This episode of CRACKCast covers Rosen’s Chapter 92 for the 8th Edition (Chapter 82 9th Edition), Small Intestine. This chapter covers the various pathologies, diagnoses and treatments of the Small Intestine.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Mortality for small bowel obstruction used to be around 60%, but is now in the 8% range!
- Pathophysiology of small bowel obstruction:
- Bowel gets kinked – leads to a backup of intestinal contents and secretions. This leads to temporary increase in peristalsis (initially loose BM’s, N/V).
- Then the bowel becomes edematous and absorptive functions cease
- Then bowel develops bacterial overgrowth
- Development of transudative fluid loss (hypovolemia, metabolic alkalosis, shock)
- **in a closed loop obstruction the fluid contents increase in pressure much more rapidly (no antero/retrograde flow). This can lead to necrosis and perforation**
Blood supply to the gut is key! The celiac trunk (foregut – distal esophagus to the duodenum at the entrance of the bile duct) superior mesenteric artery (midgut – distal half of the duodenum to the proximal two-thirds of the transverse colon) and inferior mesenteric artery (hindgut – distal third of the transverse colon to the rectum) are the major arterial blood vessels.
[bg_faq_end] [bg_faq_start]Question 1) List the types of mechanical small bowel obstruction.
Let’s quickly talk through the classification systems; there are at least four categories of SBO.
- Mechanical obstruction:
- “presence of a physical barrier to the movement of the intestinal contents”; classified as either:
- External
- Internal ….more on these below!
- Neurogenic / functional obstruction:
- Disruption of the normal peristaltic activity in the absence of a physical blockage in the lumen.
- Pseudo-obstruction: poorly understood/complex syndrome, similar symptoms and signs to mechanical obstruction without a mechanical lesion. Thought to be due to disruption of intestinal pacemaker cells (Interstitial cells of Cajal). “These cells regulate the contractility of the intestinal smooth muscle and are under the influence of the enteric nervous and autonomic systems. Pathology at any one of these sites can lead to pseudo-obstruction. Causes include degenerative neuropathies, autoimmune and paraneoplastic disease, and hereditary conditions. The symptoms of pseudo-obstruction are often chronic and respond poorly to treatment.” – From Rosen’s 9th Ed.
- Closed loop vs. open loop
- An open loop (or simple) obstruction = blockage at one point only (e.g. someone pinching a garden hose).
- A closed loop obstruction = TWO locations are pinched off. This creates a section of ischemic bowel
- E.g. internal hernia (mesentery twists on itself) → twice the mortality rate due to necrosis.
- “presence of a physical barrier to the movement of the intestinal contents”; classified as either:
Question 2) What are potential etiologies of mechanical small bowel obstruction?
External = compress the gut from the outside, preventing peristalsis
- Adhesions (scarring post-op) > 60%
- Hernias (internal or external)
- Volvulus
- Usually occurs in the normal abdominal cavity; may have increased incidence during Ramadan; small bowel volvulus can commonly occur in children < 1 month of age
- Compressing masses (tumours, abscess, hematomas)
Internal = something stuck inside!
- Primary intra-intestinal neoplasm (e.g. polyp)
- Inflammatory strictures (Crohn’s disease, radiation enteritis)
- Infectious causes (intestinal TB)
- Intussusception
- #1 cause of intestinal obstruction in kids aged 6 months – 36 months.
- Ileocolic intussusception = non-operative treatment with enema or watchful waiting
- Small bowel intussusception = usually needs surgery
- Usually a mechanical cause is found in adult cases!
- #1 cause of intestinal obstruction in kids aged 6 months – 36 months.
- Hematoma of the wall (due to trauma)
- Bezoars
- Ingested foreign bodies
- Gallstone ileus
- Ascaris infestation
We’ll mention the HAMMER a NAIL mnemonic in the wisecracks!
Top three causes:
- Adhesions
- Tumours (adenocarcinomas, carcinoid tumors, lymphomas, and sarcomas, and benign conditions, including adenomas, leiomyomas, and lipomas; metastatic disease, ovarian cancer.)
- Hernias
- Be worried about the closed loop internal hernia – in someone post bariatric surgery!
Question 3) List causes of functional small bowel obstruction.
- Metabolic disease (especially hypokalemia)
- Medications (eg. narcotics)
- Infection (retroperitoneal, pelvic, intrathoracic)
- Abdominal trauma
- Laparotomy
Question 4) List 5 lab tests useful in the diagnosis of SBO. What findings are expected on AXR? On CT?
This is a trick question….or one from the old edition. The 9th Ed. of Rosen’s only lists two lab tests that can be used. An elevated serum lactate and CPK – can suggest a bowel obstruction with strangulation if its late in the disease process. So, add these tests on if you’re at all suspicious – but know that a normal level won’t rule the disease out! WBC, HCT, creatinine and others aren’t even mentioned! (but may suggest a degree of dehydration).
X-ray:
- Used to be the standard test – views are supine and upright views +/- decubitus views
- Usually only diagnostic in 50-60% of cases, and equivocal in 30%
- Findings:
- More than 3 Distended bowel loops > 3 cm in diameter (usually centrally)
- No gas is usually seen in the large bowel – unless it is early in the disease or it’s a partial SBO
- Dilated loops of small bowel proximal to the obstruction
- Predominantly central dilated loops
- Valvulae conniventes are visible
- Air-fluid levels if the study is erect, especially suspicious if
- >2.5 cm in length
- in same loop of bowel but at different heights
- An adynamic ileus = shows extensive air-filled loops throughout the entire GI system and NO small bowel dilation
- Rule of 3’s:
- > 3 air fluid levels, > 3 instances of > 3 cm dilation
CT: This is the GOLD standard diagnostic test
- Tells us more about the cause of the obstruction! And they can tell us if there are signs of strangulation (with IV contrast)
From Radiopaedia, features on CT may include:
- dilated small bowel loops >2.5-3 cm from outer wall to outer wall
- normal calibre or collapsed loops distally
- small bowel faeces sign (https://radiopaedia.org/articles/small-bowel-faeces-sign-bowel)
Closed-loop obstructions are diagnosed when a bowel loop of variable length is occluded at two adjacent points along its course. May be partial or complete with characteristic features:
- Radial distribution of several dilated, fluid-filled bowel loops
- Stretched of prominent mesenteric vessels converging towards the point of torsion
- U-shaped or C-shaped configuration
- beak sign at site of fusiform tapering
- whirl sign reflecting rotation of bowel loops around a fixed point
Strangulation is defined as closed-loop obstruction associated with intestinal ischaemia. Mainly seen when the diagnosis is delayed (up to 10% of small bowel obstructions) and associated with high mortality. Features are non-specific and include:
- thickened and increased attenuation of the bowel wall
- halo or target sign
- pneumatosis intestinalis
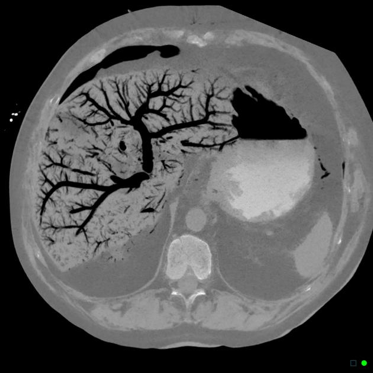
- portal venous gas
- localised fluid or haemorrhage in the mesentery
Positive oral contrast is NOT usually necessary for the diagnosis of small bowel obstruction
[bg_faq_end] [bg_faq_start]Question 5) Describe the acute management of SBO.
- A) Hemodynamically stable
- If yes, go on
- If no, then fluid resuscitation with balanced crystalloid solution
- Don’t forget to replace electrolytes
- B) Early surgical consultation if bowel strangulation / closed loop / surgical abdomen secondary to perforation
- C) NG placement: only if N/V uncontrolled with modern day antiemetics or ALOC with risk of aspiration (make sure you decompress that hostile abdomen if you need to intubate!!!) Dogmalysis!
- D) Antibiotics in the sick, hypotensive or rigid abdomen (think gram negative and anaerobic coverage: eg. 2nd gen cephalosporin or carbapenem)
- E) NPO for complete bowel obstruction, fluids only for partial
- F) Pain control
Question 6) What are the potential complications of a small bowel obstruction?
- Hypovolemia / Shock
- Persistent N/V with inability to tolerate PO intake
- Metabolic alkalosis (contraction and loss)
- Perforation leading to peritonitis
- Intrabdominal abscess
- Sepsis
- Death
Surgical complications:
- Infection
- Short Gut syndrome
- Recurrent SBO (40% non operative vs 27% operatively)
Question 7) List the 4 primary types of mesenteric ischemia. For each describe 4 associated factors/etiologies.
“Acute mesenteric ischemia involves the sudden reduction or loss of blood flow to the small bowel and may also involve the right colon. The left colon has a much higher degree of collateral blood flow and is less prone to mesenteric ischemia.”
Remember that patients can have chronic mesenteric ischemia, and intestinal angina post-prandially, but here we’re talking about AMI!
Rare, but devastating!!! Mortality remains 60-80%. By 6 hours of ischemic time to the small bowel, transmural necrosis is complete
All these lesions are out to get the jejunum!
| Type | Etiology | Risk factor |
| Mesenteric arterial embolus | Arterial emboli make up 50% of cases (think left sided atrial/vent/valvular source) The SMA is the most common vessel occluded. | -Age >70 -Female>>Male -MI -cardiomyopathies -ventricular aneurysms -endocarditis -atrial fibrillation |
| Mesenteric arterial thrombosis | Rupture of atheromatous plaque (think STEMI of gut) | -advanced age -hypertension -diabetes -tobacco use |
| Nonocclusive mesenteric ischemia | Vasospasm from hypoperfusion or sympathetic storm | -Hypoperfusion: sepsis, severe dehydration, pancreatitis, or hemorrhagic shock -Excessive sympathetic: CHF, vasopressors, cocaine, digoxin |
| Mesenteric venous thrombosis | Hypercoagulable state (inherited or acquired) The most common cause is Factor V Leiden mutation, which is thought to account for 20% to 40% of cases. Oral contraceptive use accounts for 9% to 18% of the episodes of mesenteric venous thrombosis in young women.
| See box 82.3 HYPERCOAGULABLE STATES -Polycythemia vera -Sickle cell disease -Antithrombin III deficiency -Protein C or S deficiency -Malignancy -Myeloproliferative disorders -Estrogen therapy, oral contraceptive pills -Pregnancy INFLAMMATORY CONDITIONS -Pancreatitis -Diverticulitis -Appendicitis -Cholangitis TRAUMA -Operative venous injury -Postsplenectomy -Blunt or abdominal trauma MISCELLANEOUS -Congestive heart failure -Renal failure -Decompression sickness -Portal hypertension |
Other weird causes:
SMA dissection leading to occlusion, tumor emboli, retroperitoneal fibrosis, and various types of vasculitis, including Buerger’s disease, polyarteritis nodosa, and Takayasu’s arteritis.
[bg_faq_end] [bg_faq_start]Question 8) Describe the classic presentation of acute mesenteric ischemia?
Traditional triad is the cardiac patient that presents with sudden onset non-localised abdominal pain and gastric emptying (vomiting or diarrhea)
*** 50% of patients with mesenteric ischemia have a prior history of embolic events !!! *** (eg. DVT, PE, Stroke)
[bg_faq_end] [bg_faq_start]Question 9) How is mesenteric ischemia diagnosed? List 4 lab abnormalities expected in acute mesenteric ischemia. List 5 findings on AXR.
CT abdo/pelvis with IV contrast is the most utilised, but mesenteric angiography is the GOLD STANDARD! Duplex U/S is not widely used due to inability to image past proximal vessel or rule out bowel infarction.
Lab:
- Leukocytosis,
- Elevated hematocrit secondary to hemoconcentration
- Metabolic acidosis.
- Biomarkers you can consider: lactate (sens 86% spec 42%), D-dimer (sens 96% spec 40%), interleukin (IL)-6,
AXR:
- Thumbprinting (credit radiopedia)

- pneumatosis intestinalis (credit radiopedia)


- portal venous gas (credit radiopedia)

Question 10) What is the management approach for the different types of mesenteric ischemia?
4 cardinal goals: 1) Restore mesenteric blood flow
2) Treat underlying condition
3) Treat underlying persistent vasospasm (if present)
4) Reduce further clot propagation
- Hemodynamic stabilisation: consider invasive arterial monitoring
- Vasopressors/Inotropes: too much Alpha (squeeze) is bad. Go for dobutamine/milrinone/dopamine.
- Epi/Norepi/Vaso have been shown to worsen mesenteric blood flow
- Antibiotics in cases of suspected infarct/perforation (Ceftriaxone or Cipro + metronidazole)
- Consider IR directed clot retrieval / stent / fibrinolytic therapy
- Evidence for the phosphodiesterase inhibitor papaverine – Increases C-AMP and causes profound smooth muscle relaxation
Wisecracks:
[bg_faq_start]Question 1) What is an adynamic ileus? List at least 5 causes.
Remember Rosen’s in Perspective? This is another name for neurogenic / functional obstruction:
- Disruption of the normal peristaltic activity in the absence of a physical blockage in the lumen.
- It is usually transient
Causes:
- Postoperative ileus (manipulation, analgesia, hormones, neurotransmitters)
- Systemic infection
This is Box 82.2 (9th Ed.):
- Metabolic disease (especially hypokalemia)
- Medications (eg, narcotics)
- Infection (retroperitoneal, pelvic, intrathoracic)
- Abdominal trauma
- Laparotomy
Here’s a mnemonic: HAMMER a NAIL:
- Hernias
- Adhesions
- Mass of Medications (bezoars, foreign bodies)
- External compression (tumour/malignancy)
- Rocks (gallstone ileus)
- Ascaris infection (and other infections)
- Narcotics (meds)
- Abdominal trauma
- Infection
- Laparotomy
Question 2) Which patients with SBO should receive antibiotics?
“There is no convincing evidence to recommend the empirical use of antibiotics for the nonoperative management of a simple SBO. In patients in whom surgical exploration is planned or perforation is suspected, antibiotics are recommended and should provide coverage against the gram-negative and anaerobic organisms that colonize the intestinal tract (eg. a second-generation cephalosporin such as cefuroxime, 1000 mg IV tid, or a broadspectrum carbapenem such as meropenem, 1000 mg IV tid).” – UpToDate 2017
[bg_faq_end] [bg_faq_start]Question 3) What are the 3 arteries supplying the GI tract? Which is the most common culprit in acute mesenteric ischemia?
Blood supply to the gut is key! The celiac trunk (foregut – distal esophagus to the duodenum at the entrance of the bile duct) superior mesenteric artery (midgut – distal half of the duodenum to the proximal two-thirds of the transverse colon) and inferior mesenteric artery (hindgut – distal third of the transverse colon to the rectum) are the major arterial blood vessels. The most common vessel involved in AMI is the SMA.
[bg_faq_end]This post was uploaded and copyedited by Andrew Guy (@andrew_s_guy)


