Indications
- Percutaneous abscess drainage. An abscess is an inflamed collection of pus, the area is usually tender, warm, firm, & fluctuant to palpation. Any abscess, however small, must be drained for complete resolution. Sometimes there is surrounding cellulitis or lymphangitis and, in the more serious case, fever.
Possible Complications
- Risk of bleeding (damage to adjacent blood vessels)
- Dissemination of infection (sepsis, bone & joints, endocarditis)
- Injury of local nerves
- The procedure may not be successful & the abscess may not be completely drained due to loculated collections
Contraindications to Incision and Drainage
- Do not attempt to incise a pulsating mass (could be a hemangioma or pseudo-aneurysm).
- Large, extensive, and complex abscesses, both size and depth, especially if deeper tissues are involved, such as bone (osteomyelitis) or muscles.
- Risk of neurovascular damage such as adjacent to major blood vessels and nerves.
- Anal, perirectal abscess, and pilonidal abscess due to risk for development of fistulas.
- Deep infections of the hands are not simple cutaneous abscesses. When significant pain and swelling exists or there is pain on range of motion of a finger, seek surgical consultation.
- Do not fully “pack” an abscess cavity with ribbon gauze. This may actually trap pus within the cavity, inhibit drainage, and enlarge the eventual scar. The idea is to insert the gauze across all the surfaces of the cavity and provide some degree of debridement when the gauze is removed.
Definitions1
- Pustule
- smaller abscess that can be opened with a scalpel/needle
- Infected epidermoid (or sebaceous) cysts
- chronic reappearing fluid collection. Should be referred for complete excision of the cyst after the infection and inflammation have resolved to prevent recurrence
- Folliculitis
- superficial infection of the hair follicle. Minor uncomplicated cases can be treated with warm compresses and gentle cleansing with antibacterial soap
- Furuncle or boil
- extension of a folliculitis infection into the subcutaneous tissue. May require I&D and warm compresses
- Carbuncle
- coalescence of individual furuncles, resulting in a large painful nodule -located on the back of the neck and generally require I&D with blunt dissection using a hemostat to break up the interconnected loculations of pus. Warm compresses and antibiotics are usually indicated
- Hidradenitis Suppurativa
- Chronic inflammatory condition of the apocrine glands in the axilla and groin. Secondary infection typically results in abscess formation and fistulization requiring I&D and antibiotics. Pts can have a history of self- squeezing to pop abscess, important to assess degree of infection and systemic signs, follow up with dermatology or surgery where required
- Pilonidal cyst abscess
- Relatively common finding in the sacrococcygeal region- Escherichia coli is a frequent infecting organism commonly- Drainage should include a search for and removal of hair and follicular tissue at the base of the abscess cavity, consider surgery consult where needed
- Pointing:
- where the abscess is close to the skin surface , where the skin is thinned, and pus may eventually break through to drain spontaneously
Environment, Material and Equipment Checklist
Environment
- Adjust the light for visibility
- Adjust bed height for ease of procedure
- Use a side table or cart for procedural material
- Keep a trash can nearby for proper disposal of waste
Medications
- Sterile solution: normal saline wash, chlorhexidine, betadine. Normal saline or sterile water can be used for irrigation. However, there is evidence that there is no statistical difference between infection rates with sterile saline wound irrigation compared to potable tap water irrigation. Potable tap water is a safe option for wound irrigation and should be considered if cost or availability of sterile saline is an issue.
- Local anesthetic in a 5 ml syringe (one of the following):
- Lidocaine 1% with 1:100,000 epinephrine
- Bupivacaine 0.25% or 0.5%, with or without epinephrine*
- Bupivacaine can be used if need for longer anesthetic for large/complex wounds
- Lidocaine/Epinephrine/Tetracaine (LET) gel – useful for open wounds in children. Apply under a tegederm bandage
- Sodium Bicarbonate (NaHCO₃): One part sodium bicarbonate to 10 parts local anesthesia with epinephrine may be added into premixed bottles of lidocaine with epinephrine to lessen the local burning during infiltration.
- *Note: The added epinephrine helps with additional hemostasis, and increased concentration at the injection site. However, it has been classically taught that its inclusion with local anesthetic should be avoided in use in the ears, tip of the nose, distal phalanges, and the penis, because the vasoconstrictive effect of the epinephrine may cause local tissue necrosis. While this theory has been mostly debunked in the literature, the use of local anesthetic with epinephrine in these sensitive locations is controversial2–7.
Materials
- Gauze (4″ bx 4″), sterile sheets, bandage & tape for dressing
- Sterile ribbon gauze half or quarter inch, depending on the size of the unroofed cavity
- Window drape for wound, Sterile gloves
- Needles of various size for administration of local anesthetic
Equipment within an Incision and Drainage Tray
- Field block: large 27 G needle filled with anesthetic
- Sponge-holding forceps
- Surgical blade, Nos. 11 and 15
- Curved artery forceps/ hemostat
- 60 ml syringe with Normal saline to irrigate the wound
- Toothed forceps
- Scissors
Points to Focus on
Pre-procedure Preparation Considerations
- Complete History and physical is essential. Document vital signs, use of anticoagulants or steroids, immunocompromised status, and tetanus status. Assess any bony or joint involvement. Remember to assess comorbidities and social determinants of health that may hamper with wound care. Ask about foreign bodies or trauma.
- Immunocompromised patients or those with symptoms and signs of systemic toxicity, such as tachycardia and hypotension will require blood work, and septic evaluation. Blood and wound cultures are recommended in such cases.
- Skin and wound should be washed with antiseptic solution.
- Wash hands , wear sterile gloves , prepare the sterile field and place the window drape around the wound. Consider having a suction set up, and wearing visor or eye protecting equipment for large abscesses.
- Ultrasound can be used to help differentiate an abscess from complex cellulitis or phlegmon and determine maximum area of fluctuance.
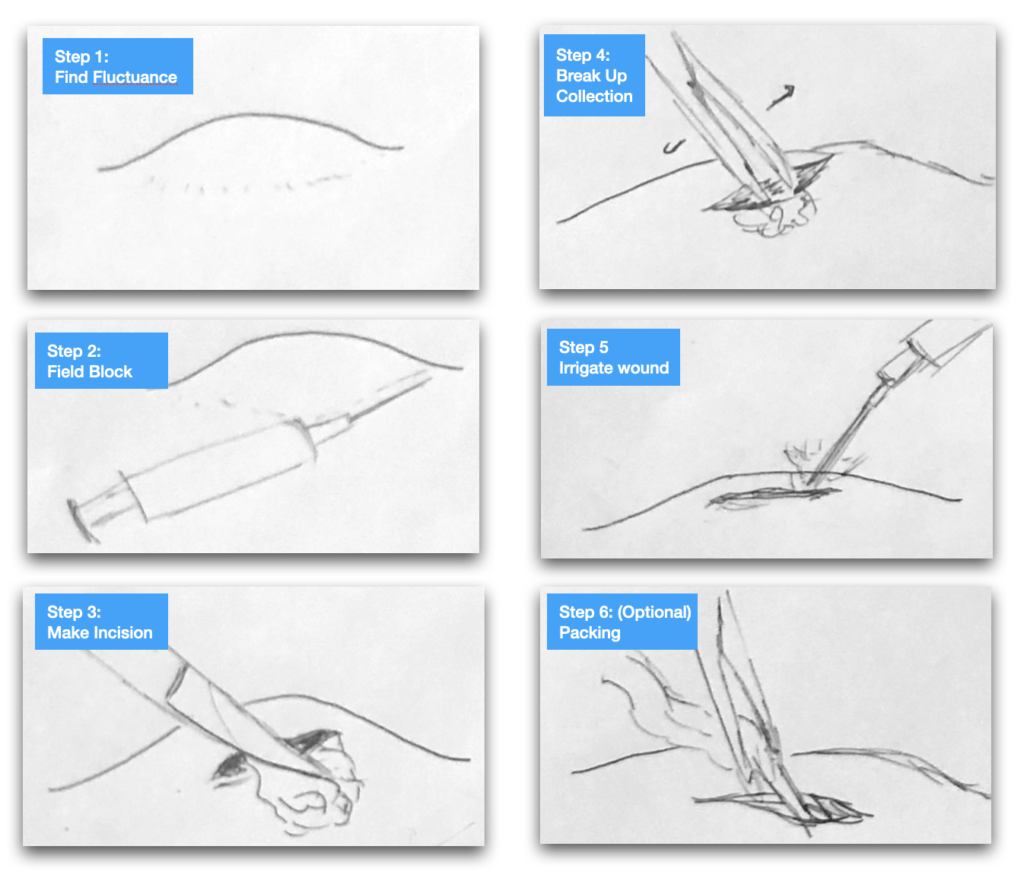
Procedure
Prepare
- Prepare the overlying skin for incision and drainage with povidone-iodine solution/ other antiseptic prep
- Small collections: Inject lidocaine superficially into the roof of the abscess along the line of the projected incision
Field Block – Medium to large collections
- Perform a field block by injecting a circumferential area of subcutaneous 1% or 2% lidocaine around the abscess, approximately 1 cm peripheral to the erythematous border
- Form a wheal of lidocaine forming a ring around the abscess as you advance the needle gently and infiltrating at the same time.
- Avoid going through the infected areas
- In addition to infiltration in in a ring, anesthetize across the dome of the abscess where you plan to make the incision
The Incision
- Using an 11 straight blade make an incision along the most fluctuant part of the abscess
- If required to culture, collect the specimen on the swab for sensitivity
Blunt dissection of the abscess
(Caution: painful step, add more local anesthetic if warranted)
- With the hemostat/artery forcep, explore & break up loculations to release pockets of collections
- Use 4 X 4 gauze to clean the pus
- Squeeze out the contents with gentle pressure and clean the pocket
Irrigation
- 60 cc syringe filled with Normal saline and a protective cap if available
- Flush the cavity thoroughly
Packing and Dressing
- Packing allows to keep the wound open and drain while healing over a course of time. Not all abscess need to be packed. (depending on case to case variation and clinician’s discretion)
- Consider packing larger than 5cm abscesses, or immunocompromised patients
- Remember to pack only loosely, introducing the ribbon with the help of hemostat
- Depending on your local guidelines, the packing gauze may or may not be soaked with antiseptic solution such as saline
- Leave a tail end of ribbon hanging outside the abscess
- Cover with gauze, dressing, and tape
Post-Procedure Considerations
- Dispose of all the sharps in a sharps-container, and gauze in the safe bodily fluids disposal bin
- Wash and dry the wound well, cleaning out any remaining clots or debris
- Cleanse the open surface with normal saline and cover with a dressing
Role of Antibiotics8,9
Uncomplicated abscesses with no symptoms or signs of systemic involvement respond well to incision and drainage and appropriate wound care.
Check your specific hospital guidelines for specific local antibiotic resistance as well as dosing and duration.
Severe Purulent SSTI
- IV Piperacillin/Tazobactam and Vancomycin; or
- Oral or IV Clindamycin (same bioavailablity); or
- IV Linezolid
Mild/Moderate Purulent SSTI – chose one or combination
- Oral TMP/SMX; or
- Oral or IV Clindamycin; or
- Oral Doxycycline
In the setting of systemic disease or an immunocompromised host, blood and wound cultures are recommended. Oral or intravenous (IV) antimicrobial therapy is then started empirically, depending on the severity of the infection
Of note, if no overlying cellulitis or comorbid conditions, Choosing Wisely Canada recommends discussing the use of antibiotics with patients as the benefits conferred by antibiotics may not outweigh the risks associated with their use.
For more information about the use of antibiotics for skin and soft tissue infections, check out the related post in the primer!
Aftercare & Discharge Instructions
| S– Symptomatic: Pt may take acetaminophen for pain relief, or antibiotic if prescribed E– Educate: keep the wound dry, change the dressing and observe for discharge and foul smell. The patient should be instructed to use warm compresses and cleanse the area R- Reassure the patient, return to work precautions F– Follow up appointment with a primary care physician or wound care nurse ideally within the next 48 hours to reevaluate the wound A– Alarm signs: increased soreness around wound, white or yellow discharge, any foul-smelling discharge, uncontrolled bleeding, or fever over 38 degrees, redness around the wound increasing in size D– Document the encounter, procedure and preferably draw the wound for reference. Always document the discharge instructions given. Document tetanus status |
* Follow up with the patient, preferably in the primary care setting for wound assessment and suture removal based on the type and location of suture placed. Arrange for wound dressing with nurse in wound clinic where available
Patient Education Tools
Recommended Reading, Videos, and Podcasts
- CanadiEM – Skin Infections
- Hippo Education-Soft Tissue Abscess Drainage (14 min video (American content)
- Teach me surgery Surgical Skills – Abscess Drainage (2 min video)
- Role of Antibiotics: Medscape
- Hippo Education: Urgent Care Bootcamp- Soft Tissue Abscess Drainage – 14 min video
- Anesthesia Key-Cutaneous Abscess Drainage and Field Block
- Skilled physicians group- Incision and Drainage of Abscess (1 min video)
The following is part of the CanadiEM Frontline Primer. An introduction to the primer can be found here. To return to the Primer content overview click here.
This post was edited by Dr. Geoff Comp DO. This post was copyedited and uploaded by Johnny Huang.
References
- 1.Anesthesia Key . Cutaneous Abscess or Pustule. Anesthesia Key. https://aneskey.com/cutaneous-abscess-or-pustule/. Published August 11, 2016.
- 2.Häfner H, Röcken M, Breuninger H. Epinephrine-supplemented local anesthetics for ear and nose surgery: clinical use without complications in more than 10,000 surgical procedures. J Dtsch Dermatol Ges. 2005;3(3):195-199. doi:10.1111/j.1610-0378.2005.04758.x
- 3.Ilicki J. Safety of Epinephrine in Digital Nerve Blocks: A Literature Review. J Emerg Med. 2015;49(5):799-809. doi:10.1016/j.jemermed.2015.05.038
- 4.Schnabl S, Herrmann N, Wilder D, Breuninger H, Häfner H. Clinical results for use of local anesthesia with epinephrine in penile nerve block. J Dtsch Dermatol Ges. 2014;12(4):332-339. doi:10.1111/ddg.12287
- 5.Krunic A, Wang L, Soltani K, Weitzul S, Taylor R. Digital anesthesia with epinephrine: an old myth revisited. J Am Acad Dermatol. 2004;51(5):755-759. doi:10.1016/j.jaad.2004.05.028
- 6.Stevens D, Bisno A, Chambers H, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):e10-52. doi:10.1093/cid/ciu444
- 7.Denkler K. A comprehensive review of epinephrine in the finger: to do or not to do. Plast Reconstr Surg. 2001;108(1):114-124. doi:10.1097/00006534-200107000-00017
- 8.Singhal H. Skin and Soft Tissue Infections – Incision, Drainage, and Debridement Periprocedural Care,Antimicrobial therapy. Medscape. https://emedicine.medscape.com/article/1830144-periprocedure#b. Published May 10, 2018.
- 9.DeClerck M. Standard Incision and Drainage with Dr. Matt DeClerck. Hippoeducation, Urgent care bootcamp. https://www.hippoed.com/urgentcare/bootcamp?utm_source=YouTube&utm_medium=social&utm_campaign=20200303–YouTube–social–UCB–AbscessDrainage. Published February 28, 2020.


