This episode of CRACKCast covers Rosen’s Chapter 118 (108 in 9th), SLE and Vasculitides. These are complex patients with a constellation of seemingly unrelated symptoms that can be difficult to tie together. However, their presentation to the ED is often a more serious complication of their disease process and represents an opportunity to intervene and help make the diagnosis.
Shownotes – PDF Here
[bg_faq_start]Systemic Lupus Erythematosus (SLE)
- SLE may affect any organ system. Thus, a fundamental understanding of the disease is required to tailor the differential diagnosis and evaluation.
- A 50-fold increased risk of coronary artery disease (CAD) and up to a 30-fold increased risk of venous thromboembolism in patients with SLE prompt chest pain evaluations in the emergency department (ED), even in young women.
- An elevated C-reactive protein level is more closely linked to infection in SLE patients and is not reflective of SLE disease activity
- An isolated elevated partial thromboplastin time (PTT) in a patient with SLE prompts consideration for antiphospholipid (aPL) antibody carrier state and, if there is a history of thrombosis, antiphospholipid syndrome (APS).
- Steroids are the mainstay for management of the majority of conditions that are associated with increased SLE disease activity, including musculoskeletal, cutaneous, renal, pleural, and pericardial disease.
- APS is common in patients with SLE and carries with it a risk of venous (typically deep venous thrombosis or pulmonary embolism) and arterial (most commonly stroke) thrombosis.
- Consultation with a rheumatologist may be helpful in diagnostic, management, and disposition decisions for patients with SLE.
Vasculitides
- Vasculitis syndromes should be considered in the presence of systemic symptoms, such as fever, malaise, and weight loss plus pulmonary, renal, or cutaneous manifestations.
- Massive hemoptysis and acute renal failure can occur in Wegener’s granulomatosis, Goodpasture’s disease, microscopic polyangiitis, and Churg-Strauss syndrome.
- Tracheal stenosis may be present in Wegener’s granulomatosis, further complicating airway management.
- Many patients with established vasculitis are receiving high-dose or combination immunosuppressive therapy, making them vulnerable to opportunistic infections and overwhelming sepsis.
[1] What the pathophysiology of lupus?
If you don’t know, it’s because no one truly knows!!! This is a multisystem autoimmune disease with every clinical manifestation known to man!
- 90% cases are women = strong role of estrogen? Throw on top of that importance of HLA alleles giving lots of overlap, making genetics a strong risk factor.
- SLE is the “prototype of all systemic autoimmune disease.” Long story short, the body starts producing antibodies via B-Cells directed towards host antigens, IE starts attacking itself.
- These auto-antibodies (think for example anti– double-stranded DNA antibody) start destroying multiple organ systems
[2] List diagnostic criteria for SLE
- See table 108.1 in Rosens 9th Edition – SLE and Vasculitides
| Clinical Criteria | Immunological Criteria |
| · Acute cutaneous lupus · Chronic cutaneous lupus · Oral ulcers · Non-scarring alopecia · Synovitis · Serositis · Renal disorder · Neurological disorder · Hemolytic anemia / leukopenia / thrombocytopenia
| · ANA elevation · Anti-Sm elevation · aPL antibody elevation · Low complement levels · Direct coombs test positive |
Table 108.1 is very busy – Remember the only mnemonic from med school
SOAP BRAIN MD
- Serositis
- Oral Ulcers
- Arthritis
- Photosensitivity & Pulmonary Fibrosis
- Blood cells (pancytopenia)
- Renal, Raynauds
- ANA
- Immunologic (anti-Sm, anti-dsDNA)
- Neuropsych
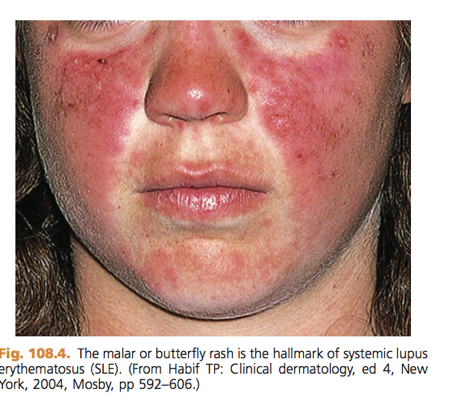
- Malar Rash
- Discoid Rash
[3] List drugs that induce lupus
- See Box 108.2 from Rosens 8th Edition – SLE and Vasculitides
Drugs Definitively Implicated in Causing Drug-Induced Lupus
- Procainamide
- Hydralazine
- Methyldopa
- Chlorpromazine
- Isoniazid
- Quinidine
- Minocycline
[4] Describe the clinical manifestations of SLE with classic triad & symptoms and signs by system
In general, 4 broad presentations
- Symptoms related to SLE that is not yet diagnosed (eg. idiopathic pericarditis, new rash)
- Progression or acute deterioration due to known SLE (eg, progressive nephritis, lupus enteritis)
- Complications of immunosuppression from treatment of SLE (eg, opportunistic infection)
- Complaints or disease unrelated to SLE (eg. trauma, pregnancy).
See Table 108.3 in Rosen’s 9th Edition – SLE and Vasculitides Chapter
Common or specific differential considerations with patients with SLE based on common presentations, comorbidities, or complications
| Pleuritic Chest Pain | Pericarditis, pleuritic, PE, PNA, MSK chest wall pain |
| Delirium | Neuropsychiatric lupus, steroid psychosis |
| Leg Swelling | DVT, renal failure, right heart failure, protein losing enteropathy |
| Shortness of breath
| PNA, anemia, pericarditis +/- effusion, pleuritic +/- effusion, ILD, shrinking lung syndrome |
| Pruritic or painful rash | Discoid SLE, drug reaction, sun exposure |
| Abdominal pain | Lupus enteritis, PUD, pancreatitis, pseudoobstruction |
| Fever | Infection, increased disease activity |
| Arthritis | Arthralgias, OA, septic arthritis, unrelated (gout, fibromyalgia) |
[5] List 3 drug regimens to treat SLE
- See table 108.4 in Rosen’s 9th Edition – SLE and Vasculitides
Medications and typical dosing range for acute SLE exacerbations
| Medication | Medication Class | Typical Regimen |
| Methylprednisolone | Glucocorticoid | 1-2mg/kg IV once daily |
| Prednisone | Glucocorticoid | 1-2mg/kg PO once daily |
| Hydroxychloroquine | Anti-malarial | 200-400mg PO once daily |
| Cyclophosphamide | Alkylating agent | 500-750mg/m2 IV once |
| Azathioprine | Antimetabolite | 25-50mg/day IV or PO |
[6] How does neonatal lupus present?
- Rash
- Erythematous annular lesions or arcuate macules with slight central atrophy and raised active margins look on scalp and face
- Can be confused with fungal infection, present at delivery or not until child has been exposed to UV
- Heart Block
- From first degree to complete
- Hepatic
- Elevated liver enzymes
- Mild hepatosplenomegaly
- Cholestasis
- Hepatitis
- Neurologic
- Hydrocephalus
- Macrocephaly
- Hematologic
- Anemia
- Neutropenia
- Thrombocytopenia
- Aplastic anemia
[7] What is antiphospholipid syndrome? What is the unusual laboratory feature seen with this condition?
Nearly 40% of SLE patients have APS!!! Happens when auto-antibodies are directed towards serum proteins. Examples:
- Lupus anticoagulant: most thrombogenic
- Anticardiolipin antibody
- Anti–β2-glycoprotein I antibody.
Box 108.1 – Rosens 8th Edition – SLE Vasculitides
Common clinical features of antiphospholipid syndrome
- Venous thrombosis
- Arterial thrombosis including stroke and TIA
- Recurrent miscarriage
- Livedo reticularis
- Thrombocytopenia
Note: “A small subset of those with APS may present with multiple thrombotic sites and organ failures simultaneously. This condition is known as catastrophic APS.”
Abnormal labs:
- Elevated PTT in the setting of a normal PT/INR
- Due to interference of the coagulation study by aPL antibodies. Confirm w/ mixing study.
- “A mixing study requires repeating the PTT with a mixture of the patient’s blood and a 50% contribution from normal, control serum. In the presence of an inhibiting antibody, the PTT will remain elevated. If, however, the PTT was elevated for other reasons (most commonly heparin), the addition of normal clotting factors from the control serum will restore the PTT to normal.”
- False positive VDRL
- “The Venereal Disease Research Laboratory (VDRL) assay to test for syphilis contains cardiolipin and thus will commonly be falsely positive in patients with anticardiolipin antibodies or APS.”
[8] What is the pathophysiology of vasculitis?
Easy answer: unknown
As Rosen’s states: “The cause of most vasculitis syndromes is unknown. Most cases are believed to result from immune complex deposition in blood vessel walls, prompting a complement-mediated inflammatory reaction. This results in vessel wall damage and necrosis, leading to stenosis, occlusion, and subsequent end-organ ischemia. The clinical manifestations are determined predominantly by the size and distribution of blood vessels involved along with the histologic subtype of inflammation.”
[9] Give examples of vasculitides based on vessel size
See table 108.5 in Rosens 9th Edition – SLE and Vasculitides
- Large vessel vasculitis
- Giant cell arteritis (GCA)
- Takayasu’s arteritis
- Medium vessel vasculitis
- Polyarteritis nodosa
- Buerger’s disease
- Kawasaki disease
- Small vessel vasculitis
- Goodpasture’s disease
- Wegener’s granulomatosis
- Microscopic polyangiitis
- Churg-strauss
- Behcet’s disease
- HSP
- Hypersensitivity vasculitis
- Subcutaneous vasculitis
- Large vessel vasculitis
[10] Compare the findings for vasculitis
- See table 108.6 in Rosens 9th Edition – SLE and Vasculitides
Essentially Rosens breaks it down by the relative presence of a variety of clinical and investigative findings based on the type of vasculitis you are dealing with, including considerations for features like:
- Pulmonary infiltrates and nodules
- Alveolar hemorrhage
- Glomerulonephritis
- Upper airway disease
- Purpura
- Peripheral nervous system involvement
- Central nervous system involvement
[11] List 5 criteria for the diagnosis of temporal arteritis and two associated features
- See box 108.4 in Rosens 8th Edition – SLE and Vasculitides
American College of Rheumatology Classification Criteria for GCA
- Age over 50 years old
- New onset localized headache
- Temporal artery tenderness or decreased temporal artery pulse
- ESR >50mm/hr
- Abnormal arterial biopsy specimen characterized by mononuclear infiltration or granulomatous inflammation
Associated features:
- Vision loss
- Jaw claudication
[12] Describe the features of Behcet’s Disease
Behçet’s disease = complex, chronic small-vessel vasculitis that may affect:
- Mucocutaneous
- Ocular
- Cardiovascular
- Renal
- Gastrointestinal
- Pulmonary
- Urologic
- Musculoskeletal
- Central nervous systems.
The ancient Greeks knew about it!
Definition includes the presence of:
- Aphthous oral ulcers
- Plus two or more of the following
- Genital aphthae
- Cutaneous lesions
- Neurologic, oral, or rheumatologic manifestations
Classic triad for Behçet’s disease
- Oral aphthous ulcers
- Genital ulcers
- Uveitis
[13] List 10 causes of Erythema Nodosum
[14] Compare Buerger’s, serum sickness and hypersensitivity vasculitis
See Table 108.7 in Rosen’s 9th Edition –SLE and Vasculitides
| BUERGERS DISEASE | SERUM SICKNESS | HYPERSENSITIVITY VASCULITIS | |
| Pathophysiology | Small / medium arteries and veins of the extremities
| Immune complex deposition in blood vessel walls | Small vessel |
| Associated exposures
| Heavy cigarette smoking Cold exposure | Foreign protein or serum Penicillin based antimicrobials Sulfa drugs NSAIDs | Beta lactam abx NSAIDs Diuretics |
| Common symptoms
| Pain, paresthesias, claudication, rest pain | Fever, arthralgias, diffuse lymphadenopathy. Pruritic skin lesions | Typically confined to skin (vs. serum sickness) |
| Physical exam findings
| Poorly healing wounds Ulcerations Splinter hemorrhages Digital ischemia and necrosis Distal to proximal progression | Urticaria Purpuric skin lesions Scarlatiniform rash Erythema multiforme Azotemia, proteinuria Myocarditis, pericarditis | Palpable purpura in dependent regions including legs and buttocks Urticarial vasculitis Livedo reticularis Skin nodules and ulcers |
| Diagnosis
| Angiography: demonstrates Corkscrew pattern of collateral vessels – rule out other ischemia causes | Clinical | Clinical |
| Management and outcome
| Smoking cessation Meticulous wound care Protection from trauma and thermal injury | Supportive Systemic steroids if severe Recovery generally 4-6 weeks | Supportive Systemic steroids if severe |
[15] List the diagnostic criteria for HSP
2 or more of the following:
- Age < 20
- Palpable Purpura
- Abdominal pain
- Vessel wall granulocytes on biopsy
Wise Cracks
[bg_faq_start][1] What is the differential for SLE patient and Chest pain?
See Table 108.2 Rosens 9th Edition – SLE and Vasculitides
- Pleuritis
- Pulmonary embolism
- Pneumonia
- Pericarditis
- Coronary artery disease
[2] Name and identify 2 pathognomonic clinical features for lupus
Malar Rash & Discoid Lupus
 |  |
[3] When should rheumatology be involved in the ED with a SLE patient?
Hold up – your SLE patient is not just an automatic turf to CTU! Here is an important list to consider from box 108.3 in Rosens 8th Edition – SLE and Vasculitides
Reasons for rheumatological referral for patients with SLE
- To confirm a diagnosis
- To assess disease activity and severity
- To provide general disease management
- To manage uncontrolled disease
- To manage organ involvement or life-threatening disease
- To manage or prevent treatment toxicities
- Special circumstances (APS, pregnancy, surgery)
[4] Spot Diagnosis: A 36 year old female stock trader present with what appears to be necrosis of the nose and ears…
[5] Spot diagnosis: 13 year old presents with abdo pain, polyarticular arthritis, foaming urine and the following rash…
Neonate 1 week post delivery
[6] Rounds Pimper: List 10 side effects of chronic steroid use
- Psychosis
- Amenorrhea
- Moon Facies
- Obesity
- Buffalo Hump
- Striae
- Poor wound healing / ulcers
- Muscle weakness
- Osteoporosis
- Avascular necrosis
- Immunosuppression & recurrent infections
- Hyperglycemia
- Hypertension
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)







