This episode of CRACKCast covers Rosen’s Chapter 54, Back Pain. Back pain is one of the most common reasons for visits to the emergency department. Everyone will experience back pain at some point in their lives – having a solid approach to ruling out life threatening diagnoses is critical and will come in handy on your very next emergency shift.
Shownotes – PDF here
[bg_faq_start]Rosen’s in Perspective:
- Everyone in the world will experience back pain sometime in their life.
- Costs USA billions of dollars a year
- Pain < 6 weeks = acute back pain
- The cause of back pain remains unknown in up to 85% of patients after initial investigation
- The pathology is assumed to be soft-tissue in origin: muscles, ligaments
- There are no pathognomonic tests for low back pain, so terms used include:
- Acute lumbosacral pain
- Lumbago
- Mechanical back pain
- ***idiopathic low back pain*** is the preferred term
- No red flags on hx or physical exam
- Often no clear inciting cause
- Pain asymmetric in the lumbar paraspinal muscles
- Radiation to buttock and proximal thigh
- Exacerbated by movement
- Most cases resolve in 6 weeks, pain decreased by 58% at 1 month
- Mainstay of treatment is avoiding bed rest
- Recurrence rate: 60-80%!
- Chronic low back pain – huge morbidity for the patient and difficulty for the physician
- Risk factors:
- Poor pain coping behaviour
- Functional impairment
- Poor general health
- Psychiatric disease
- Risk factors:
Anatomy and Physiology
- 5 lumbar vertebrae and the sacrum

- Bone structure: vertebral body, two pedicles, two transverse processes, two overarching laminae, a spinous process
- Each vertebral body has superior and inferior articulating processes (facet joints)
- The neural canal is surrounded by these structures
- Has a diameter 15-23 mm
- The Intervertebral disks: have no sensory fibers
- Inner colloidal gelatinous substance – the nucleus pulposus
- Outer capsule: annulus fibrosus which is thinner posteriorly
- Ligaments:
- Anterior and posterior longitudinal ligaments
- The PLL protects the neural canal, but it thins from L1 – S1
- The ligamentum flavum – sits just anterior to the laminae. (this thickens with age and cause spinal stenosis)
- Anterior and posterior longitudinal ligaments
Pathophysiology:
- Think of back pain in broad categories:
- Life threats:
- 85% of cases are usually thought to originate from muscle-nerve tissue
- “Idiopathic low back pain”
| Nerve root origin ● Spinal nerve root ● Cauda equina irritation | Articular facet origin | Bone origin | Referred pain |
| Pain causes: In sciatica: ● Local nerve ischemia from compression of the disk ● Nerve inflammation from the exposure to the nucleus pulposus In spinal stenosis, congenital narrowing, degenerative changes in any of the structures | Degenerative changes to the synovial articular facets
Likely contributes in 15-45% of chronic back pain cases | Direct irritation of the vertebral bone and periosteum Osteomyelitis, Potts disease (tuberculosis infection), hematogenous seeding from skin, urine, IVDU (think Staph. Aureus coverage) Primary and metastatic bone tumours -breast, lung, prostate, thyroid, kidney, lymphoma. | ● Think intraperitoneal and retroperitoneal structures
|
| Do not miss: Cauda equina Spinal infections
| Ank. spondylitis, rheumatoid arthritis, psoriatic arthritis. Morning stiffness, pain relief with activity. Decreased ROM. SI tenderness | Degenerative: -osteoporosis -inflammatory | AAA – leaking/ruptured Pancreatitis Gallbladder Aortic dissection Pyelonephritis Pneumonia PE Renal colic Retroperitoneal hemorrhage Peptic ulcer Ectopic |
What about kids?
- Similar challenges exist in the pediatric population: non-specific back pain is diagnosed in 50% of cases
- Similar pathologies exist in children
- Watch for the athlete with back pain and spondylolisthesis
- Watch for leg length discrepancy
- UTIs
- Sickle cell crisis
- Imaging may identify:
- Spondylolysis / Spondylolisthesis
- Forward shifting of one vertebral body on another
- No evidence to support surgery for degenerative spondylolisthesis in adults
- In kids:
- Surgery for > 30-50% slippage
- < 30-50% = activity modification
- Kyphosis and osteochondritis
- Disc herniation can occur, but it is rare.
- Spondylolysis / Spondylolisthesis
1) Describe the myotomes and dermatomes L3-S1
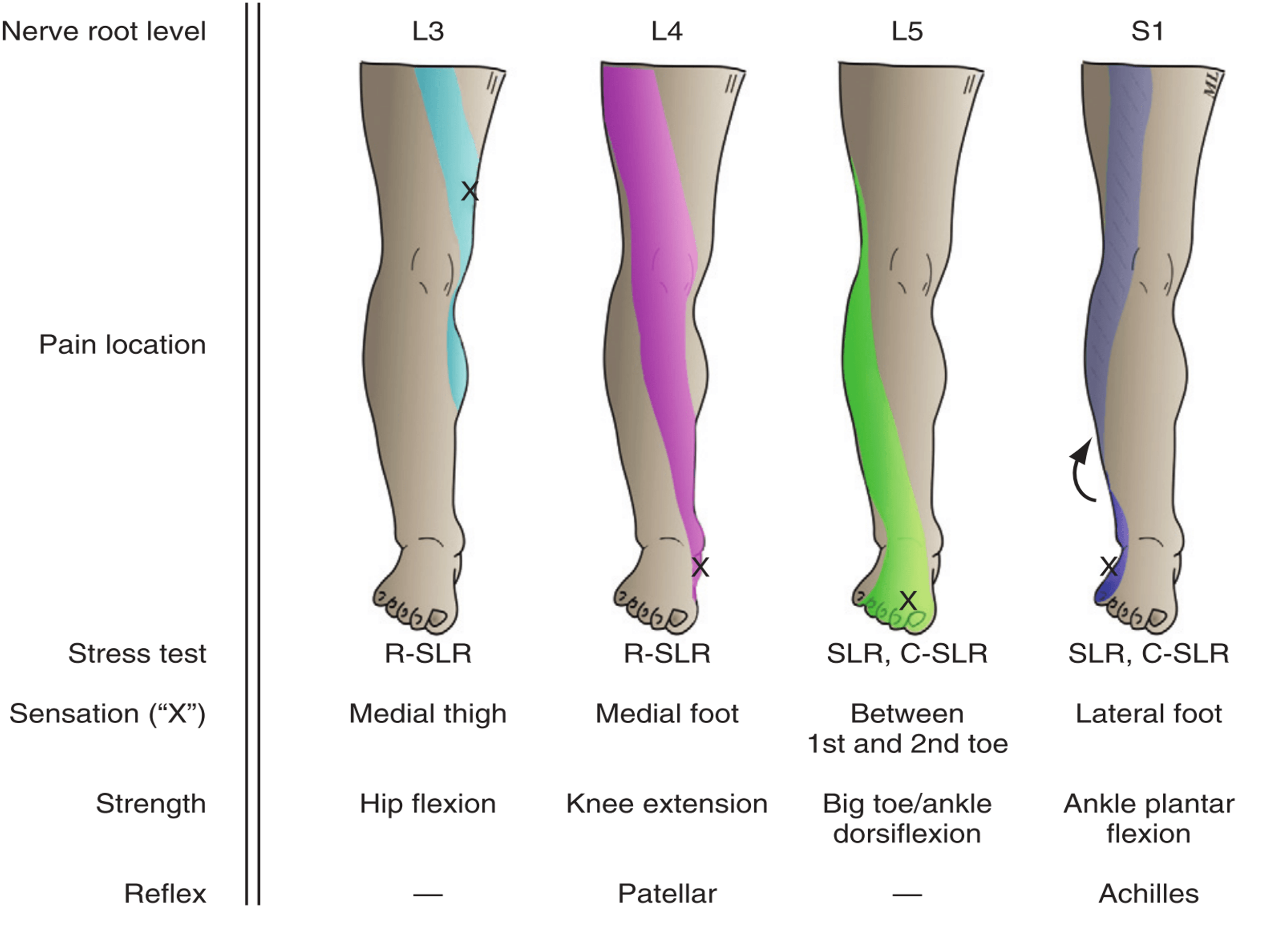
- 95% of lumbar disk herniations occur at L4-S1
- As many as 31% of people have MRI identified disk pathology that is asymptomatic
- Many asymptomatic herniations occur in people aged 30-50
- Most disc herniations extrude posterior-laterally
- This is the most common cause of sciatica (pain radiates down the posterior leg due to nerve root irritation)
- The discs start to degenerate in the 30s with increasing risk of the nucleus pulposus extruding outward and pinching a spinal nerve root
- They shrink further with age
- The spinal cord ends at L1-L2, transitioning into the cauda equina
2) List 4 red flag diagnoses and their associated history and physical
These are identified by the agency for healthcare research and quality as “cannot miss” diagnoses.
- Fracture
- Hx: of trauma or minimal trauma in an osteoporotic person
- Chronic steroid users for any reason should be x-rayed even with no trauma history
- Older than 50 yrs
- Cauda equina syndrome
- Due to sudden compression of multiple lumbar or sacral nerve roots.
- Causes: epidural abscess, hematoma, trauma, malignancy
- Hx: back pain, may have atypical, equivocal neurologic findings.
- Px: multiple, bilateral nerve root pain in both legs
- Saddle anesthesia
- Decreased rectal tone/incontinence; urinary retention
- Hx: of trauma or minimal trauma in an osteoporotic person
“The most consistent examination finding in cauda equina syndrome is urinary retention……overflow incontinence owing to a neurogenic bladder. Given the high sensitivity of urinary retention of 90% and a negative predictive value of 99.99%, this disease process is extremely unlikely if the patient’s postvoid residual urine volume is less than 100 to 200 mL. This can be measured by urethral catheterization or estimated by ultrasonography. Saddle anesthesia—sensory deficit over the buttocks, upper posterior thighs, and perineal area— frequently is an associated finding, with a sensitivity of 75%. In 60 to 80% of cases, the rectal examination reveals decreased sphincter tone.” Rosen’s Page 647
- Spinal infection
- Spinal epidural abscess or osteomyelitis of the vertebral bodies – usually Staph. Aureus
- May be: mycobacterium tuberculosis, pseudumonas
- Risk factors: immunocompromised, diabetes, alcoholism, renal failure, elderly, post-blunt trauma to the back, indwelling devices, instrumentation of the GU/GI/ENT tract
- Spinal epidural abscess or osteomyelitis of the vertebral bodies – usually Staph. Aureus
- Hx: back pain at rest, fevers and chills, neurologic deficits
- 20% of those with spinal epidural abscesses have NO risk factors or comorbid illness!
- Px: tenderness over the affected spinous process, “triad” = fever (27-50% sensitive), focal back pain, neurologic deficit (<50% of cases)
- Typical progression:
- Seeding of the disk space → discitis → spondylitis → epidural abscess
- Malignancy – primary vs. secondary
- Hx: of cancer, pain persists at rest, B symptoms, pain worse at night
- Age > 50
- Typically spread from breast, prostate , lung
- Px:
- ESR > 50 mm/hr, low hematocrit
- Spinal tenderness
- Hx: of cancer, pain persists at rest, B symptoms, pain worse at night
3) Describe SLR, crossed-SLR, flip-test, reverse SLR and their implications
- True sciatica: sharp, shooting, lancing, burning pain from the low back to below the knee
- With associated numbness or weakness
- Can be exacerbated by sitting, bending, coughing, straining
The straight leg raise:
- Sensitive for sciatica (91%) but poor specificity (26%)
- Method:
- Supine patient with legs extended.
- Symptomatic leg is passively raised (knee straight)
- Presence of radiating back pain past the knee in between 30-70 degrees suggests a L5-S1 radiculopathy
- If the leg elevation produces isolated low back pain without radiation it is negative
Two corroborative tests:
- Bowstring sign: reproduced pain with deep palpation of the taut posterior tibial nerve in the midline at the popliteal fossa
- Foot dorsiflexion test
- When the SLR is elevated just below the pain threshold
The crossed SLR:
- Passively raise the asymptomatic extended leg
- Positive if: pain radiating from the back to the opposite affected leg
Sensitivity: 29%, Specificity: 88%
Good as a “rule in” test
The “flip test”:
- An alternative to the SLR for the patient in the seated position where the knee is extended which will also stretch the sciatic nerve causing pain
- The patient may “flip back” in the supine position (arch their back in pain!)
The reverse SLR test:
- Used to detect L3-L4 radiculopathy
- Procedure:
- Patient lies prone
- Each hip is passively extended
- Positive if pain along the L3-4 nerve root is experienced
It is important to map out the patient’s pain distribution and test each nerves’ individual function, strength, reflexes, and sensation.
E.g. Test light touch and pin-prick at L4, L5, S1
Herniated disks:
- Sciatica has a high sensitivity for lumbar disk herniation (95%)
- Can have overlapping symptomatology with spinal stenosis
- Spinal stenosis:
- Age > 55. Chronic pain, and radiculopathy
- Pain relieved with rest, bending forward
- Pseudoclaudication lasts 10-15 mins, and eases off by bending forward
- Spinal stenosis:
4) List 5 indications for X-ray in low back pain

- Plain radiography
- Very low yield – for screening lumbosacral plain x-rays for all patient with acute back pain
- Should only be ordered with red flag features
- Radicular symptoms do not mean x-rays should be ordered
- Findings on X-ray:
- Spondylolysis
- Spondylolisthesis is graded 1-4
- Vertebral osteomyelitis
- Erosion of vertebral endplates, shortened disk space height
- Metastatic disease
- Spondylolysis
- Sensitivity and specificity for last two things are: 82% and 60%
- U/S
- Only use is in assessing post-void residual volume
- CT
- Finds fractures best
- MRI
- BEST test for:
- Cauda equina, spinal infection, malignancy, epidural abscess
- At risk for finding up to 30% of people with asymptomatic, incidental disc herniations or other incidental ligament/bony/alignment variations leading to damaging surgical intervention
- BEST test for:
Low risk back pain patients need an educational intervention, not an imaging intervention
[bg_faq_end][bg_faq_start]5) Discuss the discrimination of functional from organic back pain
| Functional | Organic |
| Clues from history: 1. Prolonged hx of non-anatomic pain complaints 2. Vage pain descriptions and no localization 3. Multiple lawsuits over similar problems 4. Multiple narcotic prescriptions 5. Multiple different prescribers 6. Lack of coordinated care for a problem that dominates a person’s entire life | Anatomic, life-altering, physiologic complaints |
| In search of secondary gain | In search of diagnosis and treatment |
| Clues from physical examination: 1. Negative Sitting SLR (aka “flip back test”) 2. Extreme superficial tenderness 3. Non-dermatomal sensory loss 4. Axial load on the cervical spine (head) causing pain 5. Over-reaction during physical assessment
“All of these signs are believed to correlate well with psychopathology but have poor prognostic value. They are suggestive of malingering and functional complaints but are neither sensitive nor specific enough to rule out organic pathology.51,52” From Rosen’s page 648 | objective physical findings |
6) Describe the management of:
- Fracture
- See episode 43
- Cauda Equina Syndrome
- Direct nerve irritation due to massive central disk herniation
- Management:
- Needs urgent operative decompression within 48 hrs of symptom onset
- Overflow urinary incontinence may be an exception to the 48 hr rule
- Spinal Infection
- Investigations:
- ESR, CBC, urine analysis
- ESR > 20 mm/hr has a 98% sensitivity
- If an additional risk factor present then 100% sens, and 67% spec.
- Serum WBC is of little help
- Do not do a lumbar puncture
- ESR, CBC, urine analysis
- Management:
- Collections need drainage by a neurosurgeon
- Antibiotics with MRSA and pseudomonas coverage
- Vertebral Malignancy
- Investigations
- ESR, CBC, ALP, PSA, SPEP
- X-ray, CT, MRI
- Back Pain without a history of cancer and without radiculopathy
- (Suggestive history)
- If -ve xray and -ve ESR/CRP workup can be done as an outpatient (10-20% false negative rate)
- Symptom control
- either +ve x-ray or ESR/CRP = Ct or MRI as urgent outpatient test
- Back pain without hx of cancer but radiculopathy present
- If blood work or x-ray abnormal = urgent MRI/CT to screen for impending spinal cord compression
- Back pain with hx or cancer
- Urgent CT and/or MRI regardless of x-ray/blood work
- In anyone going for MRI = they should receive dexamethasone urgently to reduce the potential mass effect
- Consider urgent radiation therapy as well
- Simple Radiculopathy
- Mobilization
- Analgesics
- Systemic vs local steroid injections – somewhat short-lived effects and somewhat controversial
- Symptoms > 4-6 weeks may indicate need for MRI and possible surgical discectomy (with similar long term results)
7) List 10 differential diagnoses for thoracic back pain
See Box 54-3
- Aortic dissection
- Pneumonia
- Myocardial infarction
- PE
- Ruptured esophagus
- Pancreatitis
- Thoracic disc herniation
- Usually not diagnosed until 20 months after the first clinical presentation!
- Tumour / hematoma with nerve impingement
- Disk infection
- Pyelonephritis

Think:
Skin (herpes zoster!) – soft tissue – chest wall – bones – joints – nerves – lungs – heart – esophagus – etc.
[bg_faq_end]Wisecracks:
[bg_faq_start]1) Back pain treatment cocktails?
EDUCATION is essential. (Diagnosis, activity suggestions, reassurance, and warning signs to watch for)
“A typical lumbosacral spine series involves as much gonadal irradiation as that incurred with a daily chest x-ray for 5-6 years!” – from Rosen’s
- Movement – will lead to earlier resolution of pain!
- Referral to physio, exercise therapy, athletic therapy
- Yoga, acupuncture, traction, massage, nerve stimulation, etc.
- Avoid heavy lifting and proper lifting technique
- NSAIDs and/or acetaminophen
- Attempts* with:
- Cyclobenzaprine
- Increased risk of falls, accidents, drug dependence, drowsiness
- Careful, almost never, use of narcotics and benzos for breakthrough symptoms
- Steroids – could be considered with evidence of radiculopathy
- Cyclobenzaprine
2) When to order the CT scan?
- Similar to box 54-1
- Better at finding fractures…and that’s it.
- Uptodate: “evaluation of low back pain in adults”
- Systematic reviews looking at early imaging for low back pain:
- Support is mainly for these red flags:
- History of cancer
- Older age
- Prolonged use of corticosteroids
- SEVERE trauma
- Presence of contusions or abrasions
- What about spinal infection concerns?
- For those people with a moderate risk for spinal infection:
- Consider ordering plain film = if abnormal → lab tests +/- MRI
- If x-ray normal and ESR/CRP high = MRI
- CRP = sensitivity 82-98% for
- Infection very unlikely with an ESR < 20 and no more than one risk factor for systemic illness
- WBC elevation. = 30% sensitivity !
- For those people with a moderate risk for spinal infection:
- Support is mainly for these red flags:
- Systematic reviews looking at early imaging for low back pain:
3) How to estimate the amount of post-void residual volume with ultrasound?
- Formula: Volume = 0.52 x bladder height in cm x width (cm) x depth (cm)
This post was edited and uploaded by Ross Prager (@ross_prager)



