This episode of CRACKCast covers Rosen’s Chapter 76, Acute Coronary Syndromes. Part A of this episode covers the essentials of Acute Coronary Syndromes, including DDx, pertinent ECG findings and the ever important STEMI equivalents.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
Ischemic heart disease and CAD are leading causes of death worldwide…and expected to increase with the obesity and sedentary epidemic.
“In the United States, approximately 900,000 persons every year experience an AMI, of whom 20% die before reaching the hospital, and 30% die within 30 days.The majority of fatalities from CAD occur outside the hospital, usually from an ACS- related dysrhythmia within 2 hours of onset of symptoms. For many patients who experience a nonfatal AMI, their lives are limited by an impaired functional status, anginal symptoms, and a diminished quality of life. The economic cost of ACS is estimated to be $100 to $120 billion annually.” – quoted from Rosen’s 7th Ed.
“Coronary heart disease includes the spectrum from:
- Asymptomatic CAD and stable angina, to
- UA, AMI, and sudden cardiac death
- ACS includes the “acute” subtypes of coronary heart disease, including UA, AMI, and sudden cardiac death.”
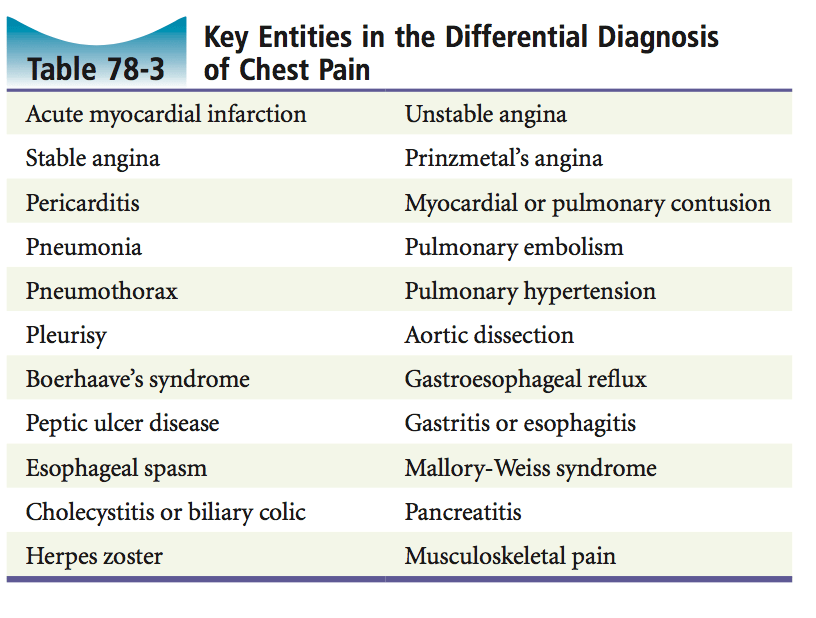
Don’t forget that DDx!
[bg_faq_end][bg_faq_start]1) Define Stable Angina, UA, AMI
Angina refers to “tightening” NOT pain! Remember to use terms like discomfort, pressure, ache, squeezing, heaviness, burning, not just “chest pain”….
- Stable Angina:
- “Stable angina pectoris is transient, episodic chest discomfort resulting from myocardial ischemia.
- This discomfort is typically predictable and reproducible, with the frequency of attacks constant over time.
- Physical or psychological stress (physical exertion, emotional stress, anemia, dysrhythmias, or environmental exposures) may provoke an attack of angina that
- ***resolves spontaneously over a constant, predictable period of time with rest or nitroglycerin (NTG).”***
- UA:
- “Unstable angina is broadly defined as angina occurring with minimal exertion or at rest, new-onset angina, or a worsening change in a previously stable anginal syndrome in terms of frequency or duration of attacks, resistance to previously effective medications, or provocation with decreasing levels of exertion or stress. Rest angina is defined as angina occurring at rest, lasting longer than 20 minutes, and occurring within 1 week of presentation. New-onset angina is angina of at least class II severity with onset within the previous 2 months. Increasing or progressive angina is diagnosed when a previously known angina becomes more frequent, longer in duration, or increased by one class within the previous 2 months of at least class III severity. Symptoms that last longer than 20 minutes despite cessation of activity are consistent with angina at rest and reflect UA.”
- Key points:
- Rest angina = lasts longer than 20 minutes (not the “I had chest pain while reading a book that lasted 5 minutes”)
- Can represent a possible harbinger of acute myocardial infarction
- Any ED patient with angina should be assumed to have UA until a thorough clinical evaluation proves otherwise.
- “UA can also be defined from a pathophysiologic perspective. Plaque rupture accompanied by thrombus formation and vasospasm illustrate the intracoronary events of UA. This is frequently characterized by an electrocardiographic abnormality, including T wave and ST segment changes.
- Variant angina—also known as Prinzmetal’s angina—is caused by coronary artery vasospasm at rest with minimal fixed coronary
artery lesions; it may be relieved by exercise or NTG. The ECG reveals ST segment elevation that is impossible to discern from AMI electrocardiographically and, at times, clinically.”
What are the Canadian cardiovascular guidelines for unstable angina?
“The Canadian Cardiovascular Society classification for angina is defined as follows:
- Class I, no angina with ordinary physical activity;
- Class II, slight limitation of normal activity as angina occurs with walking, climbing stairs, or emotional stress;
- Class III, severe limitation of ordinary physical activity as angina occurs on walking one or two blocks on a level surface or climbing one fight of stairs in normal conditions;
- Class IV, inability to perform any physical activity without discomfort as anginal symptoms occur at rest.”
- AMI = myocardial cell death leading to myocardial necrosis
- “This [universal definition for myocardial infarction] requires a typical rise and fall of a cardiac biochemical marker, currently troponin, with either (a) clinical symptoms, (b) ECG changes(T wave changes, ST elevation or depression, pathologic Q waves), or [c] coronary artery abnormalities based on interventional evaluation.”; or (d) wall motion abnormalities on echocardiography.
- Five types Of infarction:
- Type 1: a true ACS event leading to coronary thrombosis and vasospasm
- Type 2: demand ischemia – “shock” of the coronary arteries due to supply/demand imbalance
- Type 3: sudden cardiac death (arrest) before blood could be sampled.
- Type 4: Iatrogenic related to PCI
- Type 5: Related to CABG
- The AHA has differentiation in the management of UA/NSTEMI and STEMI….we’ll cover this below.
2) Describe the pathophysiology of AMI
Acute coronary artery thrombosis due to a sudden intraluminal activation of platelet-thrombotic factors leading to myocardial necrosis.
“Inadequate perfusion to meet myocardial oxygen demand [causing cell necrosis and death]. Myocardial oxygen consumption is determined by heart rate, afterload, contractility, and wall tension.”
- There can be stable fibrous plaques – that don’t usually cause symptoms until they are occluding
- There are those UNSTABLE fibro-fatty plaques that can spontaneously rupture.
- “Fibrolipid plaques consist of a lipid-rich core separated from the arterial lumen by a fibromuscular cap. These lesions are likely to rupture, resulting in a cascade of in ammatory events, thrombus formation, and platelet aggregation that can cause acute obstruction of the arterial lumen and myocardial necrosis.”
- “Angiographic studies demonstrate that the preceding coronary plaque lesion is often less than 50% stenotic, indicating that the most important factors in the infarction are the acute events of plaque rupture, platelet activation, and thrombus formation rather than the severity of the underlying coronary artery stenosis.”
3) What are the components of prehospital management of AMI
- Activation of the EMS system
- BLS care (for cardiac arrests)
- ACLS care:
- 12 lead ECG – to rule in/out STEMI
- Administration of chewable ASA 180-325 mg PO
- Administration of SL nitroglycerin
- Possibly administration of oxygen if Sp02 <94%
4) List population RFs for CAD. Do they matter in the evaluation of a specific patient?
Male gender, age, tobacco smoking, hypertension, diabetes mellitus, hyperlipidemia, family history, artificial or early menopause, and chronic cocaine abuse.
Non-traditional risk factors: Rheumatoid arthritis, Lupus, HIV
Do they matter in evaluation of a specific patient? NO!
“Nevertheless, Bayesian analysis indicates that risk factors are a populational phenomenon and do not increase or decrease the likelihood of any condition in any one patient. Thus the presence of an individual risk factor or a collection of risk factors is far less important in diagnosing acute cardiac ischemia in the ED than the history of presenting illness, prior diagnosis of ischemic cardiac disease in the patient, the presence of ST segment or T wave changes, or cardiac marker abnormalities.”
So, we should be relying on:
- HPI
- ST / T wave changes on ECG
- Prior diagnoses of cardiac ischemia in the patient
- Biomarker changes
5) List RFs for atypical presentation of ACS. What are the risks of atypical presentations?

- Women
- Elderly (Especially > 85 years)
- *Dyspnea, fatigue, confusion, syncope*
- Diabetics
- Non-Caucasian
- No prior hx of MI
- Dementia
These are at risk of:
- Delay in diagnosis: the emergency provider not thinking of the diagnosis in someone with an atypical symptom: e.g. Confusion, dyspnea, indigestion, ear pain, nausea, shoulder pain, fatigue, cold sweats, anxiety, diaphoresis etc.
- Not thinking that a person can have a concurrent ACS as well as trauma/infection
- Worsening outcomes/prognosis overall – increased complications and mortality rate
To sum it up: “Although certain features of the chest pain history serve to increase or decrease the likelihood of ACS, none of them is strong enough to endorse discharge of the patient based on the history alone.”
AND
“It is suggested that patients with chest pain that is fully pleuritic, positional, or reproducible by palpation (the three Ps) are at low risk (yet not no risk) for ACS.”
6) List 8 early complications of AMI and briefly describe the management of each one.
- Bradydysrhythmias / AV conduction block
- Atropine +/- pacing
- ACLS care
- Tachydysrhythmias (Sinus tach, a.flutter, VF, VT, etc)
- ACLS care!
- “80% of VF/VT occur in the first 12 hrs post MI”
- Cardiogenic shock
- Investigate for any other contributing causes (pericardial effusion, hypovolemia)
- “Therapeutic measures include vasopressor and inotropic support, intra-aortic balloon counterpulsation, and early revascularization; fibrinolytic therapy does not decrease mortality in cardiogenic shock.”
- LV freewall rupture
- Resuscitate
- Surgery! (If survived)
- Septal rupture
- Resuscitate
- Surgery
- Papillary muscle rupture (leading to mitral valve regurg.)
- Resuscitate
- Surgery
- Infarct Pericarditis
- Anti-inflammatories
- Embolic or hemorrhagic stroke
- Hyperglycemia
- IV insulin infusion
- Iatrogenic complications:
- From anticoagulation/antiplatelets/fibrinolysis – require resuscitation and discontinuation of the drug
- Difficult if not impossible to reverse most therapies
- Heparin – use protamine sulfate
- LMWH – can’t be reversed
- Fibrinolytics – can’t be reversed
- Anti-platelets – can’t be reversed
- Pseudoaneurysm from femoral artery cannulation
- Difficult if not impossible to reverse most therapies
- From anticoagulation/antiplatelets/fibrinolysis – require resuscitation and discontinuation of the drug
7) Describe the progression of ECG changes in STEMI
“In context, a single ECG is neither 100% sensitive nor 100% specific for AMI and reflects a single point in time. Over-reliance on a normal or nonspecifically abnormal ECG in a sensation-free patient with anginal chest pain should be avoided.”
Progression:
- Hyperacute, tall, broad-based, peaked T wave
- Often asymmetric

- Often asymmetric
- ST segment depression
- May be from NSTEMI or reciprocal change elsewhere in the myocardium

- May be from NSTEMI or reciprocal change elsewhere in the myocardium
- ST segment elevation
- May be flat / concave / convex / sloped
- Use the TP segment or terminal PR segment to measure ST elevation

- Use the TP segment or terminal PR segment to measure ST elevation
- Narrow, symmetrical, inverted T waves can also occur, but are nonspecific.
- Pseudonormalization of T waves
- Pathologic Q waves
- May appear within 1 hr of the ACS or typically after 8-12 hrs from the initial event.

- May appear within 1 hr of the ACS or typically after 8-12 hrs from the initial event.
- May be flat / concave / convex / sloped
“The patient’s history of the event—and the physician’s interpretation of the history—is the most important diagnostic study.”
DYNAMIC ECG changes should worry the clinician!
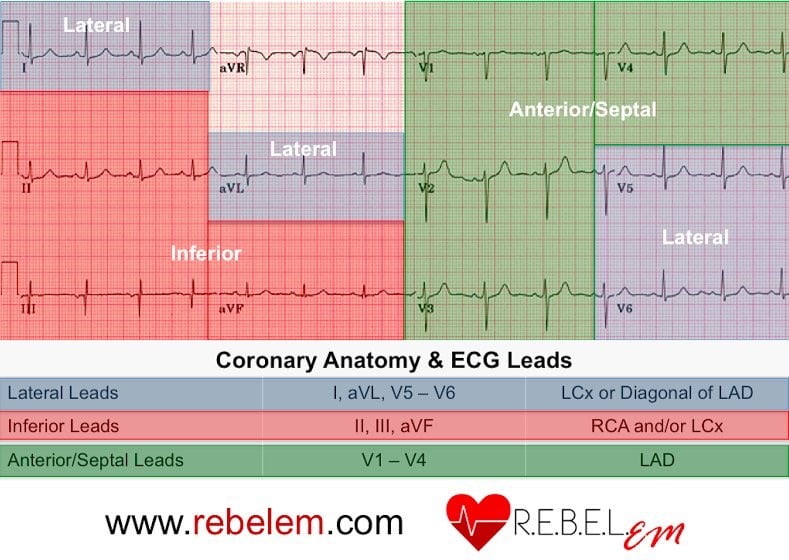
[bg_faq_end][bg_faq_start]8) List expected ECG changes (ST↑ and reciprocal ST↓) and culprit vessel for the following:

- Anterior wall MI
- Reciprocal: ST seg. Depression V8-V9
- LAD
- Lateral wall MI
- Reciprocal: V4R, II, III, aVF
- LCx
- Inferior wall MI
- Reciprocal: aVL depression
- RCA/LCx
- RV wall MI
- Reciprocal: V5-6
- RCA
- Posterior wall MI
- Reciprocal: V1-4
- LCx
REBELEM to the rescue!
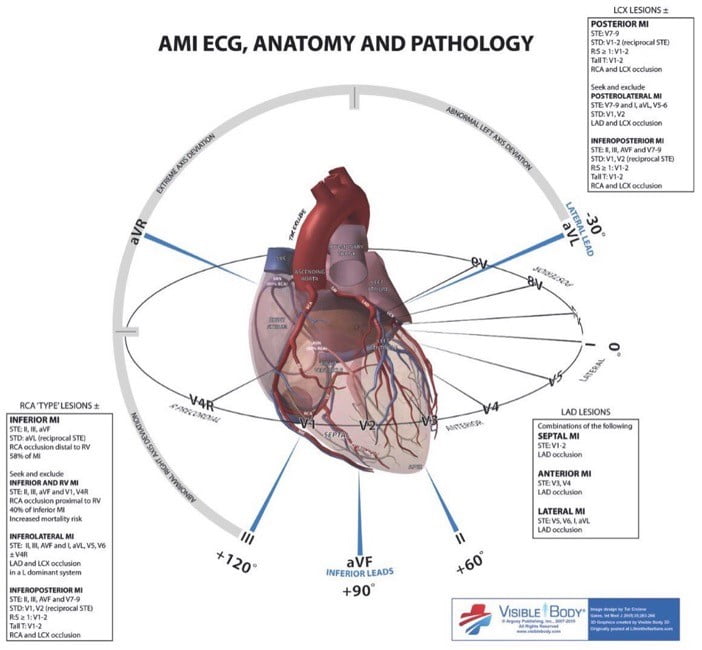
9) Describe the ECG characteristics of Left Main Occlusion
Widespread horizontal ST depression, most prominent in leads I, II and V4-6
ST elevation in aVR ≥ 1mm
ST elevation in aVR ≥ V1
What is Wellens’ sign and what is it’s significance?
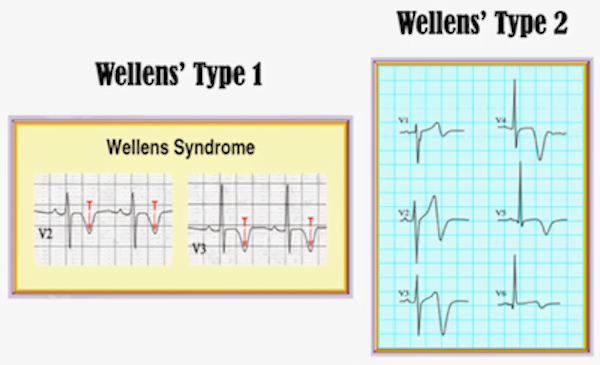
Image from: https://www.aliem.com/2013/06/wellens-syndrome-on-your-radar/
“A notable subgroup of ischemic T wave inversions is associated with Wellens syndrome, which classically manifests with either deep symmetrical T wave inversions (type I) or biphasic T wave changes (type II) in the anterior precordial leads. The presence of biphasic T waves is suggestive of ischemic heart disease. Other electrocardiographic features include isoelectric or minimally elevated (<1 mm) ST segments and no precordial Q waves. This finding may manifest in the anginal or pain-free state and may or may not be accompanied by cardiac marker elevations, which is indicative of a lesion of the left anterior descending artery.”
[bg_faq_end][bg_faq_start]10) List 10 DDx for ST-elevation

11) Describe the ECG features of:
Benign early repolarization
- ST segment elevation;
- upward concavity of the initial portion of the ST segment;
- notching of the terminal portion of the QRS complex at the J point (i.e., junction of the QRS complex with the ST segment);
- symmetrical, concordant T waves of large amplitude;
- diffuse ST segment elevation on the ECG;
- relative temporal stability over the short term, although these changes may regress with old age;
- maximal ST segment elevation in BER is typically seen in leads V2 to V5
Pericarditis
- Diffuse ST segment elevation, ST seg. depression in aVR
- PR segment depression (insensitive) in leads II, III, aVF, V6
- PR segment elevation (in lead aVR)
**remember that the pericardium is electrically silent, so when ST changes occur, it is important to think of myopericarditis**
LBBB
- QRS duration of > 120 ms
Dominant S wave in V1
Broad monophasic R wave in lateral leads (I, aVL, V5-V6)
Absence of Q waves in lateral leads (I, V5-V6; small Q waves are still allowed in aVL)
Prolonged R wave peak time > 60ms in left precordial leads (V5-6)
(from LITFL)
RBBB
- Broad QRS > 120 ms
RSR’ pattern in V1-3 (‘M-shaped’ QRS complex)
Wide, slurred S wave in the lateral leads (I, aVL, V5-6)
(From LITFL)
Ventricular-paced rhythm
- Similar morphology to LBBB
Except:- Predominantly negative QRS in V5,V6
- Pacer SpikesThe Sgarbossa criteria may be used in this clinical picture to assist in the diagnosis of AMI
LVH / Strain-pattern
- Limb Leads
R wave in lead I + S wave in lead III > 25 mm
R wave in aVL > 11 mm
R wave in aVF > 20 mm
S wave in aVR > 14 mm - Precordial Leads
R wave in V4, V5 or V6 > 26 mm
R wave in V5 or V6 plus S wave in V1 > 35 mm
Largest R wave plus largest S wave in precordial leads > 45 mm - Increased R wave peak time >50 ms in leads V5 or V6
LV aneurysm:
- Any ST elevation morphology in V1-V6
- “The calculation of the ratio of the amplitude of the T wave to the QRS complex may help distinguish acute anterior MI from LVA. If the ratio of the amplitude of the T wave to the QRS complex exceeds 0.36 in any single lead, the ECG probably reflects acute MI. If the ratio is less than 0.36 in all leads, however, the findings are probably a result of ventricular aneurysm.”
Wise Cracks
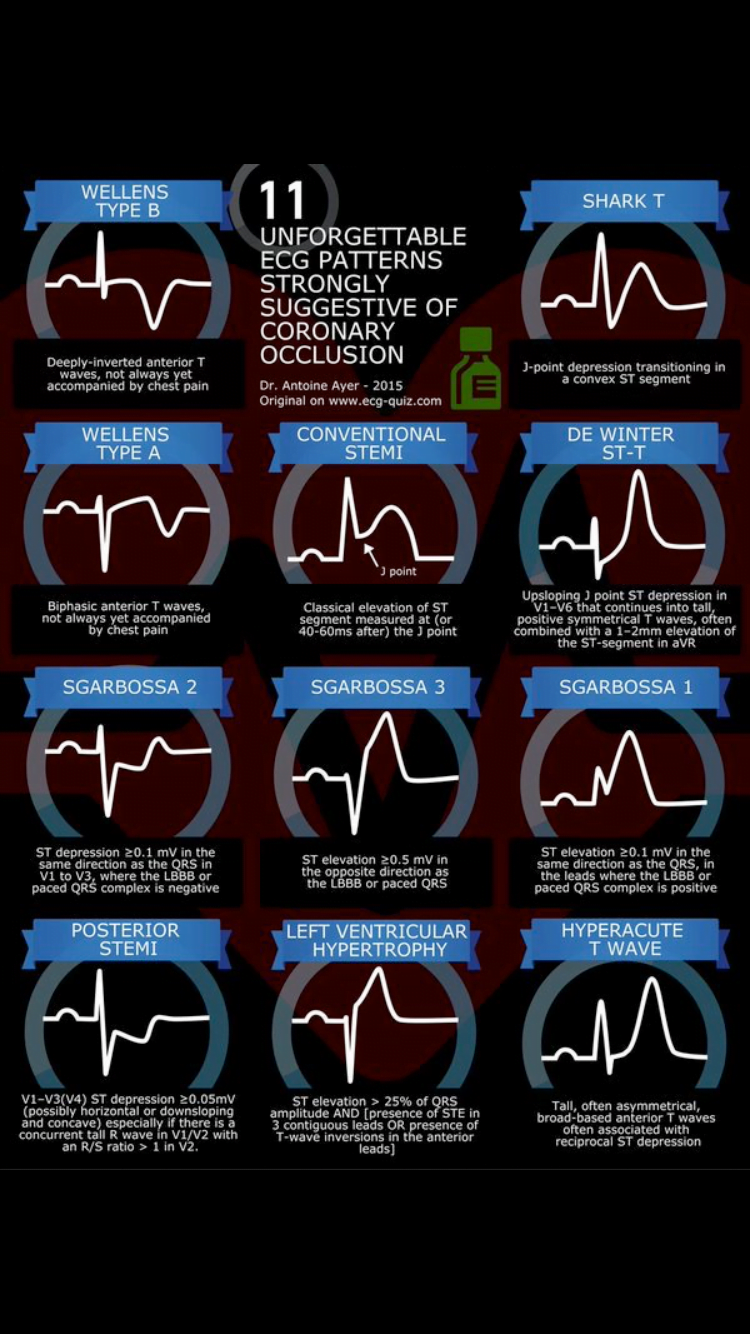
[bg_faq_start]1) What are the STEMI equivalents? Know these patterns!!!
This post was uploaded and copyedited by Colin Sedgwick (@colin_sedgwick)






