You are working a particularly busy overnight solo coverage shift when a very sick 4-year old patient with respiratory distress begins desatting requiring urgent intubation. A team is quickly assembled and preparation is completed for the procedure. You begin attempting endotracheal tube insertion but after two failed attempts with direct laryngoscopy you ask for a bougie, and none is delivered. You ask again, and nothing. As you momentarily take your eyes off of the patient’s airway, you realize that a bougie was never gathered, and a nurse colleague is hurriedly tracking one down. As you move down your algorithm, you wonder how such a vital piece of equipment could have been missed during preparation…
The Hierarchy of Effectiveness
In a previous post, we discussed reporting patient safety events, and different forms of surveillance for detecting potentially unsafe practices in health care. However, once a patient safety event is reported and a need for change is identified, what are the options for intervention? Depending on the individual circumstances of the event, different approaches can be taken, from person-based interventions to systems based approaches, as summarized in Figure 1.1
Figure 1. The Hierarchy of Effectiveness of Patient Safety Interventions.
On one end of the hierarchy, approaches that are the most systems based in nature, such as implementation of a new forcing function often have the highest leverage in preventing patient safety events, but can be challenging to implement. In contrast, person-based approaches such as educational sessions or employing new rules are easier to implement, but have a higher tendency to fail as they rely on individual attention and vigilance. One of the more effective levels in the hierarchy is the use of checklists as a tool for improving patient safety.
Checklists as a Tool for Improving Patient Safety
Checklists have been very effective in increasing the safety profile of high risk fields such as aviation, and nuclear power plants.2 The use of checklists in medicine was widely popularized by Dr. Peter Pronovost who devised its use for the intensive care unit (ICU) where it decreased rates of central line associated bloodstream infections by 66%. This idea was a simple, and low cost solution to a problem that significantly contributed to morbidity, mortality, and healthcare costs.3 Central line infections were once thought to be inevitable in the ICU, however with widespread adoption of the checklist approach, it resulted in extensive decreases in central line infections.
Other major milestones included the introduction of the WHO surgical safety checklists, and the implementation of checklists in anesthesia, and critical care, which led to significantly reduce morbidity and mortality.4–8
So why are checklists so effective? In a system with no shortage of complexities, the introduction of checklists allows complex, error-prone procedures and processes to be distilled into manageable, stepwise components. Notably, it prevents human factors such as memory lapses from leading to patient safety events.9–12 In Dr. Gawande’s The Checklist Manifesto, he argues that checklist implementation saves us from error driven by ineptitude: having the knowledge and skills to complete the tasks at hand but failing to apply them consistently and correctly.2
Evidence Surrounding Checklist Usage in the ED
The ED’s fast pace, vulnerability to overcrowding, abundance of distractions, and complex patients makes the ED prone to cognitive overload leading to missed tasks and suboptimal performance.13–16 However, this complex and error-prone environment theoretically makes the ED the perfect setting for checklists to exist.
Checklist utility in the ED is diverse, designed to facilitate patient monitoring, patient handovers, equipment checks, medication delivery, as well as preparation for invasive procedures.16,17 However, compared to surgical specialties, the evidence surrounding checklist efficacy in the ED is relatively sparse. In the review of available studies, such as that conducted by Redfern et al. (2018) for example, implementation of an ED safety checklist in the UK was associated with faster times to obtain critical imaging and greater usage of tools to recognize deteriorating patients.18 Likewise, the implementation of checklists in strenuous scenarios such as emergency endotracheal intubation was also associated with a potential improvement in outcomes and error reduction in multiple studies, though further studies are needed to provide insight into its efficacy.19–21
Elements of an Effective Checklist and Implementation
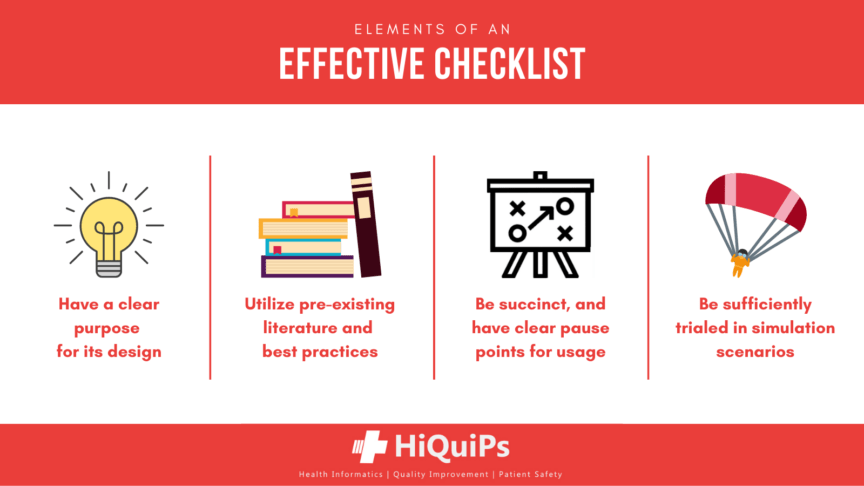
Prior literature outlines several keys to an effective checklist suggesting that effective checklists should, as summarized in Figure 2.2,16,22,23
- Have a clear purpose in its development (e.g.,emergent pediatric intubations, prevention of central line infections).
- Utilize pre-existing literature and/or best practises in its creation, such as the inclusion of specialty guidelines.
- Be succinct in its intended method of use to facilitate use in stressful situations:
- Include pertinent items that will have meaningful consequences if missed
- The point of checklists are not to explain procedures or processes, but rather to remind its users of its steps
- Its format should be rid of any clutter or distractions, and its wording exact
- Have a clear pause point in which it is supposed to be used:
- DO-CONFIRM checklists allow team members to perform their tasks from memory and experience, with a pause following to confirm all actions were completed
- Example being a pre-intubation checklist in which each all the preparation steps (including correct equipment) is read allowed and performed in a systematic manner
- READ-DO checklists, as its name suggests, enable team members to complete tasks as they are read out
- Examples including room entry procedures into isolated areas, and donning and doffing of personal protective equipment
- DO-CONFIRM checklists allow team members to perform their tasks from memory and experience, with a pause following to confirm all actions were completed
- Be sufficiently trialed in simulation scenarios prior to implementation to allow for appropriate development time and understanding of its functioning.
Figure 2. Important Considerations to Take Into Account When Making a Checklist.
While checklists are not the most challenging intervention to implement on the hierarchy of effectiveness, there are logistical challenges that exist. Common challenges include:22,24,25
- Resistance from staff, stemming from views that checklists are ineffective, or in some cases, redundant chores that slow down healthcare provision.
- Lack of training or educational sessions for the proper usage and implementation of checklists.
- Lack of organizational support.
- Faults with the checklist itself.
Taking the additional steps of forming a panel of experts, engaging stakeholders and gathering feedback during its development process may allow the process to have the appropriate buy-in and organizational support it needs to succeed.
Case Resolution
You worked through your difficult airway algorithm and successfully intubated the patient and transferred them to the Pediatric ICU. You debriefed the event with your team and highlighted learning points. The event was appropriately reported, and at your next ED department meeting it was raised as a patient safety event. After consulting with prior literature and other patient safety experts, the department begins dedicating the time and resources to creating a pre-intubation checklist to ensure all necessary steps and equipment are appropriately addressed in the future.
References
- 1.Beard P, Hoffman C, Ste-Marie M, et al. Incident Analysis Collaborating Parties. Canadian Incident Analysis Framework. Canadian Patient Safety Institute; 2012:0-148. https://www.patientsafetyinstitute.ca/en/toolsResources/IncidentAnalysis/Pages/incidentanalysis.aspx
- 2.Gawande A. London J Prim Care. 2010;3(2):124.
- 3.Pronovost P, Needham D, Berenholtz S, et al. An Intervention to Decrease Catheter-Related Bloodstream Infections in the ICU. N Engl J Med. Published online December 28, 2006:2725-2732. doi:10.1056/nejmoa061115
- 4.Bergs J, Hellings J, Cleemput I, et al. Systematic review and meta-analysis of the effect of the World Health Organization surgical safety checklist on postoperative complications. Br J Surg. Published online January 27, 2014:150-158. doi:10.1002/bjs.9381
- 5.Haynes AB, Weiser TG, Berry WR, et al. A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population. N Engl J Med. Published online January 29, 2009:491-499. doi:10.1056/nejmsa0810119
- 6.Verdaasdonk EGG, Stassen LPS, Hoffmann WF, van der Elst M, Dankelman J. Can a structured checklist prevent problems with laparoscopic equipment? Surg Endosc. Published online July 3, 2008:2238-2243. doi:10.1007/s00464-008-0029-3
- 7.Lingard L. Evaluation of a Preoperative Checklist and Team Briefing Among Surgeons, Nurses, and Anesthesiologists to Reduce Failures in Communication. Arch Surg. Published online January 1, 2008:12. doi:10.1001/archsurg.2007.21
- 8.DePalo VA, McNicoll L, Cornell M, Rocha JM, Adams L, Pronovost PJ. The Rhode Island ICU collaborative: a model for reducing central line-associated bloodstream infection and ventilator-associated pneumonia statewide. BMJ Quality & Safety. Published online December 1, 2010:555-561. doi:10.1136/qshc.2009.038265
- 9.Thomassen Ø, Espeland A, Søfteland E, Lossius H, Heltne J, Brattebø G. Implementation of checklists in health care; learning from high-reliability organisations. Scand J Trauma Resusc Emerg Med. Published online 2011:53. doi:10.1186/1757-7241-19-53
- 10.MARCUS R. Human factors in pediatric anesthesia incidents. Pediatric Anesthesia. Published online March 2006:242-250. doi:10.1111/j.1460-9592.2005.01771.x
- 11.Shillito J, Arfanis K, Smith A. Checking in healthcare safety: theoretical basis and practical application. International J Health Care QA. Published online October 5, 2010:699-707. doi:10.1108/09526861011081831
- 12.Cooper JB. Preventable anesthesia mishaps: a study of human factors. Quality and Safety in Health Care. Published online September 1, 2002:277-282. doi:10.1136/qhc.11.3.277
- 13.Bigham BL, Bull E, Morrison M, et al. Patient safety in emergency medical services: executive summary and recommendations from the Niagara Summit. CJEM. Published online January 2011:13-18. doi:10.2310/8000.2011.100232
- 14.Jepson ZK, Darling CE, Kotkowski KA, et al. Emergency department patient safety incident characterization: an observational analysis of the findings of a standardized peer review process. BMC Emerg Med. Published online August 8, 2014. doi:10.1186/1471-227x-14-20
- 15.Brubacher J, Hunte G, Hamilton L, Taylor A. Barriers to and Incentives for Safety Event Reporting in Emergency Departments. hcq. Published online July 15, 2011:57-65. doi:10.12927/hcq.2011.22491
- 16.Hearns S. Checklists in emergency medicine. Emerg Med J. Published online June 15, 2018:530-531. doi:10.1136/emermed-2018-207782
- 17.Stone T, Banks J, Brant H, et al. The introduction of a safety checklist in two UK hospital emergency departments: A qualitative study of implementation and staff use. J Clin Nurs. Published online January 30, 2020:1267-1275. doi:10.1111/jocn.15184
- 18.Redfern E, Hoskins R, Gray J, et al. Emergency department checklist: an innovation to improve safety in emergency care. BMJ Open Qual. Published online September 2018:e000325. doi:10.1136/bmjoq-2018-000325
- 19.Smith KA, High K, Collins SP, Self WH. A Preprocedural Checklist Improves the Safety of Emergency Department Intubation of Trauma Patients. Reardon R, ed. Acad Emerg Med. Published online July 20, 2015:989-992. doi:10.1111/acem.12717
- 20.Long E, Cincotta DR, Grindlay J, et al. A quality improvement initiative to increase the safety of pediatric emergency airway management. von Ungern-Sternberg B, ed. Pediatr Anaesth. Published online October 24, 2017:1271-1277. doi:10.1111/pan.13275
- 21.Turner JS, Bucca AW, Propst SL, et al. Association of Checklist Use in Endotracheal Intubation With Clinically Important Outcomes. JAMA Netw Open. Published online July 2, 2020:e209278. doi:10.1001/jamanetworkopen.2020.9278
- 22.Verdaasdonk EGG, Stassen LPS, Widhiasmara PP, Dankelman J. Requirements for the design and implementation of checklists for surgical processes. Surg Endosc. Published online July 18, 2008:715-726. doi:10.1007/s00464-008-0044-4
- 23.Hales B, Terblanche M, Fowler R, Sibbald W. Development of medical checklists for improved quality of patient care. International Journal for Quality in Health Care. Published online November 16, 2007:22-30. doi:10.1093/intqhc/mzm062
- 24.Close KL, Baxter LS, Ravelojaona VA, et al. Overcoming challenges in implementing the WHO Surgical Safety Checklist: lessons learnt from using a checklist training course to facilitate rapid scale up in Madagascar. BMJ Glob Health. Published online September 2017:e000430. doi:10.1136/bmjgh-2017-000430
- 25.Mahmood T, Mylopoulos M, Bagli D, Damignani R, Aminmohamed Haji F. A mixed methods study of challenges in the implementation and use of the surgical safety checklist. Surgery. Published online April 2019:832-837. doi:10.1016/j.surg.2018.09.012
Senior Editor Ahmed Taher @ak_taher
Junior Editor Sabrina Campbell @SabrinaMCamp
This post was copyedited by Sabrina Campbell