This episode of CRACKCast covers Rosen’s Chapter 014, Cyanosis. Here are some tips for the next time someone comes in to the Emergency Department looking a little blue.
Shownotes – PDF Link
[bg_faq_start]Rosen’s in Perspective:
Key terms:
- oxygenated vs. deoxygenated hemoglobin = saturated vs. desaturated hemoglobin
- SaO2 (arterial oxygen saturation measured/calculated by ABG) SpO2 (peripheral oxygen saturation measured by pulse oximetry)
- PaO2 PAO2 (partial pressure of O2 in the blood (measured by ABG) vs. partial pressure in the alveolus)
Cyanosis = imbalance between oxy/deoxy hemoglobin
- cyanosis is specific for hypoxia but not sensitive (can be hypoxic without cyanosis!)
- normal adults that is when deoxyhemoglobin >5g/dl
- cyanosis is about absolute amount of deoxygenated hemoglobin – anemic individuals turn blue only at lower levels of PaO2 and SaO2
1) What is the differential diagnosis for cyanosis?
Critical:
- acute heart failure
- acute coronary syndrome
- hypovolemic or cardiogenic shock
- acute respiratory failure
- massive PE
- congenital heart disease
Emergent:
- methemoglobinemia (consider when no hx/physical suggesting underlying respiratory/CVS disease)
- sulfhemoglobinemia
- rare cause of cyanosis
- most common after exposure to hydrogen sulfide from organic sources
- also from medications (sulfonamide derivatives)
- GI sources (bacterial overgrowth)
- consider when cyanotic and methemoglobin on CO-oximetry, but does not respond to methylene blue treatment
- polycythemia (elevated RBC mass)
- three main causes:
- polycythemia vera – bone marrow stem cell disorder with increase RBC mass, cyanosis, and splenomegaly
- secondary polycethmia – increase in erythropoietin (appropriate or not) in response to chronic hypoxemia
- e.g. congenital heart disease, cigarette smoking, high altitude exposure
- relative polycethemia – result of reduced plasma volume
- e.g. dehydration
- three main causes:
Non-emergent:
- Raynaud’s phenomenon
- may cause a cyanotic appearance
- 15% of the population
- F>M
2) List the common causes for methemoglobinemia

Common causes of methemoglobinemia.
Rosen’s 8th Edition. Box 14-1. Chapter 14 – page 130.
3) Describe the mechanism for methemoglobin formation, treatment, and indications for methylene blue
Pathophysiology:
- normally hemoglobin binds O2 via iron in its reduced state (Fe2+)
- if iron is oxidized it forms methemoglobin (Fe3+) – “ferric state”
- this new oxidized state cannot bind O2 and thus cannot transport O2 to tissues or remove CO2 leading to hypoxia and acidosis
- normally methemoglobin is only ~1% of total hemoglobin stores (cyanosis when greater than 10-25%)
- the body can use NADH to reduce methemoglobin back to Fe2+ (major pathway)
PEARL 1: pathognomonic sign of methemoglobinemia is dark-purple-brown or chocolate looking blood when exposed to room air
PEARL 2: second pathway to reduce methemoglobin exists using glutathione and G6PD. This is the MOA of methylene blue.
Treatment:
If cutaneous exposure, first don appropriate PPE and then decontaminate patient.
Urgent treatment with oxygen and methylene blue indicated for:
- symptomatic hypoxia (dysrhythmias, angina, respiratory distress, altered LOC, seizures)
- OR methemoglobin levels >30%
If patient does not respond to methylene blue but has elevated methemoglobinemia consider sulfhemoglobinemia
[bg_faq_end]Wisecracks:
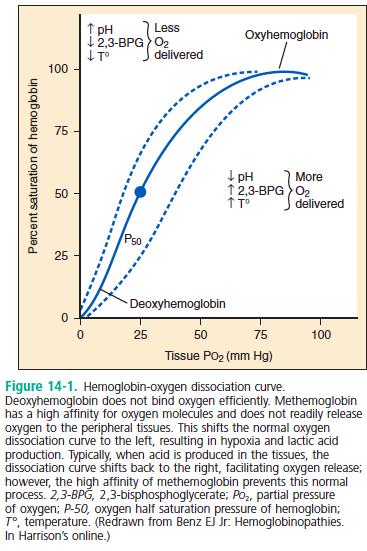
[bg_faq_start]1) Explain the oxygen-hemoglobin dissociation curve
2) What is the hyperoxia test?
Bedside test to determine the cause of cyanosis (broad categories): poor oxygenation from lung dysfunction vs. presence of R to L shunt
Official test is using a baseline ABG, and then repeating ABG after high flow O2 for 10min
- if PaO2 increases to above 150mmHg problem is with their lungs
- if PaO2 stays below 100mHg problem is likely a R to L shunt
- lots of caveats and imprecise, but potentially useful tool
Can use SpO2 instead of PaO2 and see whether patients sat improves from 88% to 100% after 10 min of high flow oxygen. If so then likely V/Q cause of hypoxia.
[bg_faq_end]This post was copyedited and uploaded by Sean Nugent (@sfnugent)


