This episode of CRACKCast covers Rosen’s chapter 83, Infective Endocarditis and Valvular Disease. In this exciting episode we dive deep into how to diagnose and manage IE, and also explores what every emergency physician needs to know about the spectrum of diseases involving the heart valves.
Shownotes – PDF Here
[bg_faq_start]Infective Endocarditis
Principles of Disease
- increasingly becoming a disease of the aged: most cases in people > 60 yrs old
- Other high risk groups: nosocomial infections, degenerative valve disease, prosthetic heart valves
Pathophysiology
- initiated by a sterile thrombus on the heart/valve to which microorganisms attach
- usually a cardiac valve, but can also affect:
- chordae tendinae, septal defects, endocardium, etc.
- in IVDU contaminants such as talc injure the valve leaflets – which make them more prone for bacterial seeding
- precipitants causing transient bacteremia can occur (endoscopy, dental work, colonoscopy etc. ) in the susceptible host
Valvular heart disease
Anatomy:
- Three have three cusps (tricuspid, pulmonic, aortic)
- mitral – only two cusps.
- each cusp:
- double layer of endocardium attached at its based to the fibrous skeleton of the heart.
- margins of the cusps attached via chordae tendineae to the papillary muscles
- ventricular contraction opens and closes the valves.
1) List 6 RFs for bacterial endocarditis
- predisposing factors for bacterial IE (Box 83-4):
- calcific/degenerative aortic/mitral valves
- Rheumatic heart disease
- congenital cardiac lesions either repaired or unrepaired
- (VSD, pulm stenosis, TEt. of fallot, palliative conduits, )
- cardiac valve disease in a TRANSPLANTED heart
- **mitral valve prolapse***
- IVDU (right sided endocarditis)
- prosthetic valve
- history of endocarditis
- Break this list down into:
- Cardiac
- Non-cardiac: IVDU, indwelling IV catheters, immunosuppression, recent dental/surg. Procedure
2) List 5 common bacteria responsible for infective endocarditis
- Most common microorganisms (Table 83-1):
- Staphylococcus aureus (30%)
- Viridans – 18%
- enterococci – 10%
- Coag-negative staph. – 10%
- Bovis
- Other strep.
- non-HACEK gram negative bacteria
- Fungi (candida, aspergillus)
- HACEK
- haemophilus, actinobacillus, cardiobacterium, eikenella, kingella
- Polymicrobial
- Culture negative – 8%
3) Give three examples of immunologic sequelae of infective endocarditis
Clinical Features:
- intermittent fever
- Osler nodes / roth spots / rheumatoid factor
- Malaise, chills, anorexia
- non specific : weakness, myalgias, back pain, dyspnea, chest pain, cough, h/a
- murmur usually absent in EARLY disease
- present in < 30%
4) Give three examples of vascular sequelae of infective endocarditis
- Osler nodes
- Splinter hemorrhages
- Janeway lesions
- Roth spots
- Splenomegaly
- watch for stroke like symptoms and fever
- Can have emboli anywhere!
- CRAO
- Pneumonia
- MI
- Intestinal infarcts
- Can have emboli anywhere!
- “classic” symptoms are rare:
- unexplained fever,
- osler nodes, janeway lesions, petechiae, splinter hemorrhages, glomerulonephritis, splenomegaly, retinal hemorrhages, roth spots
5) What are the diagnostic criteria for endocarditis, and how are they used?
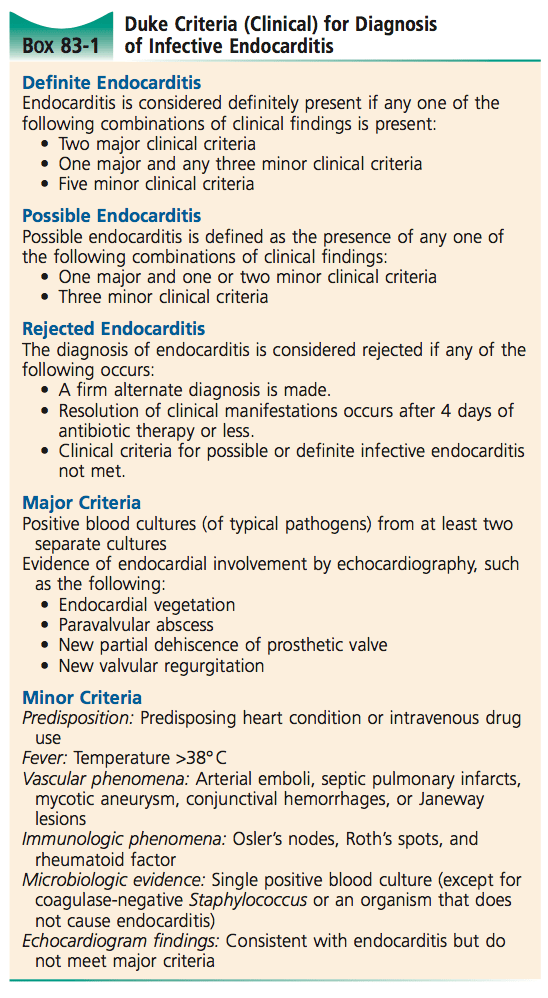
- The DUKE Criteria!
- Definite
- Unlikely …but it’s still possible
- KNOT endocarditis …..rejected!! = DUKE
- Three categories:
- And Major and minor criteria
6) List 5 lab or investigative findings in bacterial endocarditis
Diagnostic Strategies:
- usually nonspecific
- leukocytosis, CRP elevated, anemia, microscopic hematuria,
- abnormal CXR or ECG
- **need three (3) blood cultures from separate sites**
- TTE non-diagnostic in 20% of people (60% sens)
- TEE much better
- Duke Criteria are the best:
- 95% sens, 99% spec.
Don’t forget about the culture negative IE patient – the patient with negative blood cultures and persistent fevers AND at least one or more clinical findings of IE. This category also includes people with ECHO findings of vegetations on echo.
[bg_faq_end][bg_faq_start]7) Describe the treatment of infective endocarditis

Ideally we treat based on culture results…
Native valve endocarditis is usually caused by a gram +ve organism; people with prosthetic valves require more elaborate antimicrobial regimens (i.e. involve ID and the cardiac surgeon!)
- empirical ED therapy:
- Vancomycin 15 mg/kg IV q12hrs
- with history of IVDU!
- Ceftriaxone 2 g IV
- can also be exchanged with ampicillin and Gentamicin 1mg/kg IV q 8hrs
- Surgical therapy for IE – Box 83-3
- IE + Acute heart failure
- Fungal endocarditis
- Periannular extension of infection
- Recurrent emboli
- mobile vegetations
- Persistent bacteremia
- Vancomycin 15 mg/kg IV q12hrs
8) List four complications of IE.
- Cardiac
- Heart failure
- Perivalvular abscess
- Embolic
- CVA
- Blindness – due to CRAO
- Pain syndromes from intestinal / cardiac infarctions
- Metastatic infections (showered lung)
- Neuro:
- Stroke
- Acute encephalopathy
- Meningo-ecphalitis
- Seizures
- Renal
- Infarction
- Glomerular nephritis
- MSK:
- Vertebral osteomyelitis
9) List the indications for infectious endocarditis prophylaxis. What are the empiric antibiotics used for pts with suspected infectious endocarditis?
- Because the evidence for antibiotic prophylaxis is weak, the UK no longer recommends it. See: http://heart.bmj.com/content/103/12/937
- However, Rosen’s doesn’t cover it in much detail. They state that:
- all procedures routinely performed in the ED unless obviously stimulating an abcess or infection do NOT require prophylactic ABX in patients with prosthetic heart valves.
According to uptodate:
- High risk patients (anyone with foreign material in their heart or congenital heart disease or history of IE) should receive amoxicillin for most resp/GI/GU biopsy-like procedures, dental work, or SSTI’s undergoing manipulation….
10) Describe the Jones Criteria for Acute Rheumatic Fever

Rheumatic Fever
- dramatic decline since the 1920s
- improved living conditions, use of abx,
- 2-4 cases per 100,000
- peds peak in 4-9 yr olds, 25-35 yr olds in impoverished areas
Principles of Disease
- delayed, NON-suppurative complication of Strep. pharyngitis
- unknown pathogenesis
- Exaggerated immuno. response to Group A beta-hemolytic strep. –> antibodies cross reacting with tissues in the heart/joints/skin/CNS
- ***anyone with a hx of ARF are predisposed to recurrent infections and heart damage
- ARF does not equal RHD!
- Rheumatic heart disease occurs 15-20 yrs post ARF as a type of acquired valvular disease
Clinical Features
- post initial pharyngitis:
- latency period 1-5 weeks
- then signs of ARF appear
- >30% of people DON’T remember having pharyngitis
- Fever,
- Arthritis, carditis, chorea, SubCut nodules, erythema marginatum (<10% of cases)
- **migratory polyarthritis**
- affecting large joints (knees, ankles, elbows, wrists)
- pain out of proportion
- sterile inflammatory fluid
- Cardiac manifestations
- peri/myo/endo-carditis
- Mitral valve regurg.
- new high pitched systolic murmur
- Syndenham Chorea (St Vitus’ dance)
- random rapid purposeless movements of the upper extremities and face
- erythema marginatum: non pruritic, painless, smoke ring of erythema on trunk/extremities
- Nodules: painless
- then signs of ARF appear
- latency period 1-5 weeks
Diagnosis
- Jones Criteria:
- Antecedent Strep infection PLUS:
- >2 Mj criteria
- 1 mj + 2 minor
- Antecedent Strep infection PLUS:
- Antistreptolysin antibody titres (ASO) (positive for 4-6 weeks)
- Increased CRP
- Prolonged PR interval
11) What is the treatment of rheumatic fever
Management
- All people should receive ABX regardless of clinical history of pharyngitis
- Treatment:
- Penicillin to eradicate group A beta-hemolytic streptococcus
- IM one time dose or PO x 10 days
- same treatment plan for adults and kids
- Need to get source control
- Arthritis
- anti-inflammatory agents to treat the bad arthritis
- ASA or naproxen for joint symptom relief
- Steroids for severe carditis
- Treatment of CHF using the standard treatment
- anti-inflammatory agents to treat the bad arthritis
- ***Treatment of ARF does NOT prevent progression to RHD!!**
- Prevention
- treat those with Group A strep. Pharyngitis (and a previous history of ARF) within 9 days of the onset of symptoms
- Or give Penicillin G every 28 days – for 5-40 years!
- Penicillin to eradicate group A beta-hemolytic streptococcus
12) Name three causes of acute and three causes of chronic mitral regurgitation.
Acute
Idiopathic rupture
Ischemia induced papillary muscle dysfunction
Post-MI papillary muscle rupture
Infective endocarditis
Chronic
Dilated cardiomyopathy
RHD
MVP
Connective tissue disorder
[bg_faq_end][bg_faq_start]13) How is acute and chronic MR managed?
Mitral Regurgitation
● Acute
- emergency cardiac TEE and Cath.
- Nitrates and diuretics
- intra-aortic balloon pump
● Chronic
- Management:
- diuretics and afterload reducers
- surgery
14) What is the pathophysiology of mitral valve prolapse? How does it present?
Mitral valve Prolapse:
- usually benign billowing of a leaflet during systole
- can be associated with
- mitral regurg, endocarditis, arrhythmias
- connective tissue dz.
- Symptoms
- Chest pain, palpitations, dyspnea, lightheadedness, fatigue
- “auscultated click in midsystole”
- Management:
- Beta-blockers
- exercise,
- relaxation techniques
- usually a benign disease
15) List four causes of mitral stenosis
Mitral Stenosis
- #1 cause is Rheum. Heart disease (>85%)
- symptoms develop after the latency period of 10-30 yrs post Group A strep. infection
- Another cause:
- congenital mitral stenosis / annular calcification – aging, post-infection, degeneration
- Pathophys:
- impeded LA –> LV flow leads to left atrial hypertension — > decreased CO –>pulmonary congestion –> pulm. hypertension –> RV failure
- #1 complication = A. Fib.
- need to rate control
- Clinical features
- dyspnea on exertion, dec. exercise tolerance
- orthopnea
- Classic (RARE) presentations: “hemoptysis, hoarseness”
- Loud S1 with opening SNAP, low pitched rumbling diastolic apical murmur
- CXR:
- LAE
- EKG: a fib, LAE, RVH
- Management:
- “SLOW AND FULL”
- diuresis for vasc. congestion
- Anti-coag. for A fib,
- Surgery
- Treat Anemia, hypothyroidism, etc.
16) List four causes of aortic valve insufficiency
Aortic insufficiency
- aka: aortic regurg.
- aortic valve doesn’t close tightly so flow moves from aorta to LV
- caused by:
- bicuspid valve, RHD, IE
- ectasia, aneurysm, dissection
- Elderly patient with hypertension causing scleroSis and dilation of the ascending aorTa.
- pathophysiology
- LV compliance decreases, and LV pressure increases –>pulm congestion
- mild pressure gradient between aorta and ventricle
- clinical features:
- sx:
- sound like aortic dissection/resp. distress/cardiogenic shock
- need echo to diagnose
- sx:
- management:
- needs urgent valve replacement
- vasodilators
- diuretics
17) List 3 physical exam findings associated with aortic stenosis
Aortic stenosis
- #1 cause: calcific degeneration
- in the elderly and CAD
- other preconditions:
- Bicuspid aortic valve
- RHD
- significant reduction: valve area <50%,
- Clinical features:
- Progression of symptoms: angina –> syncope –> CHF –>
- Parvus et tardis – slow, rate of palpable rise in carotid pulse
- Crescendo – decrescendo murmur, mid to late peaking
- S4 gallop
- Causing a reduced second heart sound.
18) What is critical aortic stenosis? Outline the ED management for a pt with critical aortic stenosis with CHF and hypotension.
- Critical stenosis valve area <0.8cm squared.
- or **Pressure gradient >50 mmHg***
- compensated LVH can maintain CO until the stenosis becomes too severe!
- then patients become
- **preload dependent with LITTLE reserve***
- need to delicately balance myocardial 02 supply and demand
- Management:
- judicious fluid resuscitation
- blood transfusion
- return to Sinus rhythm
- AVOID
- nitrates
- diuretics
- inotropic agents
- Although dobutamine may be considered in a closely monitored setting.
- need surgery
- Slowly use diuretics and an ACE inhibitor if needed.
- then patients become
19) List 5 complications of prosthetic valves
- structural failure
- rare
- present in shock
- thrombosis of the valve
- CHF
- systemic embolization (thromboembolic)
- avoided by higher INR goal of 2.5-3.5
- usually CNS strokes
- at high risk for hemorrhagic conversion
- hemolysis
- hemolytic anemia due to sheer forces
- fatigue, jaundice, dark urine, dyspnea,
- endocarditis
- highest during the initial months post-op
- early <60 days
- Vary based on valve type:
- mechanical
- bioprosthetic
1) Describe the following lesions
- Janeway lesions
Non-tender erythematous macules on the palms and soles. They are micro-abscesses. Much more common than Oslers and Roths spots (these were described in the pre-antibiotic era).
- Osler nodes
Tender subcutaneous violaceous nodules usually on the pads of fingers and toes. (papulopustules)
- Splinter hemorrhages
Non-blanching, linear, reddish brown lesions under the nail beds
- Roth Spots
Exudative, edematous hemorrhagic lesions of the retina with pale centres.
[bg_faq_end][bg_faq_start]2) What are the HACEK organisms, and what is their significance in patients with IE?
- HACEK
- haemophilus, actinobacillus, cardiobacterium, eikenella, kingella
- These are rare <5-10%. They are fastidious gram -ve bacilli
- They occur in people with native valves, who DO NOT use IV drugs
- Historically hard to culture (>6 days needed, and thought to be the etiology in culture-negative IE), but now with automated blood culturing machines they can be cultured in 5 days or so.
- Susceptible to ceftriaxone
3)What are buzz-bizz features of all four valve diseases?
- Mitral stenosis
- Rheumatic heart disease – keep them SLOW and FULL
- Mitral regurg:
- Sudden fulminant pulmonary edema (find out why!!)- reduce the afterload!
- Mitral valve prolapse:
- Usually a benign disease – chill the heart out (beta blockers)
- Aortic regurg/insufficiency
- Can acutely present in cardiovascular collapse and CHF – think about florid infective endocarditis or aortic dissection. These people need surgery! (Diuretics, and vasodilators in the mean time, maybe dobutamine!)
- Aortic stenosis:
- Very common disease. Be very careful in suddenly dropping afterload or increasing it….all our go to agents are risky (diuretics, nitroglycerin, vasopressors)
- Carefully sustain preload. Start low go slow – consider an ACE inhibitor and diurEtic to slowly manage hypertension and. Symptoms.
- Right sided valve disease:
- Tricuspid heart disease – usually age related degeneration, managed with diuretics
- Pulmonic valve disease – rare!
This post was uploaded and edited by Ross Prager (@ross_prager)



