This episode of CRACKCast covers Rosen’s Chapter 97, Renal Failure. This chapter covers an approach to acute and chronic kidney injuries, including causes, complications and treatments.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
So what’s the emergency about kidney disease?
Well here’s the thought process:
- Identify renal failure (azotemia)
- Rule out life threats: hyperK, pulmonary edema
- Is this AKI or a pre-existing CKD?
- …all the rest of the steps we’ll cover in the show!
AKI can be from pre – renal, intrinsic parenchymal damage, or post renal / obstructive causes.
When you say Acute Tubular necrosis, it means the cause of intrinsic AKI can NOT be attributed to a glomerular, vascular, or interstitial cause
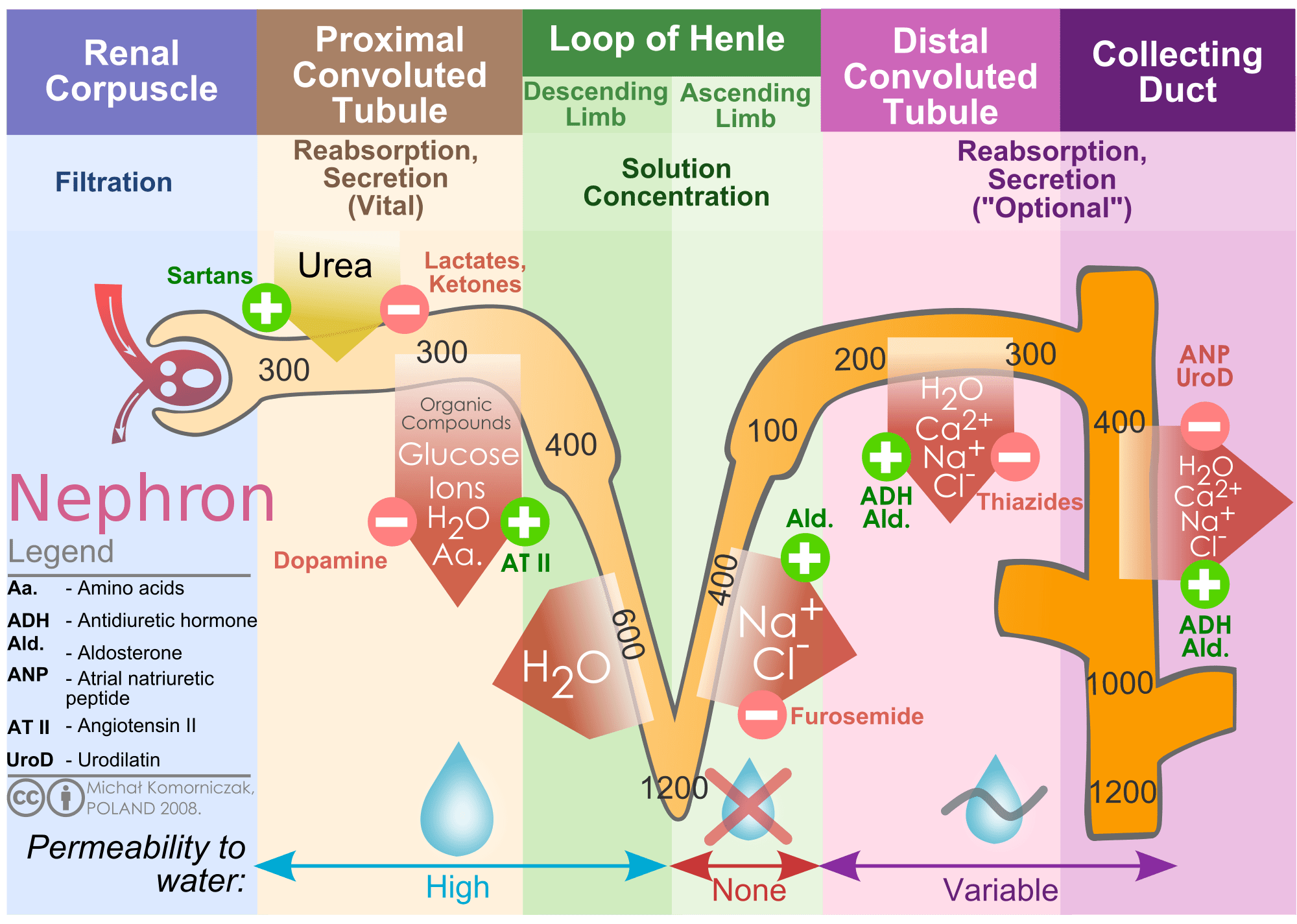
Quick refresher:

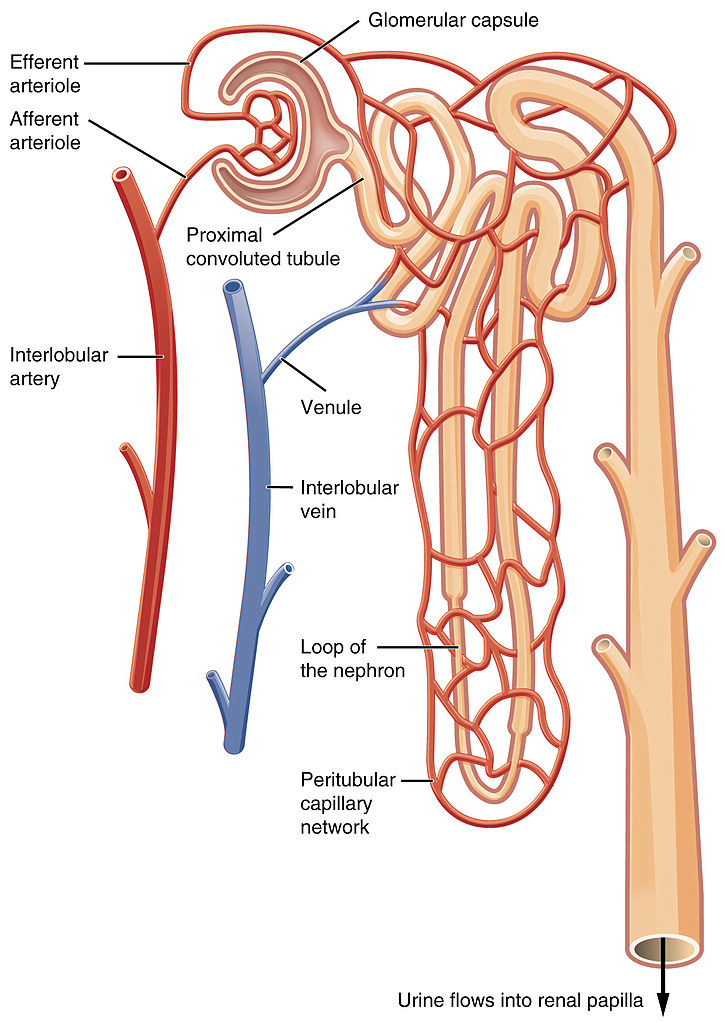
[1] Source: https://commons.wikimedia.org/wiki/File:2611_Blood_Flow_in_the_Nephron.jpg
[1] Source: https://commons.wikimedia.org/wiki/File:Kidney_nephron_molar_transport_diagram.svg
Soap Box:
Remember all you lasix happy people:
Patients w/ CHF or cirrhosis are often salt- overloaded and water-overloaded HOWEVER their effective intra-arterial volume is decreased.
Giving these patients diuretics can further decrease intravascular volume = decreased glomerular filtration and prerenal azotemia.
In the end “a state of chronic, stable, prerenal azotemia may be the best achievable compromise between symptomatic volume overload and severe renal hypoperfusion.” – Rosen’s 9th edition
[bg_faq_end][bg_faq_start]1) Describe a general approach to the evaluation of acute kidney injury (AKI)
Azotemia (azot, “nitrogen” + -emia, “blood condition”) is a medical condition characterized by abnormally high levels of nitrogen-containing compounds (such as urea, creatinine, various body waste compounds, and other nitrogen-rich compounds) in the blood. – Wikipedia.
Hx: Look for pre-renal causes:
- Decreased cardiac output signs & symptoms
(lightheadedness,SOB, PND, orthopnea etc) - Bleeding
- GI fluid loss
- Abnormal polyuria
Hx: Obstructive / Post Renal:
- Nocturia / frequency / hesitancy or decreased urinary stream
- Dysuria / hematuria (infection / inflammation or neoplasm)
- Hx kidney stones or chronic urinary tract infection (UTI).
Pearl: Hx of acute anuria (<100 mL of urine/day) = high-grade urinary tract obstruction but can also include :
- Severe volume depletion
- Severe acute glomerulonephritis
- Cortical necrosis
- Bilateral renal vascular occlusion.
Intermittent anuria usually = Obstruction
Ask about med use and other toxin exposures, rash, dark urine, fever and arthritis.
Refer to Fig 87.1 for a structured approach to Azotemia
[bg_faq_end][bg_faq_start]2) List clinical features of AKI
Box 87.1
Cardiovascular
- Pulmonary edema
- Arrhythmia
- Hypertension
- Pericarditis
- Pericardial effusion
- Myocardial effusion
- Pulmonary embolism
Metabolic
- Hyponatremia
- Hyperkalemia
- Hypocalcemia
- Hyperphosphatemia
- Hypermagnesemia
- Hyperuricemia
Neurologic
- Asterixis
- Neuromuscular irritability
- Mental status changes
- Somnolence
- Coma
- Seizures
Gastrointestinal
- Nausea
- Vomiting
- Gastritis
- Gastroduodenal ulcer
- Gastrointestinal bleeding
- Pancreatitis
- Malnutrition
Hematologic
- Anemia
- Hemorrhagic diathesis
Infectious
- Pneumonia
- Septicemia
- UTI
- Wound infection
3) List the causes of prerenal azotemia
Box 87.2
Volume loss
- GI losses
- Renal (diuresis)
- Blood loss
- Insensible losses
- Third-spacing sequestration
- Pancreatitis
- Peritonitis
- Trauma
- Burns
Cardiac causes
- Myocardial infarction
- Valvular disease
- Cardiomyopathy
- Decreased effective arterial volume
- Antihypertensive medication
- Nitrates
Neurogenic causes
- Sepsis
- Anaphylaxis
- Hypoalbuminemia
- Nephrotic syndrome
- Liver disease
4) Compare laboratory test differences between pre-renal azotemia and Intrinsic AKI
| Pre Renal | Intrinsic | Post | |
| BUN : Cr (ratio) | Usually >20 | 10-20 | 10-20 |
| Urine Na (mEq/L) | <20 | >30 | <20 early >40 late |
| FENa (%) | <1 | >2-3 | < 1 early >3 late |
| Urine Osm (mOsm/kg) | >350 | ~300 | >400 ealry 300 late |
| Urine Specific Gravity | >1.020 | ~1.010 | >1.010 early <1.010 late |
| Urine Micro | Normal +/- hyaline casts | ATN: Hyaline casts w/ dark granular casts, renal epi cells or casts | Normal +/- hyaline casts or granular casts |
5) List the intrinsic renal diseases that cause AKI
Box 87.4
Vascular Diseases
Large-Vessel Diseases
- Renal artery thrombosis or stenosis
- Renal vein thrombosis
- Atheroembolic disease
Small- and Medium-Sized Vessel Diseases
- Scleroderma
- Malignant hypertension
- Hemolytic uremic syndrome
- Thrombotic thrombocytopenic purpura
- HIV-associated microangiopathy
Glomerular (Systemic) Diseases
- Systemic lupus erythematosus
- Infective endocarditis
- Systemic vasculitis
- Henoch-Schonlein purpura
- HIV-associated nephropathy
- Essential mixed cryoglobinemia
- Goodpasture’s syndrome
Primary Renal Diseases
- Poststreptococcal glomerulonephritis
- Other postinfectious glomerulonephritis
- Rapidly progressive glomerulonephritis
Tubulointerstitial Diseases and Conditions
- Drugs
- Toxins
- Infections
- Multiple myeloma
Acute Tubular Necrosis
- Ischemia -> Shock, sepsis, severe pre-renal azotemia
- Nephrotoxoins -> Antibiotics, radiographic contrast agents, myoglobinuria, hemoglobinuria
Other Diseases and Conditions
- Severe liver disease
- Allergic reactions
- NSAIDs
6) List the RFs for contrast induced ATN
According to LITFL here
Top 3:
- Pre-existing renal disease (especially Cr >120)
- Diabetes mellitus
- Age >75yrs
Others:
- CHF
- Hypertension
- Hypovolemia
- Nephrotoxins (NSAIDs, cyclosporin, aminoglycosides, amphotericin)
- High dose contrast, intra-arterial worse than IV
- Cirrhosis/nephrotic syndrome
- Multiple myeloma
- PVD
- High uric acid and hypercholesterolemia
7) List the causes of postrenal renal failure
Box 87.3
Intrarenal and Ureteral Causes
- Kidney stone
- Sloughed papilla
- Malignancy
- Retroperitoneal fibrosis
- Uric acid, oxalic acid, or phosphate crystal precipitation
- Sulfonamide, methotrexate, acyclovir, or indinavir precipitation
Bladder
- Kidney stone
- Blood clot
- Prostatic hypertrophy
- Bladder carcinoma
- Neurogenic bladder
Urethra
- Phimosis
- Stricture
8) List the causes of pigment induced AKI
Box 87.5
Rhabdomyolysis and myoglobinuria
- Crush injury
- Compartment syndrome
- Electrical injury
- Myonecrosis from coma or immobilization
- Acute arterial occlusion
- Vigorous exertion
- Status epilepticus
- Hyperthermia/heat stress
- Metabolic myopathy
- Drugs/toxins
- Hypokalemia
- Hypophosphatemia
Hemoglobinuria
- Acute hemolysis
- Transfusion reaction
- Infections
9) List causes of hematuria, what are the most common?
Think:
UTI
Stones
Exercise Induced
Trauma
Endometriesis
Cancer
PCKD
Glomerular Disease
According to UptoDate:


10) List complications of AKI
Spaced repetition! Essentially the same as questions 1, but here is another way of thinking about it
Checkout the CCC at LITFL here
- Volume overload – CHF, HTN
- Metabolic acidosis
- Hyperchloraemia
- accumulation of organic anions – PO4
- decreased Alb -> decreased buffering
- impaired insulin action -> hyperglycaemia
- catcholamine resistance (bAR downregulation)
- increased iNOS
- Electrolytes – increased K+ and low Na+
- Pulmonary oedema – low albumin -> decreased oncotic pressure + volume overload
- ALI – neutrophil activation and sequestration in the lung
- Uraemia (ALOC and pericarditis)
- Immune – decreased clearance of oxidant stress, tissue oedema, WCC dysfunction – increased risk of infection
- Haematological – decreased RBC synthesis and increased destruction of RBC -> anaemia, decreased EPO, platelet dysfunction secondary to uremic toxins, vWF -> bleeding
- GI – GI oedema -> compartment syndrome, decreased nutritional absorption, gut ischaemia -> peptic ulcer disease
- Pharmacology – increased Vd, decreased bioavailablity, albumin, decreased elimination -> under dosing or toxicity
11) Compare and Contrast nephritic vs nephrotic syndrome
Check out this link for a more in-depth video: here

12) List the Main Causes of CKD
Box 87.6
Vascular causes
- Renal artery disease
- Hypertensive nephrosclerosis
Glomerularopathies – Primary
- Focal sclerosing glomerularnephritis (GN)
- Membranoproliferative GN
- Membranous GN
- Crescentic GN
- IgA nephropathy
Glomerularopathies – Secondary
- Diabetic nephropathy
- Collagen vascular disease
- Amyloidosis
- Post-infectious
- HIV nephropathy
Tubulointerstitial causes
- Nephrotoxins
- Analgesic nephropathy
- Hypercalcemia or nephrocalcinosis
- Multiple myeloma
- Reflux nephropathy
- Sickle cell nephropathy
- Chronic pyelonephritis
- Tuberculosis
Obstructive Causes
- Nephrolithiasis
- Ureteral tuberculosis
- Retroperitoneal fibrosis
- Retroperitoneal tumor
- Prostatic obstruction
- Congenital abnormalities
Hereditary Causes
- Polycystic kidney disease
- Alport’s syndrome
- Medullary cystic disease
13) List the reversible and treatable causes of CKD
Box 87.7
Reversible Factors
- Hypovolemia
- CHF
- Pericardial tamponade
- Severe hypertension
- Catabolic state, protein loads
- Nephrotoxic agents
- Obstructive disease
- Reflux disease
Treatable Causes
- Renal artery stenosis
- Malignant hypertension
- Acute interstitial nephritis
- Hypercalcemic nephropathy
- Multiple myeloma
- Vasculitis
- Obstructive nephropathy
- Reflux nephropathy
14) List the mechanisms of drug toxicity in CKD
Box 87.8
- Excessive drug level
- Impaired renal excretion of drug
- Impaired renal excretion of metabolite
- Impaired hepatic metabolism
- Increased sensitivity to drug
- Changes in protein binding
- Changes in volume of distribution
- Changes in target organ sensitivity
- Metabolic loads administered with drug
- Misinterpretation of measured serum drug level
15) List four major complications of CKD and their management
A) Hyperkalemia (see Table 87.1 for dose/moa/details)
- Calcium gluconate
- Albuterol
- Glucose & insulin
- Sodium bicarbonate
- Dialysis
- IV diuretics
B) Bleeding
Likely platelet dysfunction secondary to uremia:
Desmopressin 0.3-0.4mcg/kg (max dose 20mcg)
C) Pulmonary edema
IV nitro glycerin and NIPPV
Dialysis
D) Infection
Sepsis workup including blood cultures (peripheral and off any lines)
Consider advanced imaging of fistulae (especially in Prosthetic bridge fistula)
Big guns for antibiotics (Cipro and Septra for UTI, or Ceft and vanco for unwell)
E) Hypocalcemia
Aysmptomatic = Not urgent
Tetany: IV Calcium (gluconate peripheral or chloride central)
F) Hyperphosphatemia
Calcium-based antacids that bind ingested phosphate in the gut
dialysis
G) Hypermagnesemia
Stop laxatives and Mg replacement.
Dialysis
[bg_faq_end][bg_faq_start]16) Compare the mechanisms of dialysis in HD and PD
The basis of all dialysis is having the patient’s blood come in contact with a semi-permeable membrane.
In IHD, that membrane is external to the patient and thus via venous access, we remove their blood and return it post filtration.
In peritoneal dialysis the patient’s peritoneum acts as the membrane. The dialysate is pumped into the patient’s abdomen via a Silastic catheter.
[bg_faq_end][bg_faq_start]17) List indications for emergency dialysis
Box 87.9
- Pulmonary edema
- Severe uncontrollable hypertension
- Hyperkalemia
- Other severe electrolyte or acid-base disturbances
- Some overdoses
- Pericarditis (possibly)
18) List complications of hemodialysis
Vascular Access–Related Complications
Occlusion
Bleeding
Infection
Non–Vascular Access–Related Complications
Hypotension (see next question)
Bleeding (pericardial, pleural, GI, ICH, abdominal, retroperitoneal)
VTE
CAD
Neurologic Dysfunction (disequilibrium syndrome)
[bg_faq_end][bg_faq_start]19) List DDx for Hypotension in the hemodialysis patients
Box 87.10
- Hypovolemia
- Excessive fluid removal
- Hemorrhage
- Septicemia
- Cardiogenic shock
- Dysrhythmia
- Pericardial tamponade
- Myocardial infarction
- Myocardial or valvular dysfunction
- Electrolyte disorders
- Hyperkalemia or hypokalemia
- Hypercalcemia or hypocalcemia
- Hypermagnesemia
- Vascular instability
- Drug-related
- Dialysate-related
- Autonomic neuropathy
- Excessive access arteriovenous flow
- Anaphylactoid reaction
- Air embolism
20) List causes of altered mental status in dialysis patients
Box 87.11
Structural Conditions
- Cerebrovascular accident
- Subdural hematoma
- Intracerebral abscess
- Brain tumor
Metabolic Conditions
- Disequilibrium syndrome
- Uremia
- Drug effects
- Meningitis
- Hypertensive encephalopathy
- Hypotension
- Postictal state
- Hypernatremia or hyponatremia
- Hypercalcemia
- Hypermagnesemia
- Hypoglycemia
- Severe hyperglycemia
- Hypoxemia
- Dialysis dementia
21) Describe the management of peritonitis in the PD patient
Likely SBP
Send dialysate of catheter (sterile technique) if :
- >100 WBCs/mm3 peritoneal fluid
- >50% neutrophils
- Positive Gram staining
If fluid is normal then consider ruling out surgical cause
IP antibiotics: Vanco and ceftazidime or cefepime
Consider adding Heparin 500 to 1000 units to dialysate bag to decrease fibrin formation and subsequent obstruction of catheter
Wisecracks
[bg_faq_start]1) How do NSAIDs cause AKI?
- Blocking prostaglandin = decreased glomerular perfusion = decreased GFR
- This can happen in patients with normal intravascular volume and normal glomerular perfusion! (includes all NSAIDs, and Aspirin)
- Direct interstitial nephritis
- Direct papillary necrosis.
2) Describe the likely pathophysiologic etiology of the following casts
- Hyaline Casts: Acellular think pre or post renal
- Red Cell Casts: Glomerular disease (ie nephritic syndrome)
- White Cell Casts: Interstitial disease (ie pyelonephritis or AIN)
- Granular Casts: Tubular disease (ie ATN)
- Fatty Casts: nephrotic syndrome
This post was uploaded and copyedited by Colin Sedgwick (@colin_sedgwick)