This episode of CRACKCast covers Rosen’s Chapter 88, DVT and PE. This episode covers the risk factors, diagnostic approach, treatment and management of PEs and DVTs.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
- This chapter is all about VTE – venous thromboembolism – as it manifests in PE’s and DVT’s.
- VTE – formation depends on excess fibrin formation (thrombin working on fibrinogen)
- Factors that enhance fibrinogen synthesis and catalysis to fibrin are:
- Systemic inflammation
- Vascular trauma (includes immune related trauma)
- Inherited thrombophilias
- Hemoglobinopathies
- Cancer
- Pragnancy
- Sluggish blood flow
- The triad:
- Venous injury
- Slow blood flow
- Hypercoagulability
- Each year of life “independently increases the likelihood of imbalanced clot formation”
Now lets jump into each of these diseases….
[bg_faq_end][bg_faq_start]1) List 8 DDx for DVT
First off, DVT…
- This is a spectrum: isolated calf vein thrombosis ← to → limb threatening illiofemoral clot
- Here’s the anatomy you HAVE to know! (see picture)
- From the bottom up:
- Deep venous system (is what we care about):
- Distal DVT = Calf veins: ant. + post. Tibial; peroneal vein.
- Proximal DVT = Thigh veins: popliteal, common femoral vein (formed from the “superficial” femoral vein and the deep femoral vein)
- NOTE that the superficial femoral vein – IS also known as the femoral vein – and IS a DVT!!!
- Superficial venous system (not a true “DVT”): greater and short saphenous veins AND perforating veins

- Deep venous system (is what we care about):
DDx: (Box 88-1)
- Fracture (stress / occult / pathologic)
- Popliteal cyst / rupture of
- Cellulitis
- Superficial thrombophlebitis
- Vasculitis
- Proximal venous compression (tumour, gravid uterus)
- CHF related bilateral leg swelling
- Hypoalbuminemia
- Lymphedema
- Muscle strain / calf strain
- Hematoma
- Chronic venous insufficiency
2) Describe management of superficial thrombophlebitis + isolated calf thrombosis
SLT:
- These patients have a clot in the greater saphenous vein that may extend above the knee.
- This can propagate proximally
- Treatment:
- NSAIDs for symptoms
- Heat
- Graded compression stockings
- **mandatory repeat ultrasound in 2-5 days**
- If it has migrated proximally most people at least treat these patients with LMWH or fondaparinux for 10 days, followed by repeat ultrasound
ICT:
- Controversial!
- 25% risk of proximal propagation proximally
- High risk symptomatic patients – can consider repeat duplex U/S in 2-5 days OR anticoagulation based on bleeding / clotting risk
- For healthy ambulatory patients – Rosen’s recommends:
- 325 mg ASA daily and repeat U/S at 2-5 days to look for clot propagation
3) How is the d-dimer test used in the diagnosis of DVT?
So, you’re wondering if this is a DVT….good for you!
The symptoms of DVT can be very subtle and nonspecific (cramping, sensation of fullness in the calf)
- Unilateral swelling, edema, erythema, warmth, tenderness to palpation of the venous system, dilation of the superficial collateral veins, palpable venous cord
- Homan’s sign is insensitive and nonspecific = useless! Do not rely on it!
****the lack of objective swelling is an unreliable gestalt tool to exclude the diagnosis of DVT!****
- When the DVT is at the “charley horse” stage – non specific mild symptoms – it is best for us to catch it because we can reduce the morbidity and mortality of VTE
Use of D-dimer:
- (See question 5!)
- People with a LOW pre-test probability can be risk stratified as “unlikely DVT” with a NORMAL quantitative D-Dimer.
4) List 8 causes of an elevated D-dimer
D-dimer (protein breakdown product of cross-linked fibrin breakdown = i.e. Clot has formed somewhere in the body in the last 72 hrs)
- D-dimer concentration is proportional to the size of the clot (ie. may be falsely low with chronic clots because they are mature)
- There are over 75 different D-dimer assays!
- Most common assay uses cut off of 500 NG/ML
- Sensitivity = 88-97% (for calf and proximal DVT)
- A “negative” May not exclude the disease in someone who is at high risk for the disease! (This is especially true for qualitative D-dimer tools)
- Sensitivity = 88-97% (for calf and proximal DVT)
- Endothelial damage
- Aging
- Recent surgery
- Infection
- New indwelling catheters
- Inflammation
- StrOke
- MI
- Venous stasis
- Prolonged bed rest / limb casting
- Hypercoagulable state:
- Active malignancy
- Pregnancy
5) What are the Wells criteria for DVT? Describe how to use this score.
- Dx of DVT starts with us using our clinical skills to calculate the pre-test probability
- Usually we use “the clinical gestalt of an experienced provider” OR a clinical decision tool
- According to current literature, neither expert consensus of clinical gestalt NOR clinical prediction rules are superior to one another.
- You could lump patients into two groups of people:
- Low – mod – high risk as groups (3)
- Unlikely – likely (2)
- Wells tool for DVT: see Table 88-1 or table below
- Scores:
- Low probability = score 0 – 2 (depending on the source)
- Moderate probability = 1 – 2 points
- High probability = 3 – 8 points.
- 8 points is the max
- According to current literature, neither expert consensus of clinical gestalt NOR clinical prediction rules are superior to one another.
| Feature | Score |
| pitting edema to the symptomatic leg only | 1 |
| tender to deep venous system | 1 |
| calf swelling > 3 cm asymm. | 1 |
| superficial non-varicose veins | 1 |
| entire leg swollen | 1 |
| recent plaster immobilization or paresis of the lower limb | 1 |
| bedridden > 3 days or major surgery in last 12 weeks | 1 |
| previous DVT (modified Wells feature) | 1 |
| active cancer (last 6 months or palliative) | 1 |
| alternate dx as likely as DVT | -2 |
Hx: prev. DVT, active cancer, bedridden or recent surgery in 12 weeks,
Edema
Entire leg Swollen
Superficial veins
Lippism:
“Wells 10 minus 2”
Wise gestalt (including past hx of DVT!)
Edema (swelling/veins)
Leg casted
Leukemia / lesions / lump (active cancer)
Surgery in 12
10 – for ten criteria
-2 – for one of them is minus two points.
- Several criticisms of the original well’s score:
- Prospective studies showing a 12% risk of DVT in the low risk group (not the advertised 3% risk). See PMID: 16027451
- A Meta analysis showing poor performance in the old, multiple comorbidities, and prior hx of DVT groups. PMID: 16027455
The Modified Wells Score:
- Includes the question of “previous DVT” = score of 1 (included in table above)
- Also breaks people into:
- DVT likely =. Score of 2 or greater
- DVT unlikely =. Score of 1 or less
After my exam writing is done, I’m probably not going to use Wells score…..
My approach:
DVT and no other clear DDx? → risk stratify as unlikely / likely DVT →
- if unlikely and a negative D-dimer STOP testing
- IF unlikely and a positive d-dimer get an ultrasound
- If likely DVT = jump right to ultrasound (ideally a single whole-leg ultrasound)
6) Describe management of suspected DVT
Radiographic eval:
- U/S = 95% sens & spec. For proximal DVT
- Using the standard 3 point compression tests
- The standard scanning protocol misses the calf veins and superficial veins (which can progress to a DVT)
- For low risk groups with a negative 3-point U/S after a +ve d-dimer you can stop testing
- For moderate-high risk groups, a single negative 3 point venous U/S is NOT sufficient to exclude a DVT, they should have a follow-up U/S in 2-7 days to exclude a DVT
- If you perform a single FULL leg doppler U/S (whole leg including superficial veins) – you can rule out a DVT in any of the risk groups (high/med/low)
If you’re trying to diagnose an iliac or pelvic vein DVT – you need to use CT-venography
[bg_faq_end][bg_faq_start]7) How is a proximal lower limb DVT managed?
- Start an appropriate LMWH (Enoxaparin 1 mg/kg SC q12hrs) OR
- Alternatives: (Check out Uptodate for a great discussion)
- Fondaparinux
- Apixaban
- Rivaroxaban
- OR heparin infusion after a loading bolus
- Ideally transition to oral anticoagulation at least 3 months (some up to 12 months)
- Encourage ambulation as much as possible
- Bedrest promotes DVT extension, risk of embolization, and post-DVT syndrome
- Alternatives: (Check out Uptodate for a great discussion)
8) What are the common causes of upper limb DVT?
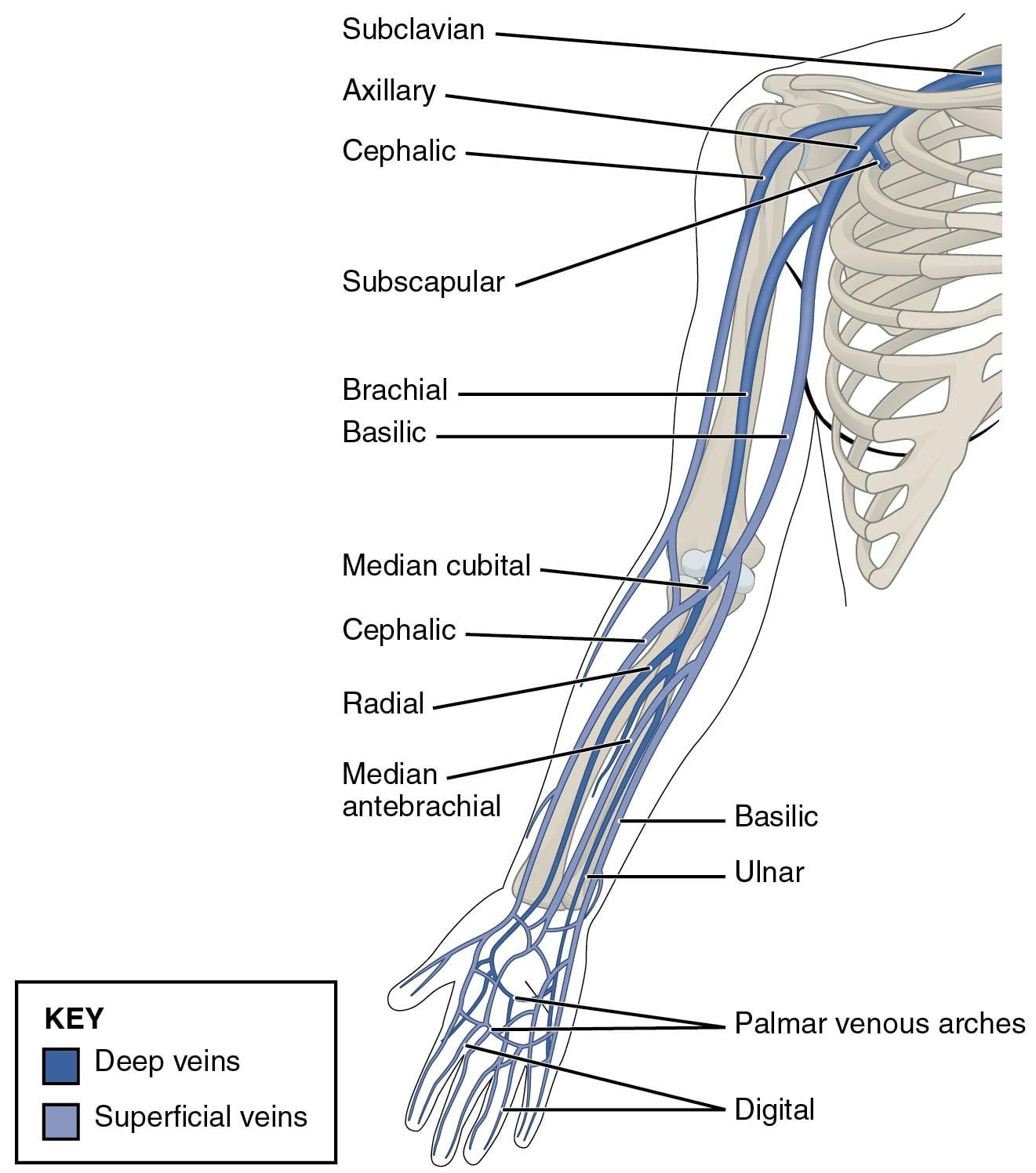
- Upper limb DVT = thrombosis in the axillary vein
- “The deep veins of the upper extremity include the paired ulnar, radial and interosseous veins in the forearm, paired brachial veins of the upper arm, and axillary vein. The axillary vein originates at the lower border of the teres major muscle in continuity with the brachial veins. The basilic and cephalic veins, which are superficial veins, contribute to the axillary vein, though many anatomic variations occur. After passing the outer margin of the first rib, the axillary vein continues as the subclavian vein.” – text from Uptodate – 2017
- Causes swelling on the same side of an indwelling catheter / IVDU / trauma
- **use of D-dimer in ueDVT population is not adequately studied**
- Breakdown of causes:
- 50% post indewlling catheter
- Post-indwelling cardiac device placement
- Healthy, young throwing/working out athletes (see wisecrack #5)
- Trauma
- Hypercoagulable states with anatomic abnormalities
- Inherited or acquired subclavian vein stenosis
9) How are upper limb DVTs managed?
At similar risk of PE, so is treated like a lower extremity DVT
- May or may not have to remove the catheter (depending on why it’s there)
- Because it can cause a PE – anyone with a u.e. DVT proximal to the elbow require definitive treatment
- Optimal dosing and duration is debated
- Usually at least 3 months of anticoagulation (do your risk analysis for everyone though!)
- Infusion phlebitis ) isolated brachial vein thrombosis – post recent IV infusion may be treated like a superficial thrombophlebitis of the lower leg, but good evidence is lacking.
- Optimal dosing and duration is debated
Remember, that we not only treat DVT’s to prevent PE’s, but ALSO because DVT’s damage the valves of veins – which can lead to venous insufficiency (see prev. chapter). This can become a chronic disabling disease!
- Pain, varicosities, ulcers, skin changes, swelling – all with high morbidity!
Now, we’re moving on to PE’s
[bg_faq_end][bg_faq_start]10) List classic risk factors for PE x 10
Every PE has its birth as a DVT somewhere in the body, which migrates to the lungs.
See Table 88-2 for a detailed list.
These are the ones that are highly associated with PE in the ED population:
- Hypercoagulable states:
- Inherited thrombophilia
- Active cancer
- Estrogen
- Prior PE / DVT
- Endothelial damage
- Surgery or Trauma within the last 4 weeks requiring hospitalization/GA
- Venous stasis:
- Surgery or Trauma within the last 4 weeks requiring hospitalization/GA
- Clinical signs/symptoms:
- Dyspnea
- Hemoptysis
- Pulse > 100
- O2 Sat < 95%
- Unilateral leg / arm swelling
Notice that smoking is NOT on that list! Smoking does not seem to increase the risk for PE compared with another patient who is a non-smoker with the same clinical presentation.
Remember, just like in cardiac disease these are epidemiologic/population risk factors and the abscence of them in a patient who has symptoms of a PE cannot be used to exclude the diagnosis!
Many symptoms are nonspecific in PE, and the suddenness of the onset of symptoms neither increases nor decreases the risk of PE.
Temp > 38.6 is more suggestive of pneumonia than PE.
***as many as 50% of people diagnosed with a PE have no identifiable risk factors for thrombosis!***
[bg_faq_end][bg_faq_start]11) What are the types of PE?
Different categories; see Table 88-4:
| Category | Criteria | Management |
| Low risk PE | ● Labs and vitals normal | ● Start PE treatment and probable d/c home |
| Non-massive PE (medium) | ● BP > 90 ● Elevated trop/d-dimer ● RV hypokinesia ● Sp02 < 94% | ● Start heparin, admit to telemetry bed |
| Submassive PE | ● Moderate distress ● New RBBB ● Sp02 < 90% | ● Start heparin ● Consider thrombolytics ● Admit to step down ICU |
| Massive PE | ● SBP < 90 mmHg with distress ● Cardiac arrest | ● Start heparin ● Give fibrinolytics* (ask re: contraindications!) ● ICU |
12) List 4 ECG + 2 CXR findings consistent with PE
These tests are more useful for finding alternative diagnoses to a PE, than confirming the diagnosis of PE
Findings of PE:
| ECG (look for signs of pulmonary HTN) | CXR |
| 1. Tachycardia 2. Symmetrical T-wave inversion (V1-V4) 3. McGinn-White pattern: S1Q3T3 4. Incomplete or complete RBBB
| 1. Unilateral basilar atelectasis 2. Hampton’s hump 3. Westermark’s sign (unilateral lung oligemia) |
13) What are the Wells criteria for PE? Describe how to use this score.
Now, let’s dive into risk scoring. Just like DVT we need to use our rational decision-making to guide our diagnostic process. So, start with the Pre-test probability. The Well’s score is an explicit tool, but an implicit/gestalt guess can be used. (Both seem to be similar in estimating pre-test probability)
If the risk is deemed to be > 2.5% then testing to rule out PE is indicated.
Well’s PE score:
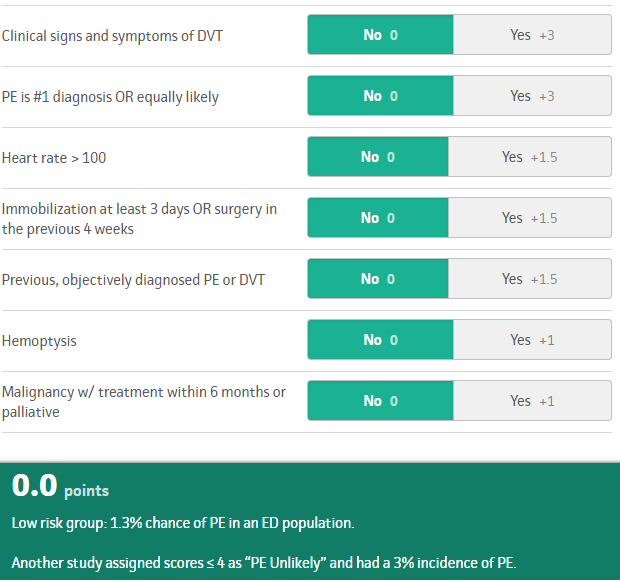
Check out: https://www.mdcalc.com/wells-criteria-pulmonary-embolism
For a great discussion on using the two tier or three tier approach.
For people with a risk > 2.5%, Rosen’s suggests we divide pts. Into two groups (this is the recommended two tier approach):
- Non-high (<40%) risk
- Order D-dimer
- i) If -ve = NO PE
- ii) If +ve = Get a CT-PE scan
- Order D-dimer
- High (>40%) risk
- Get a CT scan
- i) If -ve: consider further testing with doppler U/S for DVTs.
- ii) Review the scan with your radiologist!
- Get a CT scan
14) What is the PERC rule? How is it used?
This slick tool, can help us identify the VERY low risk population (risk <2%).
Only useful if the clinician deems the patient to be low risk!
Then if all the 8 features are satisfied, you can no longer work up for PE!
If patients have some of these risk factors, but NO chest pain / SOB / Dyspnea / SOBOE / syncope / and normal vitals – they probably don’t need a workup for PE!

15) Which imaging tests can be used to diagnose PE? List advantages and disadvantages of each.
CT-PE protocol
- +’ves: finds alternate diagnoses, rapid and fast, no iodine contrast used. Highly sensitive and specific.
- –‘ves: ionizing radiation
V/Q scanning
- +’ves: less radiation
- –‘ves: not as sensitive, does not find as many alternative diagnoses, must be stratified based on high-intermediate-low-normal probability.
- For example, someone with an intermediate probability scan still requires a CT-PE scan.
16) List indications for thrombolysis in PE, what is the risk of ICH?
- tPa: use is controversial
- Usually reserved for massive PE (diagnosed on CT-scan):
- Systolic BP < 90 mmHg for > 15 mins
- Or a reduction of ~> 60 mmHg from baseline
- Case by case use:
- in cardiac arrest
- Extensive clot burden
- RV dysfunction
- Hypoxemia
- Clot in transit
- Alteplase: 15 mg bolus, then 2 hr infusion of 85 mg. (then start heparin)
- Systolic BP < 90 mmHg for > 15 mins
- Usually reserved for massive PE (diagnosed on CT-scan):
Risk of ICH: 1-2%
[bg_faq_end][bg_faq_start]17) What are the absolute and relative contraindications?
Absolute or major contraindications to systemic thrombolytic therapy in acute PE include an intracranial neoplasm, recent (ie, <2 months) intracranial or spinal surgery or trauma, history of a hemorrhagic stroke, active bleeding or bleeding diathesis, or nonhemorrhagic stroke within the previous three months.
Relative contraindications include severe uncontrolled hypertension (ie, systolic blood pressure >200 mmHg or diastolic blood pressure >110 mmHg), nonhemorrhagic stroke older than three months, surgery within the previous 10 days, pregnancy.
From:
Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. https://www.ncbi.nlm.nih.gov/pubmed?term=22315268
Those patients with severe hypotension and a contraindication to fibrinolysis should be referred to see a vascular surgeon for embolectomy.
[bg_faq_end][bg_faq_start]18) List markers of poor prognosis in patients with PE.
Rosen’s states that 8% of patients with a PE in the ED will die within 30 days.
- Pulseless electrical activity (fully occluded pulmonary artery)
- Arterial hypotension
- Worsening respiratory distress
- Clot in transit
- Syncope or seizure in the ED
- Hypoxemia
- Evolving RBBB
- Multiple comorbidities
- RV dusyunfction (on Echo, troponin, or BNP)
Wisecracks
[bg_faq_start]1) What is phlegmasia cerulea dolens? How is it managed?
- Massive iliofemoral DVT:
- Need aggressive management:
- usually thrombolysis and/or thrombectomy.
- Intravenous (IV) UFH is usually the anticoagulant of choice
- Seek professional decision on whether to pursue more aggressive therapy (thrombolysis vs. thrombectomy)
- May progress to phlegmasia alba dolens or venous gangrene
- Need aggressive management:
2) Which patients should have an IVC filter?
- Used in patients with acute proximal DVT and PE who:
- have an absolute contraindication to anticoagulant therapy (eg, recent surgery, hemorrhagic stroke, active bleeding)
- Also often considered in patients with recurrent embolism despite adequate anticoagulation
3) What about PE/DVT in pregnancy?
- DVT / PE
- Managed with adjusted doses of LMWH for at least 3-6 months (at least 4-6 weeks post-partum)
- Not recommended:
- Heparin or Warfarin
- Do NOT use:
- Fondaparinux
- DOAC’s
- Not recommended:
- Managed with adjusted doses of LMWH for at least 3-6 months (at least 4-6 weeks post-partum)
4) What is the cause of hypoxia in patients with PE? What causes chest pain? What causes hypotension?
Hypoxia: due to V/Q mismatch. Areas of the lung that are ventilated (dead space) not being perfused.
Chest pain: thought due to a focal area of lung tissue necrosis (caused by intensive inflammatory processes)
Hypotension: impaired LV filling
[bg_faq_end][bg_faq_start]5) What is Paget-Schroetter Syndrome?
“Effort thrombosis, or Paget-Schroetter Syndrome, refers to axillary-subclavian vein thrombosis associated with strenuous and repetitive activity of the upper extremities. Anatomical abnormalities at the thoracic outlet and repetitive trauma to the endothelium of the subclavian vein are key factors in its initiation and progression. The role of hereditary and acquired thrombophilias is unclear. The pathogenesis of effort thrombosis is thus distinct from other venous thromboembolic disorders. Doppler ultrasonography is the preferred initial test, while contrast venography remains the gold standard for diagnosis. Computed tomographic venography and magnetic resonance venography are comparable to conventional venography and are being increasingly used. Conservative management with anticoagulation alone is inadequate and leads to significant residual disability. An aggressive multimodal treatment strategy consisting of catheter-directed thrombolysis, with or without early thoracic outlet decompression, is essential for optimizing outcomes. Despite excellent insights into its pathogenesis and advances in treatment, a significant number of patients with effort thrombosis continue to be treated suboptimally. Hence, there is an urgent need for increasing physician awareness about risk factors, etiology and the management of this unique and relatively infrequent disorder.”
From: https://www.ncbi.nlm.nih.gov/pubmed?term=21079709
Look for Urschel’s sign!
[bg_faq_end]This post was uploaded and copyedited by Colin Sedgwick (@colin_sedgwick)



