This episode of CRACKCast covers Chapters 19 of Rosen’s Emergency Medicine, Dizziness and Vertigo. Dizziness is one of the most common presentations to the ED so we need to have an organized approach to these patients to discern the benign from the deadly.
Shownotes – PDF Link
[bg_faq_start]Rosen’s in Perspective:
[bg_faq_start]Dizziness
- Very common yet complex neurologic symptom, reflecting a disturbance in:
- Balance perception and spatial orientation
- It is often used as a catch all word for many things:
- Weakness, light-headedness, unsteadiness, depression, etc.
- Despite the experts not uniformly agreeing, think four historical categories:
- Vertigo – illusion of spinning or motion
- Near syncope – impending feeling of fainting
- Disequilibrium – loss of equilibrium when walking
- Non-specific dizziness
- These categories are of limited use practically, but help us think through the differential diagnosis list.
Pathophysiology
The body’s ability to regulate its equilibrium and awareness relies on:
- Visual impulses (eyes)
- Body position in space
- Proprioceptive (muscles, joints, small nerves in the body)
- Relative positions of parts of the body
- Neck position particularly important in relation to visual and otic input
- Vestibular systems (otic labyrinths)
- Maintain head position and stabilize head movement
- All these systems send information to the brain
- Connected through the cerebellum by the vestibular nuclei in the brainstem
Any disease that interferes with any of these systems gives rise to vertigo/dizzy symptoms
[bg_faq_end] [bg_faq_start]Vestibular apparatus
- Maintains head position and movement
- Within the inner ear in the temporal bone
- Vulnerable to:
- Trauma, infection, blood-borne toxins

Consists of canals and otolithic structures connected to each other containing endolymph
- Three semicircular canals
- Movement and angular momentum
- Two otolithic structures (utricle and saccule)
- Orientation with respect to gravity
- Contain CaCO3 structures called otoliths
- Both semicircular canals (either ear) work together and help people respond to symmetrically to stimuli. A disease in either inner ear or motion stimulation gives the asymmetrical perception of vertigo
- For example: when otoliths are inappropriately located in the semicircular canals (as in BPPV) they can lead to positional vertigo as the otoliths move in the semicircular canals in response to gravity
Nerve supply extending from these structures:
- Impulses from the inner ear structures leave via the acoustic nerve (CN VIII)
- Enter the brainstem below the pons and anterior to the cerebellum
- Pass through the four vestibular nuclei of the brainstem and cerebellum
They then travel on two pathways leading to the clinical manifestations of vertigo:
- Medial longitudinal fasciculus (MLF)
- Vestibulospinal tract
In normal healthy vestibular systems these connections allow for eye<->body compensation in response to movement in different directions, and maintaining a stable visual axis.
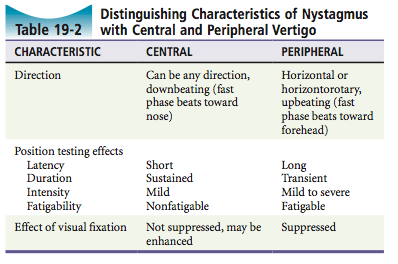
[bg_faq_end] [bg_faq_start]Nystagmus:
Occurs when the normally “synced” vestibular information becomes unbalanced
- Usually this is in unilateral vestibular disease leading to asymmetrical stimulation of the medial & lateral rectus muscles of the eye.
- Unopposed activity leads to SLOW eye movement TOWARDS the affected side of the stimulus (regardless of where the eyes are looking).
- The cerebral cortex then corrects for these eye movements and RAPIDLY brings the eyes back to midline, repeating itself cyclically and manifesting as nystagmus
Nystagmus direction is conventionally described by the FAST “cortical” component (the correction of the gaze deviation away from the diseased vestibular apparatus)
- Unilateral horizontal-rotatory nystagmus arises from vestibular disease
- Vertical nystagmus is usually a central cause – in the brainstem or cerebellum
1) Compare characteristics of peripheral and central vertigo
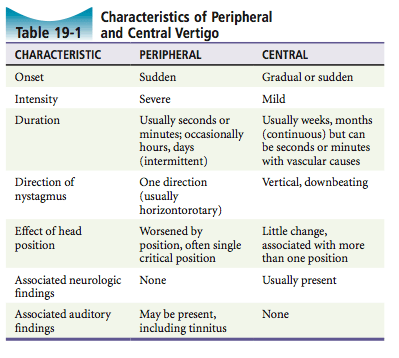
| Peripheral | Central |
| History: 1. Sudden onset 2. Severe symptoms 3. Usually seconds-minutes (may be hrs.) 4. Worsened by head position changes – may have a single comfortable position | History: 1. Advanced age 2. New onset – never occurred before 3. CAD, HTN, DM, A fib, strokes 4. Neck trauma 5. Sudden onset, severe symptoms or weeks/months of mild symptoms 6. Vertigo followed by headache 7. ALOC, altered mentation, syncope |
| Physical exam: 1. Normal neurological exam 2. May have a fever | Physical exam: 1. D’s – diplopia, dysarthria, dysmetria, dysdiadokinesis 2. Ataxia / gait disturbance / imbalance 3. Vital sign abnormalities = think central or systemic cause a. Hypotension – syncope or near syncope b. Fever – meningitis c. Pulse and blood pressure discrepancy between arms – subclavian steal syndrome / vertebrobasilar insufficiency 4. CN abnormalities (EOM’s) |
Nystagmus:
| Nystagmus:
|
Auditory findings:
| Auditory findings:
|
Fecaliths or pearls?
- There are a lot of similarities in the exam and history
- HINTS exam – to be discussed in wisecracks
2) What are risk factors for central cause or vertigo?
- TIA and stroke risk factors, including: older age, male, HTN, CAD, DM, A fib.
- Interesting facts in Rosens:
- Isolated vertigo can be the only initial sign of cerebellar and posterior circulation strokes / TIAs / infarctions
- Often missed by ED physicians
| “Stroke is seen in 3.2% of patients with dizziness syndrome, but only 0.7% of those with isolated dizziness had stroke |
| “Recent study: fewer than 1/500 of patients discharged with dizziness or vertigo had a major vascular event in the month post discharge” |
3) List 4 vestibulotoxic drugs.
- Vestibulotoxic drugs: important to consider as potential contributors to vertigo
- Aminoglycosides
- Anticonvulsants
- Alcohols
- Quinine
- Quinidine
- Minocycline
4) Describe the Hallpike Maneuver and the Epley Maneuver
Dix-Hallpike Maneuver
- “Can confirm the diagnosis of posterior canal BPPV”
- Useful diagnostic tool
EXPLANATION
- “With the head turned 45 degrees to one side while the patient is sitting up, the patient is moved to a supine position with the head hanging over the edge of the bed”
- “Patient is asked about vertigo symptoms and observed for nystagmus”
- The patient is brought back upright
- The test is repeated with the patient looking 45 degrees in the other direction (e.g. left rather than to the right)

| === If the patient has a posterior canal BPPV only one side should be positive for symptoms of nystagmus === |
=== CAVEAT ===
Roll Test
If the DH test is negative or bilaterally positive, use the “ROLL TEST”
- Examines for the horizontal canal variant of BPPV
- Useful diagnostic tool
EXPLANATION
- Patient lies supine with forward gaze (no need for head to hang over edge of bed)
- Physician turns their head 90 degrees to one side
- Patient is asked about symptoms
- Physician straightens head and turns it the other direction.
FINDINGS
- If there are otoliths in the horizontal canal the patient will develop vertigo and horizontal nystagmus, with the direction of the nystagmus will change depending on the way the head is turned.
- With horizontal canal BPPV, the patient should have symptoms with their head in either direction – but the side with the worse symptoms (e.g. looking to the right) is the side that is most involved (the right side is diseased).
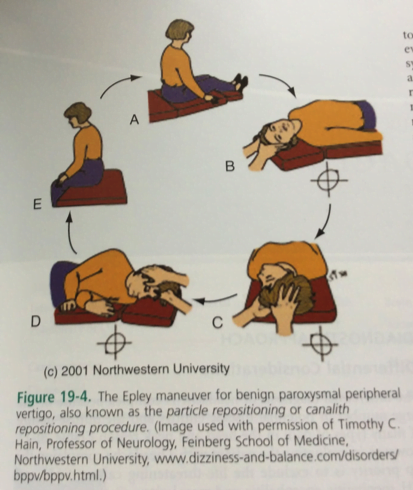
Epley Maneuver
- In essence, sequential rotations of the head 90 degrees – three times right over to left
- Useful treatment tool
- A. Started and finished in a sitting up position
- B. Lie down with head turned 45o to right
- 30 seconds or until symptoms resolve
- C. Turn head 90o left, at 45o left
- 30 seconds or until symptoms resolve
- D. Turn head additional 90o left, along with body so that patient is on left shoulder
- 30 seconds or until symptoms resolve
- E. Sit up patient
5) List 5 causes of Peripheral Vertigo + describe features of illness
Most common causes for peripheral vertigo:
- BPPV
- Short lived, positional, fatigueable – with nausea / vomiting
- NO tinnitus or hearing loss
- Vestibular neuronitis
- History: sudden severe vertigo, increasing intensity over hours → then subsiding over days to weeks. Positional changes. Usually exposure to infections, toxins.
- Physical: N/V. No auditory symptoms. Spontaneous Nystagmus.
- Labyrinthitis
- Acute suppurative
- With coexisting acute exudative inner ear infection. SEVERE symptoms
- Severe hearing loss, N/V
- Febrile patient, toxic appearing, ACUTE otitis media
- Serous
- Mild to severe positional symptoms. Pre/coexisting ENT infection
- Mild to severe hearing loss,
- Non toxic patient, with low or no fever
- Toxic
- Gradually progressive symptoms on vestibulotoxic drug
- Hearing loss, severe N/V
- Hearing loss, ataxia (if chronic)
- Meniere’ s disease
- Recurrent episodes of abrupt, severe rotational vertigo lasting HOURS. May occur in clusters with symptom free periods
- N/V. Tinnitus, hearing loss,
- Usually doesn’t have positional vertigo
- Acoustic neuroma
- Gradual onset hearing loss in women 30-60 yrs.
- Hearing loss, tinnitus; in later stages: ataxia
- Unilateral decreased hearing
- Later stages: truncal ataxia, diminution or absence of corneal reflex, CN VIII
6) List 5 causes of Central Vertigo + describe the features of illness
Most common causes of central vertigo
- Vascular disorders
- Vertebrobasilar insufficiency
- Patient with ++vascular risk factors and vertigo
- May be associated with neck trauma
- Seconds to minutes of vertigo WITH dysarthria, ataxia, weakness, numbness, double vision, headache
- Usually have neurological deficits
- Cerebellar hemorrhage
- Sudden, severe symptoms
- Headache, vomiting, ataxia
- Toxic exam, dysmetria, ataxia, ipsilateral CN VI palsy
- Posterior inferior cerebellar artery occlusion (Wallenberg’s syndrome)
- Vertigo with neurological complaints
- N/V, loss of pain and temp sensation, ataxia, hoarse voice
- Ipsilateral loss of pain and temp sensation on the side of the lesion, and contralateral palate/pharynx/larynx paralysis; Horner’s syndrome
- Head trauma
- Post trauma positional and self-limited nausea
- Rarely basilar skull fracture
- Vertebrobasilar migraine
- Vertigo → headache. Similar episodes in the past with onset in adolescence, and family history of migraines
- Headache preceded by dysarthria, ataxia, visual disturbances, paresthesias
- NO residual neurologic or otologic symptoms post-attack
- Multiple sclerosis
- 7-10% of people have vertigo as a presenting symptom.
- May be severe, occurring in 20-40 year olds
- Usually have other attacks with varying neurological signs/symptoms
- Multidirectional nystagmus which may persist after vertiginous symptoms resolve. Bilateral INO and ataxic eye movements – suggest MS
- Treat as migraine (consider trial of migraine therapy in an undifferentiated patient)
- Temporal lobe epilepsy
- Vertiginous symptoms
- May have memory impairment, hallucinations, trancelike states, epilepsy.
- May have aphasia or convulsions
- Hypoglycemia
- Should always be assessed for
- Have sweating and anxiety, tachycardia, mental status changes
Wisecracks
[bg_faq_start]1. What is the HINTS exam? – Head impulse – Nystagmus – Test of Skew
SOURCE
- Shout-out to WikEM journal club – thanks to WikEM crew
- Paper: Kattah et al. 2009
- Reported that HINTS has higher sensitivity for detecting a central cause of vertigo than MRI with DWI. (100% vs. 72%)
PERFORMING THE EXAM
- HI – Test of vestibulo-ocular reflex
- Have the patient looking at your nose, and turn their head to either side while looking at their eye movements.
- An ABNORMAL (failed) corrective saccade as you turn their head to the affected side is ‘normal’ (reassuring that it is a peripheral cause)
- Nystagmus – in primary, left and right gaze
- Looking for vertical, downbeating, non-fatigueable
- TS – alternating cover test
- Cover their eyes one at a time while they look at your nose, uncover rapidly to see if there is any corrective eye re-alignment (ask about old strabismus)
- Repeat with each eye
NOTES ABOUT THE STUDY
Exclusions: People with a history of recurrent vertigo with/without auditory symptoms
Methods: Performed in an outpatient setting by NEURO-OPHTHALMOLOGISTS
Bottom line: Is this exam practical to use clinically?
- Most people need a CTA, although this rarely changes management immediately
2) Why do people with vertigo get systemic symptoms?
- Extra-vestibular connections:
- Vestibular nuclei send info to the lateral vestibulospinal tract and connect with motor neurons that supply muscles in the extremities
- Leads to “false steps” and correcting body movements in people with disease vestibular systems who “feel” like they are moving
- There are also connections of vestibular nuclei with the autonomic system which leads to:
- Perspiration
- Nausea
- Vomiting
- Fatigue, malaise etc.
- The vestibular nuclei also connect with the cerebellum to aid in movement modulation
- Vestibular nuclei send info to the lateral vestibulospinal tract and connect with motor neurons that supply muscles in the extremities
3) What is the “barbecue roll”?
- See Rosens pg. 165
“Barbecue roll” – Used to treat the HORIZONTAL variant of BPPV:
- Patient lies supine with the head turned 90o to the affected side
- They then sequentially rotate their head 45o away from the affected side.
- Eventually the patient turns over (like a barbecue) into the prone position
- The maneuver is over when their head is in the original starting position.
NOTE: Each held for 30 seconds or until their symptoms/nystagmus terminate
[bg_faq_end]This post was copyedited and uploaded by Sean Nugent (@sfnugent)



