This episode of CRACKCast covers Rosen’s Chapter 96, Anorectal Disorders. These complaints are sensitive in nature and are not easily volunteered by patients. A sensitive and thorough history is necessary to help resolve these complaints that can be devastating to quality of life.
Shownotes – PDF Here
[bg_faq_start]Rosens in Perspective
These conditions are extremely embarrassing and have a HUGE impact on our QOL!
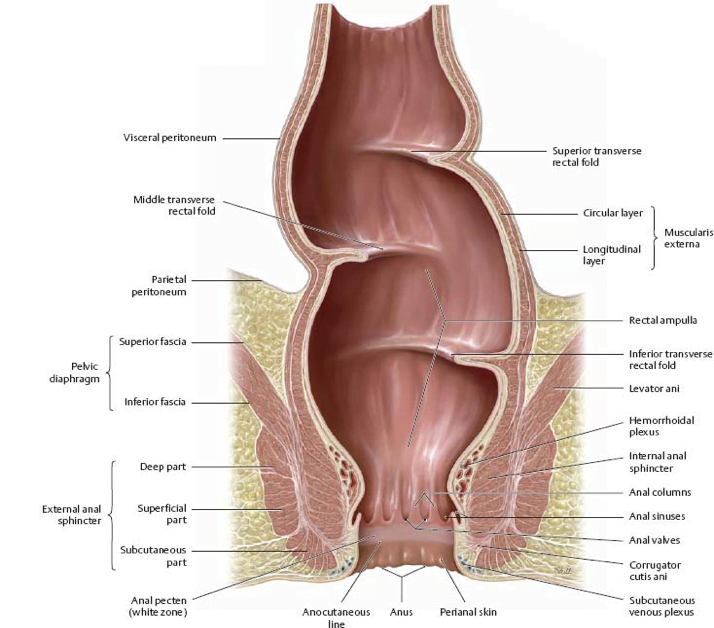
Copied from: http://doctorlib.info/medical/anatomy/15.html
Describe the neurologic control of defecation.
So, normal defecation is a balance between the PNS and SNS. Sympathetic fibers (L1-5) inhibit the contraction of rectal smooth muscle in the upper rectum and lower rectum and L5 fibers cause the internal sphincter to contract.
- Parasympathetic fibers (lower down at S2-S4) cause the rectal wall to contract, AND the internal sphincter to relax.
- The external sphincter – has voluntary control via S2,3,4. The sensation of rectal fullness depends on intact parasympathetic fibers.
- Sympathetic works = squeezes things “in”
- Parasympathetic works to = PUSH things “out”
Defecation depends on rectal distension, internal sphincter relaxation (involuntary) and stool entering the anal canal. Then at the appropriate time there is voluntary relaxation of the external anal sphincter
What is the pathophysiology of haemorrhoids?
- Form when three “anal vascular submucosal cushions become engorged.” They are normal structures and show up when the muscularis submucosa (the cushioning lining if the anal canal) becomes weak. Then the anal cushions get displaced distally.
- Important to know the anatomy for hemorrhoids: superior, middle, and inferior hemorrhoidal arteries provide the blood supply to the anorectum. (Hemorrhoids form from ARTERIAL BLOOD SUPPLY and are unrelated to portal hypertension in adults).
Hemorrhoids are NOT varicose veins. Patients with portal hypertension have rectal varices — which are different than hemorrhoids.
Key historical features for anorectal disorders:
- Bleeding,
- Swelling
- Pain
- Itching
- Discharge
- Incontinence
- Hx of radiation
- Hx of sexual practices involving the rectum/anus
- Hx of IBD, cancer, polyps, straining activities, diabetes
See figures 86.1 and 86.2 in 9th edition of Rosens for Anorectal anatomy and an algorithm for anorectal complaints.
[1] What are risk factors for the develop of symptomatic haemorrhoids?
Usually we think about hemorrhoids as being either external (bright red, painful, blood on toilet paper) vs. internal (bright red, painless, drips in the toilet bowl or is streaked in with the stool). The external ones originate distal to the dentate line and are covered in anoderm (MSE). The Internal ones originate proximal to the dentate line and are covered in mucosa. HOWEVER, people can have mixed type hemorrhoids too!
Risk fx:
- Family hx of hemorrhoids
- Straining and constipation
- Pregnancy & traumatic deliveries
- Prolonged sitting
- Heavy lifting
- Portal hypertension (technically these are rectal varices though!)
Key pearl here is that: blood mixed in with the stool = rectal source. Bloody mucous should make you think of cancer, IBD and proctitis.
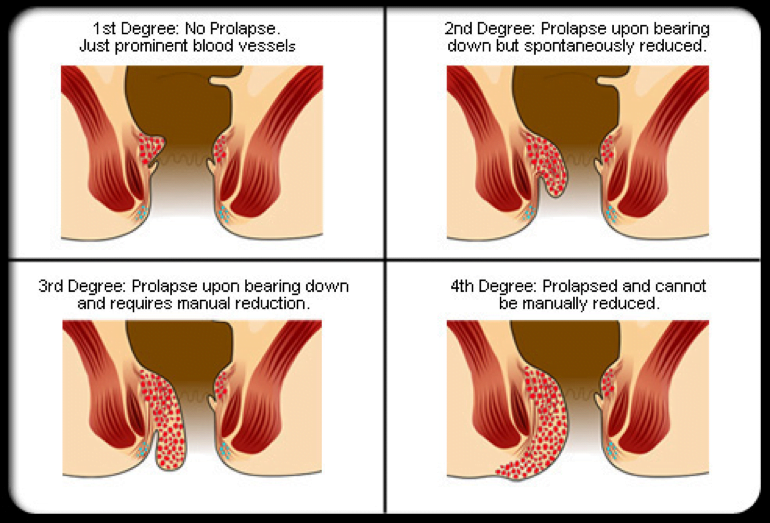
[2]Describe 4 degrees of internal hemorrhoids and indicated management options
Copied from: http://symptoms-of-hemorrhoids.net/internal-hemorrhoids/
See Table 86.2 in Rosens for Classification of Internal Hemorrhoids by severity.
- 1st and 2nd degree are managed medically (see next question); although some may benefit from in-office surgical treatment (sclerotherapy, banding)
- 3rd degree are managed medically with the option of surgery
- 4th degree require surgical repair!
There is one type of hemorrhoid that requires urgent surgical repair: watch out for the 4th degree, acute gangrenous, thrombosed internal hemorrhoid.
[3] Describe the management of non-thrombosed external haemorrhoid & thrombosed external hemorrhoids
| Non-thrombosed external haemorrhoids | Thrombosed external haemorrhoids |
| Usually it is these that cause people to come to the ER – because they HURT! | |
| Managed Medically using the WASH approach. ● Warm water sitz ● Analgesia ● Stool softeners ● High fiber diet
See below | Usually can be managed supportively as well. (they will ulcerate and ooze dark blood in a few days).
But, if within 72 hrs of onset of symptoms, they can have the clot EXCISED. Be sure to warn patients that excision will lead to evacuation of the clot, but also rebleeding, swelling and the formation of a skin tag.
People that are bad candidates for this: kids, pregnant women, immunocompromised patients.
Rosen’s does mention that an alternative non-surgical therapy: ● Topical nifedipine 0.3% ● Topical lidocaine gel 1.5%
+ Excision procedure: ● Anesthetic field block ● Elliptic incision (single crescent shaped) made on the hemorrhoid and over top of the clot) ● Clot is removed. |
Hemorrhoid management:
- WASH approach
- Warm water sitz baths (ideally with epsom salts)
- Water > 40 degrees C helps decrease anal canal pressures (a shower stream can also work).
- 5-10 mins BID-QID prn
- Analgesics
- NSAIDS, tylenol (but can be constipating)
- Topical anesthetics (1-2% lidocaine gel)
- Topical corticosteroids (only apply for 1-2 days! – e.g. anusol HC)
- Topical nitroglycerin (helps decrease internal sphincter spasm)
- Witch hazel
- Mineral oils (ANUSOL over the counter)
- Cocoa butter
- Stool softeners
- PEG 3350
- Sennokot
- High fiber diet
- Oats, broccoli, beans, whole grains, celery, peanuts, and others
- Fiber supplement
- Warm water sitz baths (ideally with epsom salts)
[4] List causes of fissures. Which type of fissure is suspicious for underlying disease?
Typically sharp, sudden onset anorectal pain with no swelling and some bleeding onset during defecation. Usually caused by a hard stool tearing the anoderm. Most people then describe nagging burning pain, and spasm pain with any attempt to pass a bowel movement.
- Usually occurs in the posterior midline (anterior midline in women).
Causes:
- Constipation (especially in infants and kids)
- Straining
- Prolonged diarrhea
- Vaginal delivery
- Anal sex
- Secondary causes.
A fissure anywhere other than posterior/anterior should make you suspicious for:
- Leukemia
- Crohn’s disease
- HIV infection
- TB
- Syphilis
(these are usually heralded by coexisting sentinel pile).
[5] Describe the treatment of anal fissures – 5 options
WASH regimen
- Nitro. Ointment 0.4% bid/tid
- Nifedipine gel 0.2% bid with lidocaine gel 1.5%
- Surgical options (botox, anal dilation, excision).
- Most take 2-4 weeks to resolve.
See question 3 above for a detailed explanation of the WASH approach.
[6] Which conditions are associated with the development of abscesses and fistulas?
Thought to occur in healthy adults when the glands at the anal crypts occlude with an associated condition (IBD, trauma, cancer, radiation, infection).
Here’s the full list:
- IBD
- Trauma
- Cancer
- Radiation injury
- Infection
- TB
- Lymphogranuloma venereum
- Usually staph. A.; E coli; streptococcus; proteus; bacteroides
Usually abscesses progress to fistulae. A fistula is a connection between two epithelium lined surfaces. Some predisposing conditions:
- Abscess
- Crohn’s disease
- Trauma
- Foreign body reactions
- TB
- Cancer
Don’t probe fistula tracts in the ER. They need definitive fistulectomies or fibrin glue applications by a colorectal surgeon (unless the patient has Crohn’s disease).
[7] List 5 types/sites of anorectal abscess. Which can be drained in ER?
The treatment for all of these is incision and drainage! Visual inspection is often misleading – because pain usually precedes redness, swelling and fluctuance.
- SUPRALEVATOR ABSCESS
- pts usually have fever and leukocytosis
- Often no external signs
- often obese/diabetic/crohn’s/PID
- Need surgery
- INTERSPHINCTERIC ABSCESS
- Deep to the external sphincter; and inferior to the levator ani
- Symptoms: continuous rectal pressure and throbbing pain.
- Often have associated fistula and inguinal lymph nodes
- Need surgery
- ISCHIORECTAL ABSCESS
- Form the in space outside the anal sphincter
- May have no visible external findings – despite patient complaints of severe pain.
- Usually surgical drainage (some may be drained in the ER)
- POSTANAL ABSCESS
- occur posterior to the rectum.
- often in severe, constant pain in the coccyx
- Often missed, need surgical drainage.
- PERIANAL ABSCESS
- Most common type
- Present with a painful perianal mass
- Located outside the anal verge
- The only one that can be consistently drained in the ER
- Antimicrobial therapy post I+D may be indicated if the patient is
- Immunocompromised
- Diabetic
- Valvular heart disease
- Associated cellulitis
- People should be instructed on wound care following the procedure and use the WASH regimen
From Rosen’s 9th Ed., see table 86.4 for more details on abscesses of the Anorectum and figure 86.6 for locations of common anorectal abscesses.
A couple other notable infections…..
- Horseshoe abscess
- Large, communicating abscess – forms in the deep spaces. Needs surgery
- Necrotizing infection
- Eg. necrotizing fasciitis, Fournier’s gangrene, tetanus
[8] What is a pilonidal cyst? How do you treat it?
These are abscesses containing hair in the midline of the sacrococcygeal area. Bacteria enter the hair follicle and inflame the area which form a microabscess. This then perforates in the subcutaneous tissue and forms a bigger abscess in the presacral area.
They aren’t true cysts, in that they are not fully epithelialized.
Usually affect young males < 40 yrs of age who are obese and hirsute (hairy); prolonged peroids of sitting, a deep natal cleft, family hx. What they are not: anal fistulae, perirectal abscesses, hidradenitis suppurativa, granulomatous syphillis/TB.
Management:
- Prevention (ideally) with good hygiene, epsom salts, ventilated clothing, etc.
- Incision and drainage of acute abscesses
- TECHNIQUE: a longitudinal incision LATERAL to the midline.
- Add antibiotics if associated cellulitis present
- Ideally refer to a surgeon for wide excision.
[9] List 8 causes of fecal incontinence.
Can be partial (liquid stool and gas sneaks past) or complete (unable to control passage of solid feces). Big categories of causes:
- Traumatic
- Spinal cord injury
- Post surgical or obstetric injury
- Neurologic
- Diabetes
- Hirschsprung’s disease
- Spinal cord lesions (cancer, ischemia, infection)
- Mass effects
- Anorectal cancer
- Foreign body / fecal impaction / hemorrhoids
- Medical
- Diarrhea / laxative abuse
- Dementia
- Pediatric patients
- Congenital, meningocele, spina bifida
- Other causes
- Post-corrective surgery for an imperforate anus
- Sexual abuse
- Encopresis (young children experiencing emotional stress).
[10] List 8 causes of pruritus ani
An uncontrollable urge to scratch the anal area, usually caused by perianal irritation. More common in the midnight summer…
Causes:
- Focal Dermatitis
- Feces on the perianal skin fecal irritation
- Usually associated with obesity, deep perineal clefts, hair, hemorrhoids, skin tags, fistulae,
- Poor hygiene – tight non-breathable clothing
- Systemic causes:
- Tea, coffee, beer, spicy foods, citrus fruits, IV hydrocortisone, colchicine, tetracyclines.
- Contact dermatitis from topical anesthetics (lidocaine), topical corticosteroids, perfumed soap
- Feces on the perianal skin fecal irritation
- Systemic diseases
- Derm:
- Psorasis
- Lichen sclerosus
- Non-Dermatologic
- Pruritis prone diseases:
- Liver failure, renal failure
- Myxedema, DM, thyrotoxicosis
- Vitamin A, D deficiency, iron deficiency
- Cancer – hodgkins or paget’s disease
- Pruritis prone diseases:
- Derm:
- Infections
- STDs
- Syphilis
- HSV
- HPV
- Others
- Scabies
- Permethrin 5%, then reapply in 2 weeks
- Pinworm (look for this in young children)
- Tape trick
- Treatment:
- Mebendazole 100 mg PO
- (or pyrantel pamoate 11 mg/kg (max 1 g) po) with a repeat in 2 weeks.
- Bacterial / fungal infection
- Scabies
- STDs
Here’s a helpful ROSENISM:
- ITCH:
- Infection
- Topical irritants
- Cutaneous conditions
- Hypersensitivity to foods or drugs!
[11] Describe 6 rectal STI’s and their management
Important to ask about this on your ano-rectal hx! Ask regarding “any activity outside using the washroom that involves the anorectal area?” if yes get the specific details. This is important because semen is known to have a concentrated HIV load and the anorectum is high risk area for the portal of entry of HIV.
See table 86.5 for a breakdown of these conditions into ulcerative vs. nonulcerative presentations. As well as their treatment!
- Gonorrhea (neisseria)
- Ceftriaxone 250 mg IM / Cefixime 400 mg PO x1 dose
- Chlamydia and lymphogranuloma venereum (LGV)
- Need antibody tests to find it because rectal cultures are inaccurate
- Doxycycline 100 mg PO BID x 7 days (21 days if for LGV)
- Or azithromycin 1 g po once for chlamydia
- Syphilis
- Primary (may be falsely confused as an anal fissure!): benzathine Penicillin G. 2.4 Million units IM x 1
- Secondary (condyloma latum – smooth, raised, painless wart-like lesions that weep fluid and smell foul): benzathine Penicillin G. 2.4 Million units IM x 1
- Condyloma acuminatum – HPV – (genital warts)
- All these patients should be tested for HIV
- Ddx: condyloma latum (secondary syphilis), squ.cell.CA.
- Podofilox 0.5% topically or cryotherapy
- Herpes simplex virus
- 1st episode double the dose of acyclovir TID for 7-10 days
- Recurrent:
- Acyclovir 200 mg po five times per day for 7-10 days
- Valacyclovir 1 g PO daily for 7-10 days
6. Chancroid (diagnosis of exclusion)
- Ceftriaxone 250 mg IM
- Or azithromycin 1 g po once
7. Ulcerative lesions in HIV patients
- Complex, and either:
- Routine anorectal diseases affecting the rest of the population
- STDs
- Opportunistic infections:
- TB, CMV, cryptococcus, lymphoma, kaposi’s sarcoma, SCC
[12] List conditions associated with rectal prolapse.
- Aka PROCIDENTIA
- Affects the very young and very old
- Elderly women with uterine or urethral prolapse
- Young children with chronic constipation or diarrhea
- May also occur with CF, parasitic infections, malnutrition
- Reduction:
- Apply dextrose/sucrose soaked gauze x 5-10 mins, then gentle pressure to coax the rectum back into the body
- Prevention:
- Increase dietary fibre
- Increase fluid intake
[13] Describe the ED management of rectal foreign bodies
Affects children; people who use the anus for sexual gratification; psychiatric patients; victims of assault; body stuffers/packers.
- We need to remove them due to the risks of mucosal lacerations, perforation, obstruction, sepsis, peritonitis.
- Important things for us to know about:
- Fever, abd. peritonitis, rectal bleeding, duration of FB
- Should get an upright abd. Xray if it is radio-opaque
- If you suspect a perforation: try using water soluble rectal contrast to outline the foreign body
- Management:
- Ask the patient to assist with valsalva
- Use benzo’s to help with rectal relaxation
- Suprapubic pressure can assist with removal
- Consider foley catheter to remove the suction – negative pressure proximally
- Some need deep procedural sedation or operative removal
Wisecracks:
[1] What is hidradenitis suppurativa?
- An infection of the apocrine glands in young adults with poor hygiene, hyperhidrosis, obesity, acne, diabetes, smoking).
- Usually the apocrine ducts are infected with Staph, Strep, E coli or proteus.
- Usually multiple small draining pustules in the intertriginous areas. May have surrounding lymphadenopathy, folliculitis, and cellulitis
- Ddx includes sebaceous cysts, furuncles, and granulomas, and Crohn’s dz.
- Management
- Good hygiene, warm compresses
- Antibiotics
- Dietary changes: low sugar diet.
- Large lesions can be drained, but the recurrence rate is 40%.
- May need wide surgical excision.
[2] What are levator ani syndrome and proctalgia fugax?
These are two unique causes of proctalgia (anorectal pain) other than the conditions listed in the previous questions. They are both benign, but affect QOL
- Levator Ani Syndrome
- Constant dull pressure in the sacrococcygeal region post defecation or long periods of sitting.
- Anecdotal treatment: sitz baths, levator ani muscle massage, and muscle relaxants
- Proctalgia Fugax – charley horse of the anus
“…an intensely painful spasm in the rectal area that begins abruptly and lasts up to 30 minutes, resulting from a sudden spasm of the levator muscle complex or sigmoid colon. Professionals, managers, perfectionists, and people who frequent the toilet are more likely to be affected. Symptoms begin abruptly during sleep, defecation, urination, or intercourse. The nature of the pain has been compared to that of charley horse (painful spasms in the leg muscles) and may radiate to the coccyx or perineum. Each patient has a unique but recurrent constellation of symptoms. Treatment includes a bowel-cleansing regimen, upward manual pressure on the anus, diazepam, and topical Nitrates.” – From Rosen’s 9th Ed.
[3] Radiation proctitis:
- Always ask patients with anorectal complaints about previous radiation.
- Symptoms can show up acutely (2 weeks) or chronically (up to 2 hrs post exposure!).
- Common complaints of pain, bleeding, irritation, etc.
- Dx is made with a biopsy
- Management:
- Supportive
- WASH regimen
- Botox injections
- Enemas with short chain fatty acids
- PO sucralfate
- Sclerosing therapy
- Hyperbaric O2
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)