This episode of CRACKCast covers Rosen’s Chapter 76, Pneumonia. This episode tackles high yield information on diagnosis and management of pneumonia, one of the most common emergency department presenting illnesses.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
- This is a common disease – thankfully most cases can be managed as an outpatient, however, this is expected to change slightly over the next decades – with the aging population, antibiotic resistance increasing, and as the number of people burdened with chronic disease increases
- The ED goals are:
- Make the diagnosis
- Start empirical treatment (this is tough disease because we almost never culture the bug!)
- Provide respiratory support
- Risk stratification +/- admission
- In the grand scheme of things – it’s amazing we don’t get more infections in our lungs – with the surface area being over 140 m2; and us breathing over 10,000 L of air each day!!
- Pneumonia develops when:
- Host defences are overwhelmed
- A Virulent organism shows up
- A large amount of oropharyngeal organisms is aspirated
Typical vs Atypical infections
- Typical ones:
- Streptococcus pneumoniae (very virulent)
- Haemophilus influenzae
- Staphylococcus aureus
- CA MRSA can commonly be associated with influenzae
- IVDU’s
- Look for the cavitation, and necrosis on the CXR
- Atypicals
- Legionella
- Mycoplasma
- Chlamydophila
- Virals:
- Influenzae
- Parainfluenza
Usually named Community acquired (CAP) vs Healthcare associated pneumonia (HCAP), or Ventilator associated Pneumonia (VAP)
1) Hospitalization for 2 or more days in an acute care facility within 90 days of infection;
(2) Attendance at a hemodialysis clinic; and
(3) Intravenous antibiotic therapy, chemotherapy, or wound care within 30 days of infection.
HCAP is associated with a greater likelihood of resistant pathogens such as Pseudomonas and MRSA, and mortality is higher than that for CAP
[bg_faq_end][bg_faq_start]1) What are the typical associative pathogens?
Big shout out to LITFL, where this list was acquired:
- Alcoholism — Streptococcus pneumoniae, anaerobes, Gram negatives such as Klebsiella pneumonia, tuberculosis
- COPD/ smoker — Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis
- Nursing home resident — Streptococcus pneumoniae, Gram negatives, Haemophilus influenzae, S. aureus, Chlamydophila pneumoniae consider tuberculosis and anaerobes (but less common)
- Poor dental hygiene — anaerobes
- Bat / cave exposure — Histoplasma capsulatum
- Bird exposure — Chlamydophila psittaci, Cryptococcus neoformans, Histoplasma capsulatum
- Rabbit exposure — Francisella tularensis
- Exposure to farm animals or cats — Coxiella burnetti (Q fever)
- Post-influenza — S. pneumoniae, S. aureus
- Bronchiectasis, cystic fibrosis — Pseudomonas aeruginosa, S. pneumoniae, Burkholderia cepacia
- Sickle cell disease, asplenia — S. pneumoniae, H. influenzae
- Suspected bioterrorism — Anthrax / Tularemia
- Tropical Australia — melioidosis, Acinetobacter
- Potting mix — Legionella longbeachae
- Travel to Asia — SARS, tuberculosis, melioidosis
2) Describe the typical clinical presentation/risk factors/management for each of the following
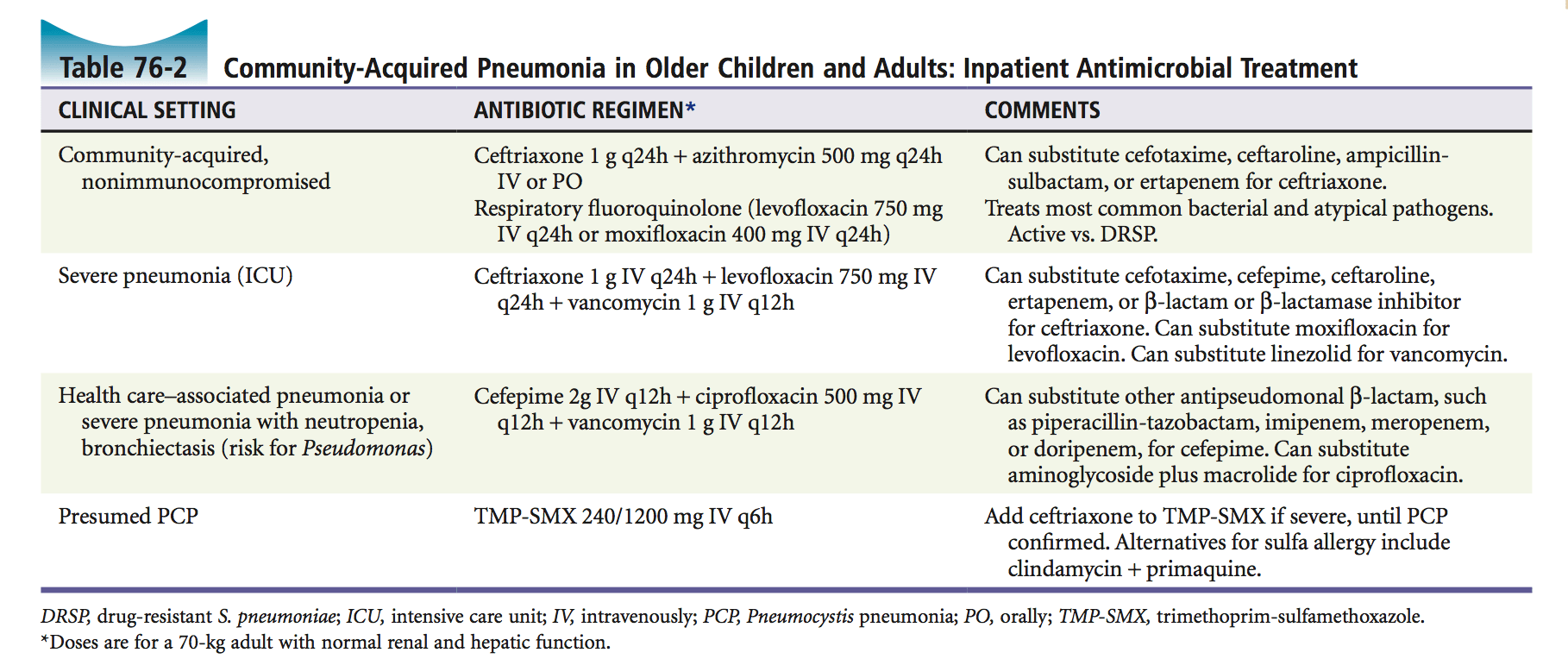
In general the guidelines for CAP are as follows, but confirm with your local resistance patterns and guidelines:

Pneumonia
- A gram +’ve cocci that is the most common cause of pneumonia requiring hospitalization – it colonizes 40% of health adults’ nares
- This is the bug targeted by the pneumococcal vaccine: By getting a vaccine with 13 or 23 of the capsular polysaccharides of pneumococcus it is thought to make any infections that occur less severe
- RF: unvaccinated / COPD / Smoker / ETOH / Asplenism / Sickle Cell / Nursing Home / Post Influenza
- Drug resistant S. pneumoniae (DRSP) is increasing. DRSP usually penicillin / β-lactams, macrolides, tetracyclines, and trimethoprim-sulfamethoxazole (TMP-SMX) are no good or variably effective.
- Extended- spectrum/ respiratory fluoroquinolones,(Levofloxacin or Moxifloxacin), are active against DRSP and other typical and atypical bacterial pathogens. 3rd gen cephalosporin plus macrolide also okay.
- Treatment: If admitted: 3rd gen. cephalosporin + macrolide OR respiratory fluoroquinolone
Influenzae
- 2nd most frequently isolated organism in CAP among adults
- Pleomorphic gram-negative rod.
- RF: COPD, alcoholism, malnutrition, malignancy, diabetes
- Treatment: Amoxicillin or a second- or third-generation cephalosporin
Staph aureus
- S.aureus common cause of CAP
- CAP MRSA more common to cause severe disease
- Often associated with influenza
- Often necrotizing, with cavitation and pneumatocele formation.
- RF: Intravenous drug users, immunosuppressed, known colonised
- Treatment: Vancomycin or Linezolid
Klebsiella
- Klebsiella pneumoniae is a gram-negative
- Rare cause of CAP in immunocompetent
- RF: alcoholism, diabetes, or other chronic illness.
- There is a high incidence of antibiotic resistance because the organism is often hospital acquired
- High risk for ESBL and CRO
- Treatment: No risk for MDR: Piperacillin-tazobactam / Cefepime / Imipenem / Meropenem / Levofloxacin
- MDR risk factors than add Amikacin / or Gentamicin / or Tobramycin
Mycoplasma pneumoniae & Chlamydia
- Mycoplasma pneumoniae is one of the most common causes of CAP
- pneumoniae, an intra cellular parasite that is transmitted between humans by respiratory secretions or aerosols
- Treatment: Macrolides such as erythromycin and azithromycin, doxycycline, or a fluoroquinolone such as levofloxacin or moxifloxacin.
Legionella
- Legionella is an intracellular organism that lives in aquatic environments.
- There is no person-to-person transmission.
- often implicated in point outbreaks related to cooling towers and similar aquatic sources, the organism also lives in ordinary tap water and is underdiagnosed as a cause of CAP. Legionella prevalence seems to vary greatly by region.
- Symptoms: important bug to think of in patients with both resp and GI symptoms (the diarrhea)
- 53% of patient have neuro abnormalities such as confusion and delirium
- Treatment: Azithromycin or levofloxicin, can consider doxy, spectra or imipenem for refractive
Anaerobes
- Generally from aspiration
- These infections are typically polymicrobial
- including Peptostreptococcus, Bacteroides, Fusobacterium, and Prevotella
- RF: central nervous system depression or swallowing dysfunction, severe periodontal disease, fetid sputum, and the presence of a pulmonary abscess or empyema.
- Treatment: Ampicillin-sulbactam or amoxicillin-clavulanate in mild disease. Can also use flagyl plus amox for mild as well.
- Severe disease consider imipenem, meropenem or piperacillin-tazobactam
- Add vanco if MRSA suspected
Pseudomonas
- HAP and CAP w: A compromised immune system (eg, HIV-infected patients, solid organ or hematopoietic cell transplant recipients, neutropenic hosts, and those on immunosuppressive or immunomodulatory agents such as TNF-alfa inhibitors)
- Recent prior antibiotic use
- Structural lung abnormalities such as cystic fibrosis or bronchiectasis
- Repeated exacerbations of chronic obstructive pulmonary disease requiring frequent glucocorticoid and/or antibiotic use
- Treatment: Piperacillin-tazobactam, ceftazidime, cefepime, imipenem, meropenem, and doripenem. Antipseudomonal quinolones include ciprofloxacin and levofloxacin
PJP & Other Fungal Pneumonia
- Bugs that live in the soil – so be suspicious in dirt bikers or people not responding to antibiotics (or those geographic areas in the USA rosen’s lists…Mississippi. Valley…)
- Histoplasma capsulatum – histoplasmosis
- Blastomyces dermatitidis – blastomycosis
- Coccidioides immitis – coccidiodomycosis
- Treatment: This is a super important differential to think of in the patient with “non-resolving” pneumonia
- Get help from ID and Respirology (need a bronchcoscopy)
- Managed with: Amphotericin B, Azoles (itraconazole, ketoconazole, fluconazole, etc)
Pneumocystis pneumonia (PCP)
- Occurs in immunocompro- mised hosts, principally people with immune deficiency syndrome (AIDS) or malignancy. Pneumocystis jiroveci (previously known as Pneumocystis carinii) is one of the most common infec- tions leading to a diagnosis of HIV infection and AIDS
- Patients with pulmonary complaints should be questioned about HIV risk factors, and clinicians should search for signs of HIV-related immunosuppression, such as weight loss, lymphadenopathy, and oral thrush.
- Presentation: PCP typically manifests subacutely with fatigue, exertional dyspnea, nonproductive cough, pleuritic chest pain, and fever.
- Treatment: Septra
Tuberculosis
- Mycobacterium tuberculosis is a slow-growing bacterium trans- mitted between people by droplet nuclei produced from coughing and sneezing.
- tuberculosis survives within macrophages and may remain dormant in the body for many years.
- Active tuberculosis (TB) develops within 2 years of infection in approximately 5% of patients, and another 5% develop reactivation disease at some later time.
- Reactivation is more likely to occur in people with:impaired cell-mediated immunity, such as patients with diabetes, renal failure, immuno- suppressive therapy, malnutrition, or AIDS.
- Approximately one third of the world’s population is infected with M. tuberculosis. Approximately 8 million new cases of active disease develop annu- ally, resulting in 3 million deaths worldwide. An estimated 10 to 15 million people in the United States (3-5% of the population) are infected with TB.
- Multidrug-resistant strains of M. tuberculosis are found in increasing numbers, especially among immigrants from Southeast Asia and AIDS patients.
- Treatment: Non drug resistant suggest isoniazid or rifampicin consider consult with ID and admission
Tularemia
- Not specifically covered in this chapter but important
- Tularemia is the zoonotic infection caused by Francisella tularensis
- an aerobic and fastidious gram-negative bacterium.
- Treatment: Gentamicin or Doxy / Ciprofloxacin if mild disease. Aminoglycosides are generally the agents of choice. Duration 7 to 10 days, but can extend to 14 days
Hantavirus
- Zoonotic infection from rodent family
- Two major forms of hantavirus disease are recognized: hemorrhagic fever with renal syndrome (HFRS) and hantavirus cardiopulmonary syndrome (HCPS, also called HPS)
- most severe forms are associated with Sin Nombre virus (SNV) and the southern (prototypical) form of Andes virus;
- In general, case-fatality ratios of HCPS range from 30 to 50 percent for severe forms
- Treatment: Supportive care / ECMO / Ribavirin
3) List the typical etiologies of viral pneumonia?
Infants: Respiratory syncytial virus and parainfluenza virus
Children and Adults: Add Influenza (mostly A) and Metapneumovirus
Don’t forget to order your Nasopharyngeal aspirate for your viral panel to determine what pathogen you’re dealing with
[bg_faq_end][bg_faq_start]4) Which patient groups should receive pneumovax?
Patients with:
- Diabetes
- Alcoholism
- Cardiovascular disease
- Sickle cell disease
- Splenectomy
- Malignancy
- Immunosuppression
- Older than 65 years
5) Which pneumonias can present with cavitating lesions (abscesses) on x-ray?
- Aureus (MRSA)
- Anaerobes
- aerobic gram-negative bacilli,
- Fungal disease ie PCP
- TB
- Noninfectious processes (e.g., malignancy and pulmonary vascular disease).
6) What is the differential for ?Pneumonia visible on CXR?
Note: Many non-infectious conditions can cause inflammatory lung processes
- Exposure to mineral dusts (e.g., silicosis)
- Chemical fumes (e.g., chlorine and ammonia)
- Toxic drugs (e.g., bleomycin)
- Radiation
- Thermal injury
- Oxygen toxicity
- Immunologic diseases (e.g., sarcoidosis, Goodpasture’s syndrome, and collagen vascular disease)
- Hypersensitivity to environmental agents (e.g., farmer’s lung disease)
- Tumors may appear initially as a postobstructive infection or adenopathy with peripheral infiltrates.
- Lymphangitic spread of lung malignancy (looks like interstitial PNA)
7) Describe the analysis of pleural fluid
Check out: https://lifeinthefastlane.com/ccc/pleural-effusion/
Pleural effusions can be blood, chyle, transudative or exudative
- Blood – post-op, trauma, malignancy, pulmonary infarct
- Chyle – trauma or rupture thoracic duct (eg strongyloides)
- Transudate – increased hydrostatic pressure (heart and liver failure, fluid overload), decreased oncotic pressure (nephrotic syndrome, loosing protein), negative pleural pressure (atelectasis)
- Exudate – parapneumonic effusion, empyema, subphrenic abscess, pancreatitis
Many bugs can cause pleural effusion, including many types of pyogenic bacterial pneumonias, Chlamydophila species, Legionella species, and TB.
Note: Anaerobic infections associated w/ effusion are prone to empyema.
Which effusions should be sampled?
- Pleural effusion >5cm on lateral upright posterior-anterior chest radiograph
- Significant resp distress
- Anyone with signs of tension / mediastinal shift
What are Light’s criteria?
https://lifeinthefastlane.com/investigations/pleural-fluid-analysis/
Lights criteria (High protein and LDH = exudate), determines presence of exudate with protein and LDH levels
- Pleural fluid protein to serum protein ratio >0.5
- Pleural fluid LDH to serum LDH ratio >0.6
- Pleural fluid level >2/3 of upper value for serum LDH
- Additional criteria – Confirm exudate if results equivocal
- Serum albumin – pleural fluid albumin <1.2g/dL
8) What is the CURB65 score?
Confusion
Uremia (blood urea nitrogen >20 mg/dL)
Respiratory rate greater than 30
Blood pressure less than 90 systolic or less than 60 diastolic,
65 years (age) or greater.
How to use it: The risk of 30-day mortality increases with a greater number of these factors present:
- 7% with zero factors
- 2% with two factors
- 57% with five factors.
- Patients with zero or one feature can receive o/p management
- 2 – Admit
- 3 – consider ICU
Summary
Key point: ***Radiologic and clinical findings are nonspecific for predicting a particular infectious cause!***
[bg_faq_end]This episode was edited and uploaded by Ross Prager (@ross_prager)


