemical compounds are:
- nerve agents
- SARIN: highly volatile, high risk for inhalation
- VX : low volatility, risk for liquid exposure
- In general, victims have symptoms after skin exposure. The median lethal dose (LD50) for VX is 10 mg, a droplet slightly larger than a pinhead. Death from doses of this size occurs in less than 30 minutes.
- vesicants (blistering)
- cyanides (previously referred to as blood agents)
- pulmonary intoxicants (previously referred to as choking agents)
- Although all have potential for use as weapons, the nerve agents and vesicants are thought to represent the greatest threat.
- Nerve agents are organophosphates. They inhibit the enzyme acetylcholinesterase, blocking the degradation of acetylcholine at the postsynaptic membrane.
- Acetylcholine accumulates, resulting in overstimulation of muscarinic and nicotinic receptors
- Muscarinic stimulation = miosis, salivation, rhinorrhea, lacrimation, bronchorrhea, bronchospasm, vomiting, and defecation.
- Nicotinic stimulation = muscle fasciculations, flaccid paralysis, tachycardia, and hypertension.
- Nerve agents (like the name suggestions) also stimulate the brain = SEIZURES, COMA, APNEA.
- In addition to good decontamination (all clothes off, don hair net and clothes), all healthcare workers must have excellent protective suits on.
- The treatment of nerve agent victims depends on the form (liquid or vapor) and level of exposure (mild, moderate, or severe).
- Three drugs are the mainstay of treatment:
- Atropine for the muscarinic effects (improves ventilation),
- Titrate to SECRETIONS, no miosis or HR.
- Pralidoxime chloride (2-PAM) for the nicotinic effects (reverses paralysis),
- Less effective >6 hrs post exposure due to AGING = defined as the permanent attachment of sarin to the acetylcholinesterase enzyme.
- Diazepam/midazolam for the prevention and treatment of seizures
- Atropine for the muscarinic effects (improves ventilation),
- An autoinjector kit (Mark I) approved by the FDA consists of two cartridges, one containing atropine (2 mg) and the other 2-PAM (600 mg).
- Mark I kits are available as part of civilian pharmaceutical caches strategically located throughout the United States. A newer version with both drugs combined in a single autoinjector (Antidote Treatment Nerve Agent Auto-Injector referred to as DuoDote) will gradually replace the Mark I kits. An autoinjector containing 10 mg of diazepam is an additional option if intravenous access is not possible.
- See Rosen’s Box 193.9 for original Treatment of Nerve Agent Exposure
- Vapour
- Mild: Observe for 1 hour, then release; no treatment
- Moderate: One or two Mark I kits IM; or atropine, 2 to 4 mg IV, may repeat every 5 to 10 minutes as needed; and 2-PAM, 1 g IV during 30 minutes, may repeat every hour as needed
- Severe: Three Mark I kits IM and one diazepam autoinjector IM; or atropine, 6 mg IV, may repeat 2-mg boluses IV every 5 to 10 minutes; and 2-PAM, 1 g IV during 30 minutes, repeat every hour for total of 3 g; and midazolam or diazepam, 5 mg IV, or midazolam 10 mg IM, may repeat as needed
- Liquid
- Mild: One Mark I kit IM; or atropine, 2 mg IV; and 2-PAM, 1 g IV during 30 minutes
- Moderate: Same as for vapor
- Severe: Same as for vapor
- Paediatric doses
- Atropine, 0.02mg/g IV
- 2-PAM, 20 to 40 mg/kg IV during 20-30 minutes
- Midazolam (0.15 mg/kg IV) or diazepam (0.2 to 0.3 mg/kg IV)
- Give atropine before attempting intubation, otherwise airway resistance will inhibit ventilation.
- Continue atropine until secretions dry (usually 20mg)
- In hypoxic patients, IV atropine has been reported to cause VFib, so using IM atropine
- Vapour
- Three drugs are the mainstay of treatment:
- nerve agents
[6] Describe the clinical effects of mustard gas. How is this treated?
- Mustard gas is a VESICANT or a blistering agents; they are chemical warfare agents that induce blister formation on contact with skin.
- Mustard is a liquid at room temperature but has both liquid and vapor toxicity. Injury from mustard exposure occurs in 1 or 2 minutes, but symptoms do not develop for 4 to 8 hours.
- The hallmark of mustard injury is skin blisters resembling second-degree burns. Within 4 to 8 hours of exposure, erythema and burning occur, followed by vesicle and bulla formation.
- Mustard has both local and systemic toxicity. Local effects occur from direct exposure to the skin, eyes, and airway – it is thought to cause direct DNA damage and has radiomimetic effects.
- Systemic effects result from the impact of absorbed mustard on the bone marrow.
- Skin exposure:
- Treatment is supportive (tetanus rx, burn care) and includes decontamination (to prevent secondary contamination) and airway maintenance. No specific antidote for mustard is currently available.
- Fluid losses from mustard injury are much less than those associated with thermal burns. Therefore, standard burn formulas for fluid administration do not apply, and caution should be used to avoid overhydration.
- Airway injury:
- Mild exposure causes irritation of the nose, sinuses, and pharynx and can be treated with cool, humidified mist.
- Moderate exposure extends to the larynx and upper trachea and may require treatment with oxygen, continuous positive airway pressure, or even intubation.
- Severe exposure involves the lungs, producing hemorrhagic necrosis of the bronchioles. Pulmonary edema is rare. Intubation is usually required, and patients may benefit from positive end-expiratory pressure and inline bronchodilators. Steroids are of questionable benefit, and antibiotics should be given only for established infection.
- Systemic toxicity from mustard is caused by bone marrow suppression. Absorbed mustard kills stem cells, causing the white blood cell count to decline after 3 to 5 days. Survival is rare if the white blood cell count falls below 200, which generally occurs when more than 50% of the total body surface area is involved from exposure to liquid agent. Death after mustard exposure usually results from secondary infection and respiratory failure.
Check out the textbook for the brief blurbs on Cyanides (and other blood agents) – which inhibit cellular oxygen use; as well as the pulmonary intoxicants (Phosgene and Chlorine).
[bg_faq_end]This post was uploaded and copyedited by Kevin Lam