This episode of CRACKCast covers Rosen’s Chapter 143, Diving Injuries and Dysbarism. While infrequently encountered except for those centers frequented by SCUBA enthusiasts, we must know the hard facts on the potentially life-threatening diving related injuries that may occur suddenly and need urgent attention.
Shownotes – PDF Here
[bg_faq_start]Key Concepts
- The majority of dive injuries are diagnosed on the basis of the focused dive history and physical examination alone; they are best differentiated into disorders of descent, disorders of depth, and disorders of ascent.
- The U.S. Navy Diving Manual and the Divers Alert Network (DAN) are valuable resources for the clinician presented with a diving emergency. DAN provides a 24-hour medical emergency hotline at 1-919-684-9111 (collect calls are accepted) and a nonemergency advisory line Monday through Friday, 8:30 am to 5 pm Eastern time, at 1-919-684-2948 or 1-800-446-2671
- International numbers by country: https://www.diversalertnetwork.org/about/international
- International Emergency hotline: +1 919 684-9111
- DAN serves as the headquarters for IDAN. Regions of coverage include the United States and Canada. Diving Emergencies: +1-919-684-9111 (accepts collect calls)
- Treatment with 100% oxygen is the initial therapy for all diving emergencies until the diagnoses can be determined. It has been demonstrated to reduce the morbidity and mortality related to decompression illness and can be helpful in patients with pneumothorax.
- Imaging and laboratory studies are not useful for ruling in decompression and should not delay definitive recompression therapy.
- With the exception of DCS, AGE, and possibly carbon monoxide poisoning from contaminated air, most dive-related disorders can be treated without recompression therapy. Recompression treatment is recommended for patients with DCS and AGE.
Rosen’s in Perspective
Diving has a fascinating history, which we don’t have time to go into, so check it out in Rosen’s. But the traditional term “the bends” originated from workers building the Brooklyn Bridge – developing symptoms from nitrogen gas coming out of solution due to rapid ascent out of deep sea working conditions.
Since the invention of SCUBA (self-contained underwater breathing apparatus’) gear people are able to use compressed air or gas mixes to dive even deeper….and gain increasing popularity. Diving related injury incidence varies from 0.01%-0.02%, and mortality is 1-9 per 100,000 dives.
We’ll cover this again in the next chapter, but as a review:
- Atmospheric pressure = 760 mmHg at sea level.
- Water = denser than air
- g. An alpinist needs to ascend 18,000 ft to reduce atm pressure by 50%, but a diver only needs to descend 33 ft in sea water to double atmospheric pressure
- Key breakdown:
- Disorders of:
- Descent
- Depth
- Ascent
- Disorders of:
[1] List 5 potential injuries in scuba diving other than Dysbarism
- Environmental exposures
- Hypothermia
- Sunburn
- Trauma (harpoon injury)
- Aquatic exposures:
- Submersion accidents (drowning)
- Motion sickness
- Marine envenomations (see Ch. 61 – box jellyfish, blue octopus, rockfish)
All the other dysbarisms and barotraumas are due to rapid pressure-volume changes in air-filled cavities or nitrogen dissolved into body tissues coming out…
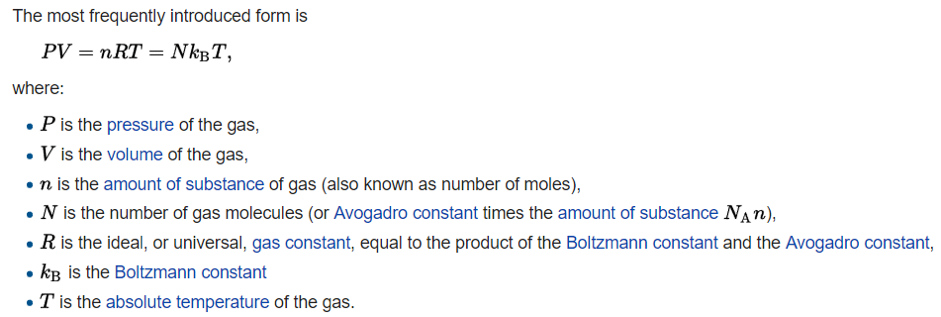
[2] What is the ideal gas law?
- Wikipedia
[3] Describe the following laws:
…let’s talk about some laws of physics – defining the behaviour of liquids and gases…This first one is easy, think of it like a tube a toothpaste. Since most of our body is made of water……
- Pascal’s Law : ΔP = pg(Δh)
- A pressure applied to any part of a liquid is transmitted equally throughout. We care because….as the pressure increases in a confined space (e.g. the inner and middle ear) it will cause barotrauma to the adjacent structures – inner/middle ear structures
These adjacent pressure changes affect the volume of air filled spaces in the body (lungs, bowel, sinuses, middle ear). These fragile structures (just like any other hollow tube (tire, balloon)) don’t do well when they are overfilled!
- Boyle’s Law : P1V1 = P2V2 (at a constant temp)
- The pressure and volume of a gas are inversely proportional to each other. …the volume of a gas (air) will decrease as the pressure (due to depth) increases. **this also applies to changes that occur in gas supplies** We care because as dives deeper (more pressure), the gas bubble volume will decrease. The greatest change happens in the first 33 ft (100% → 50% volume change)
- Low pressure = high volume; high pressure = low volume.
- Charles’ Law: V1/T1 = V2/T2
- Addresses the effect of temperature on gases: “at a constant pressure, the volume of a gas is directly proportional to the change in absolute temperature.
- Therefore, with head the volume of a gas will increase.
- General Gas Law: P1 x V1/T1 = P2 x V2/T2
- This law combines charles’ boyle’s gas laws. It relates pressure, volume and temperature in one equation when they aren’t constant.
- Dalton’s Law: Ptotal = P1 + P2 + P3 etc…
- The total pressure exerted by a mixture of gases is equal to the sum of their individual partial pressures. We care because nitrogen under pressure acts as if no other gases are present.
- Henry’s Law: ep=ekc
- …the amount of any gas that dissolves in a liquid at a given temperature is directly proportional to the partial pressure of that gas.
- We care because more nitrogen is taken into solution (your blood) at higher pressures, than comes out of solution at lower pressures.
- At higher pressures, the concentration of each component of air in blood and tissues increases until a steady state is reached.
- Boyle’s Law : P1V1 = P2V2 (at a constant temp)
If you’re only going to remember two; I’d suggest these two:
- Boyle’s law states that at a constant temperature, the volume of a gas varies inversely with the pressure to which it is subjected. This law helps to explain the principles behind diving-related barotrauma and air embolism.
- Henry’s law states that at a constant temperature, the amount of a gas that is dissolved in a liquid is directly proportional to the partial pressure of that gas. This law provides the explanation for decompression sickness and nitrogen narcosis.
[4] Describe the basic pathophysiology of decompression sickness
- According to Boyle’s and Henry’s laws – the gases from a diver’s breathing mixture are dissolved into the body
- Also, the longer a diver is at depth, the greater the amount of gas will dissolve into the tissues
- With ASCENT most of the dissolved gas comes out of solution → if this is rapid the body can’t accommodate all the bubbles leading to DCS;
- ****think of it like opening a bottle of carbonated beverage*****
- If the bottle is shaken and opened rapidly, it foams over and causes a mess (DCS), but if it’s opened slowly then the pressure release is controlled (and the lung is able to clear the excess gas through its vascular bed).
- DCS = decompression sickness
- A spectrum of clinical illnesses – due to the formation of small bubbles of nitrogen gas in the blood and tissues on ASCENT!
- LOCATION, location, location of the bubbles – determines the type of symptoms that arise
- Fetal circulation anatomy explains why pregnant women should not dive.
- Multiple small bubbles normally occur on ascent, but if they become persistent, large or too numerous for the lungs to filter → inflammatory cascades ensue, cytokines, thrombosis, ischemia, obstruction etc. can occur.
- These bubbles can cause ischemia and hypoxia if large
- ***Nitrogen is highly fat soluble – so it can very easily absorb into the white matter of the CNS → leading to huge problems when the pressure suddenly drops.
- ****think of it like opening a bottle of carbonated beverage*****
[5] List 5 potential injuries a diver can sustain in descent, at depth, and on ascent
See Figure 143-8 (8th) / 135.9 (9th)
- Descent: – head squeezed like a tube of toothpaste
- Middle Ear Barotrauma
- Most common complaint among divers
- Inner Ear Barotrauma
- External Ear Barotrauma
- Rare – due to wax in the auditory canal.
- Facial barotrauma
- Due to the dive mask eye-nose interface if the diver doesn’t exhale through their nose.
- Can cause facial / conjunctival edema, petechial hemorrhages, subconjunctival hemorrhages.
- Sinus barotrauma
- barosinusitis is the 2nd most common complaint among divers.
- Can occur on descent or ascent, causing facial pain/epistaxis
- At depth: – too much funny gas: huffing that helium balloon
- Nitrogen narcosis
- Oxygen toxicity
- Contaminated gases
- Hypothermia
- Ascent: – opening a shaken bottle of pop
- Rapid up
- Alternobaric vertigo
- Inability to equalize pressure in the middle ear during ascent, problematic with concurrent URTI
- Increased pressure in the middle ear causes nystagmus
- Pulmonary overpressurization syndrome
- Air gas embolism
- Pneumothorax
- Pneumomediastinum
- Pulmonary hemorrhage
- Barodontalgia
- Air is trapped beneath a poorly filled dental cavity – and expands on ascent (benign and self limited)
- GI barotrauma
- Rare problem. Suspect in someone with a diving history and abdominal pain
- Due to expanding bowel gas due to carbonated beverages/large meals/gassy foods.
- Long and deep
- DCS I or II
- Arterial gas embolism
- Alternobaric vertigo
- Rapid up
- barosinusitis is the 2nd most common complaint among divers.
- Middle Ear Barotrauma
[6] Describe the difference between MEBT, IEBT, ABV and Middle Ear DCS
These are all tricky entities – and the differential diagnosis of MEBT, IEBT, inner ear DCS, ABV includes all….See Table 135.2 (9th)
| Middle Ear Barotrauma (consider ruptured TM)
Very common
Transient and self limited
| Inner Ear Barotrauma
| Alternobaric Vertigo
Transient and self limited | Middle ear Decompression Sickness
Dive occurs near compression limits |
| **most common complaint of scuba divers** – 10-30% experience this
Most divers attempt to stent the Eustachian Tube open, but if it collapses – symptoms of tinnitus, vertigo develop
| Damage to the cochleovestibular apparatus.
If the diver is unable to equalize the pressure in the middle ear during descent – the pressure is transmitted to the perilymph of the cochlea
If it suddenly equilibrates with a valsalva can lead to inner ear hemorrhage or labyrinthine window tear. | Due to an inability to equalize pressure within the middle ear during ascent (usually this happens naturally on ascent). This error is due to mucosal edema.
If the pressure gradient is excessive – labyrinthine discharge occurs
Profound nausea/vomiting; blurred vision; transient hearing loss
| Same as the others,
But occurs during ascent or after surfacing! |
| further pressure may lead to TM rupture, nystagmus, vertigo, and CN VII palsy | Hearing loss, severe vertigo, nausea, tinnitus, fullness.
Severe nystagmus, positional vertigo, ataxia, vomiting.
PERSISTENT symptoms: +ve rhomberg, persistent hearing loss
| Nystagmus, emesis, TM injury, nausea
Usually self limited. | |
| Descent | Descent
“Difficulty equilibrating or tried performing a vigorous valsalva” | At depth OR During ascent | Ascent – or soon after surfacing
*diver approached decompression limits; onset on ascent or soon after; other neurological symptoms” |
***IEBT may be nearly impossible to distinguish from DCS Type II – and should not delay decompression if there is any doubt***
[7] What is nitrogen narcosis?
- “Rapture of the deep”
- Intoxicating effects of increased tissue nitrogen concentration
- Signs and Symptoms
- Euphoria, false well-being, confusion, poor judgement/skill, disorientation, laughter, diminished motor control, paresthesias/numbness in lips/gums/legs.
- Typically occurs at depths below 100 ft when compressed air is used
- Symptoms usually resolve with ascent, but can result in drowning, or dive emergencies because of poor motor control
- A similar toxicity can occur with elevated partial pressures of oxygen for a long period of time; but this only occurs with deep dives without complex hypoxic gas mixtures.
[8] List 6 risk factors of decompression sickness. List the 2 types of decompression sickness (clinical features)
What is the pathophysiology of decompression sickness? A great explanation from Uptodate:
- As a diver descends and breathes air under increased pressure, the tissues become loaded with increased quantities of oxygen and nitrogen as predicted by Henry’s law.
- As the diver returns to the surface, the sum of the gas tensions in the tissue may exceed the ambient pressure and lead to the liberation of free gas from the tissues in the form of bubbles; the location of bubble formation is somewhat dependent upon tissue characteristics. The liberated gas bubbles can alter organ function by blocking vessels, rupturing or compressing tissue, or activating clotting and inflammatory cascades. The volume and location of these bubbles determine if symptoms occur.
I think about it like using a SodaStream…you charge the water with pressure and carbon dioxide, and then when you take the cap off and start drinking the CO2 comes out of solution.
DCS = decompression sickness
- Incidence:
- 8 / 10000 (a few recent deaths!)
- Risk factors:
- Patient:
- Obesity
- Older age
- Fatigue, dehydration, fever
- Heavy exertion
- Male gender
- ETOH / Tobacco use
- Presence of a Patent Foramen Ovale
- Most sport diver’s aren’t screened for this – and some may even have normal bubble-ECHO studies: suggesting that the PFO may only open at high ambient pressures
- Energy:
- Repetitive dives within several hours of each other
- Environment:
- Longer dive (>time)
- Deeper dive
- Almost never occurs with dives < 6 meters deep
- Cold ambient temperature
- High altitude diving
- Flying after diving
- Patient:
The US Navy has developed dive tables – which are usually programed into dive “computers” – that set limits to prevent DCS. If these limits are exceeded a diver must do “decompression stops underwater” to off-gas nitrogen built up in the tissues. But these are not a guarantee that DCS will not occur. Divers can develop DCS even when they are within any calculated no-decompression limit.
Presentation of DCS:
- Usually manifests within hours of surfacing – 60% occur within 3 hrs, and almost all occur within 24 hrs
- This can be hastened by ascending to altitude or flying – and sometimes can present DAYS after diving.
- Symptoms [ Fig 143-7 ] – in order of occurrence
- Pain (joint, muscle, girdle)
- Numbness, paresthesias
- Constitutional: h/a, lightheadedness, inappropriate fatigue, malaise, N/V
- Dizziness/vertigo
- Motor weakness
- Skin findings
- Muscular stiffness, pressure, cramps
- Mental status changes
- dyspnea/cough
- Auditory
- Bladder bowel
“Decompression-related illness” – all get treated the same!!
| Type I DCS “The 1’s” -MSK system, skin, lymphatics | Type II DCS: the “doubles”; the SERIOUS stuff is SECOND -CNS, ear, lungs, heart | |
| Symptoms | Periarticular pain in the arms, and legs. Elbow and shoulder pain most common.
Watch for cutis marmorata – patchy cyanotic marbling of the skin (trunk and torso) – may first show up as pruritus, then erythema, then mottling. This is due to venous stasis.
Lymphatic obstruction presents with edema. | Spinal cord at high risk – lumbar region: ● Limb weakness/paralysis ● Paresthesias – distal to proximal migration ● Numbness ● Low back/abdominal pain ● Bladder symptoms, fecal incontinence, priapism ● Patchy symptoms Cerebral symptoms: ● Headache, blurred vision, diplopia, dysarthria, fatigue, behaviour or mood changes Inner ear: ● Same symptoms as IEBT – nausea, dizziness, vertigo, nystagmus (happens on ascent or surfacing) Pulmonary: ● Dyspnea, cough, chest pain. ● Cyanosis, hypotension |
| Diagnosis | Can be confirmed by placing a BP cuff on an affected joint and inflating it to 150-200 mmHg with pain relief! | CT and MRI may identify the gas bubbles in the brain/spinal cord ECG may show right sided heart strain in pulmonary DCS |
Don’t forget that DCS I-II-& AGE can coexist
[9] List 5 potential pathologies associated with pulmonary barotrauma
A diver who takes a full breath at 33 fsw (feet below sea water), will have TWICE the volume of air in their lungs at the surface (according to Boyle’s law).
- A change in depth of as little as 3-4 ft can force air bubbles across the alveolar-capillary membrane
- This volume expansion either causes the alveoli to rupture (pneumo) or the gas goes across the alveolar-capillary membrane to cause an air gas embolism
- *****the greatest risk for pulmonary barotrauma occurs in less than 10 feet of water*****
Clinical entities to watch for:
- Pneumothorax
- Pneumomediastinum
- Subcutaneous Emphysema
- Alveolar hemorrhage
Pearls:
- Asthmatics: two fold higher risk due to:
- Narrow airways, bronchospasm and mucous plugs, reduction of breathing capacity with depth (100 fsw – 50% reduction), breathing of cool air can cause bronchospasm, compressed air can be contaminated with pollen.
- Asthmatics have rules/regulations about safety to dive as a result
- Risk factors: rapid ascent, panic, buoyancy regulation problems, insufficient air for the dive
[10] Describe the management of DCS. What other diving disorders require recompression therapy?
ALL types of decompression illnesses require recompression – with the goal of washing out nitrogen, compressing air bubbles, deliver oxygen to ischemic tissue. Recompression therapy is the only definitive treatment for DCS and AGE – even if spontaneously resolved. Recompression therapy may still be helpful, even if delayed up to 10-14 days.
Indications (See Box 143-2)
- DCS I, II,
- AGE
- Delays of 5 hrs, lead to 50% mortality with AGE.
- Contaminated air (causing CO poisoning)
- Problem with packaging the gas, rebreathers with soda lime dust contamination, etc.
- How would you manage a patient requiring recompression in the pre-hospital and ED environment (pre-HBO treatment)? While resuscitating in the ER:
- Put the patient on 100% O2
- Follow the ACLS guidelines
- Take a history and physical!
- – look for DCS Type I or II!
- Resuscitate with IV fluids, to goal u/o of 0.5 ml/kg/hr
- Don’t over resuscitate people with pulmonary edema or AGE!!
- Treat and avoid hypothermia
- Positioning the patient in the left lateral decubitus (Durant’s maneuver) and mild Trendelenburg (bed angled downward toward head) position in an effort to restore forward blood flow by placing the right ventricular outflow tract inferior to the right ventricular cavity, permitting air to migrate superiorly to a nonobstructing position
White and black pearls….
- No benefits with ASA, steroids
- Consider lidocaine IV for anyone with AGE and serious neurosymptoms – for neuroprotection
- Cardiac arrhythmias may not respond to defibrillation until the patient is recompressed
- Benzos for seizures
- Fill the foley and the ET balloon with saline (not air)
See [Box 135.6] for disorders not needing re-compressive therapy.
[11] What is an Arterial Gas Embolism (AGE)
- Type of “decompression related illness”
- SERIOUS form of DCS
- Air bubbles forced across alveolar-capillary membrane → pulmonary Vein → LA-LV then rest of the body
- ******most common cause of death in divers********
- Especially with cerebral or coronary embolisation
- Can occur even after a short, shallow dive.
- Symptoms:
- Sudden onset
- ***cerebral symptoms***
- Loss of consciousness
- h/a, confusion, convulsions, motor/sensory loss, alteration of normal consciousness, seizures, visual changes, ataxia
- Cardiac arrhythmias / arrest
How would you differentiate between AGE and pulmonary DCS?
| DCS | AGE |
| Pulmonary DCS due to rapid ascent without proper exhalation
Type 2 DCS – the more severe type
Rare, can progress to AGE
| ● Gas bubbles enter the pulmonary vein due to a ruptured alveoli that leaks air into the pulmonary vein ● Venous gas emboli develop due to barotrauma or DCS that overwhelms the pulmonary circulation ● Venous emboli sneak through a patent foramen ovale |
| Symptomatic venous gas embolism to the lungs → chest pain, wheezing, dyspnea, pharyngeal irritation
“Air lock” is another potential risk in pulmonary DCS where the RV outflow tract is obstructed leading to circulatory collapse and death (or progressing to AGE if there is a PFO)
| Embolization causes the most serious effects when it spreads to the brain or coronary arteries Symptoms of altered mental status / stroke or cardiac ischemia/arrhythmias
|
The 10 minute rule of thumb
“Any diver breathing compressed air at any depth underwater who surfaces unconscious or who loses consciousness within 10 minutes of reaching the surface should be assumed to be suffering from AGE.” DCS typically presents after 10 minutes and may present up to 24 hrs.
[bg_faq_end]Wisecracks
[bg_faq_start][1] Describe memory aids for the gas laws
Pascal’s law – Tube of Toothpaste: A pressure applied to any part of a liquid is transmitted equally throughout.
Boyle’s law – Syringe aspirating fluid: at work you draw up local anesthetic or any drug by withdrawing a plunger on a syringe (decreasing the pressure inside the chamber and increasing the volume of the chamber) thereby creating an area of less negative pressure and more volume for the drug or liquid to enter! The incremental changes in pressure (and therefore volume) are greatest at the surface, so barotrauma most commonly occurs near the surface (other at the beginning or at the end of a dive). Long or deep dives are not required for barotrauma.
Henry’s law – Carbonated soft drink analogy: An everyday example is given by one’s experience with carbonated soft drinks, which contain dissolved carbon dioxide. Before opening, the gas above the drink in its container is almost pure carbon dioxide, at a pressure higher than atmospheric pressure. After the bottle is opened, this gas escapes, moving the partial pressure of carbon dioxide above the liquid to be much lower, resulting in degassing as the dissolved carbon dioxide comes out of solution. – Wikipedia
[2] What are key aspects of a diving history?
See Box 143-1 and Figure 143-8
- Dive profile
- Depth and length of dive
- **when did the symptoms first occur**
- Ask members of the dive group
Focus on treatment decisions, rather than exact diagnosis. Call your HB doc sooner!
[3] What are the types of gas-mixture injuries?
Divers who dive to less than 130 feet usually just use compressed air; however when people go deeper they may use an artificial mixture of gas to extend the duration of their “bottom time” and avoid some of the disorders that happen at depth. Examples are nitrox, trimix, and heliox.
The main challenge is either oxygen toxicity or hypoxemia due to the gas blend ratios and dive profile. In Nitrox the percentage of oxygen in the mix is increased, reducing the nitrogen fraction. This means that there is less nitrogen uptake at a given depth.
The critical caveat with nitrox is that its higher oxygen content means that a diver breathing nitrox is at risk of developing oxygen toxicity at a shallower depth than a diver breathing air. Therefore, these folks are at risk for oxygen toxicity.
See: https://www.diversalertnetwork.org/medical/faq/Breathing-gas-mixture
There can also be major risks when mixing the gases – explosions, fires, asphyxiation, toxic additive additions (CO poisoning), hydrocarbons and others.
[4] What are the indications for re-compression (hyperbaric treatment)? How does it work?
- Air gas embolism
- Decompression sickness types 1 and/or 2
- Carbon monoxide poisoning (contaminated air)
Reduction of gas bubble size — The use of hyperbaric oxygen therapy for decompression illness is based upon Boyle’s Law, since the volume of nitrogen bubbles is inversely related to the pressure exerted upon it. At 3.0 atm, bubble volume decreases by approximately two-thirds. Further bubble dissolution is accomplished by the replacement of inert nitrogen within the bubbles with oxygen, which is then rapidly metabolized by tissues. – uptodate
[5] What complications of asthma are associated with diving?
A patient with active asthma should also be strongly discouraged from diving even if they have normal pulmonary function tests, because individual lung units may have prolonged time constants, exhibit gas trapping, and rupture upon ascent. However, asthmatics at their baseline status with normal pulmonary function and easily controlled airway reactivity during exercise are probably at only a minimally increased risk of diving-related barotrauma. – Uptodate
[6] List five causes of dizziness associated with diving.
- AGE
- DCS type 2 (neurologic)
- DCS type 1 (inner ear DCS)
- Inner ear barotrauma (ear squeeze)
- Anything else:
- Oxygen toxicity
- Nitrogen narcosis
- Hypoglycemia
So, ask when the dizziness started! IF you can’t figure it out, call hyperbarics and consider diving them!
[7] When post-dive is it ok to go on a trans-continental flight?
The post dive pre-flight surface interval = depends on the diver’s repetitive group designator or residual nitrogen time. The time to flight interval depends on the number of dives, their depths and if no-decompression limits were approached.
You’d be safe if you didn’t have any DCS or AGE symptoms if you waited 48 hrs….but as an example you’d be able to fly after 12 hrs of surfacing if you had less than 2 hrs of dive time in the last 48 hrs.
This also brings up the questions about how to get a patient to decompressive therapy. Ideally the plane should be pressurized to < 1000 ft. A helicopter should fly <500 ft.
[bg_faq_end]This post copy-edited and uploaded by Andrew Guy


