10 ED practice points based on current clinical practice guidelines
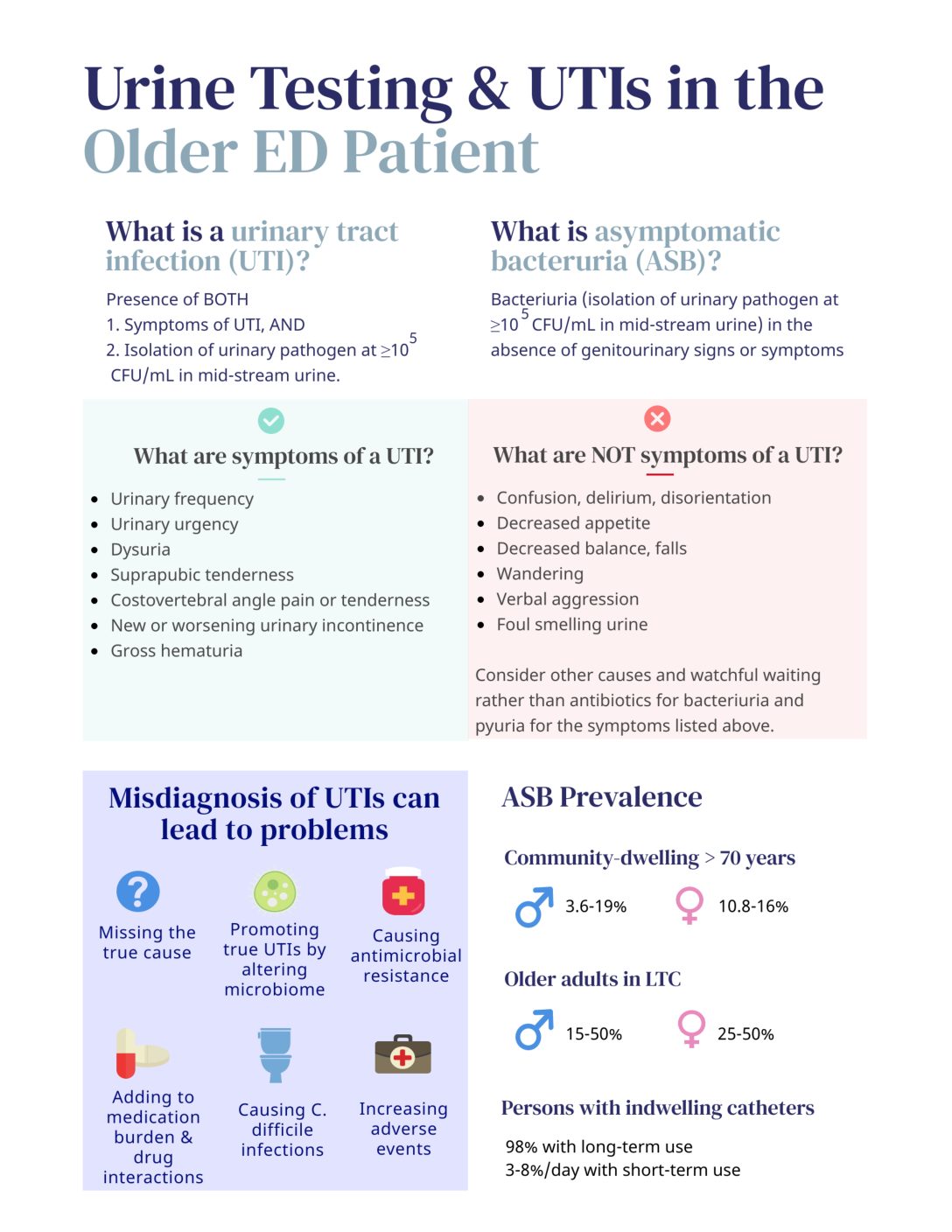
1. Focus on a change in urinary symptoms. Chronic urinary incontinence or dysuria can be common.
2. Watchful waiting is okay. For patients with non-localizing symptoms consider the alternative diagnosis before sending urine tests. If pyuria is present, consider a period of observation with hydration. Follow the clinical course and C&S results, while investigating other causes1,2.
3. Foul smelling, dark, and/or cloudy urine without urinary symptoms should not be investigated. These signs are more typical of dehydration than infection3.
4. Do not screen for bacteriuria or treat with antimicrobials unless specific urinary tract symptoms are present. Screening for and treatment of ASB is only recommended before urologic procedures where mucosal bleeding is anticipated4–6.
5. Avoid routine urinalysis or urine dips in the ED. These should be sent only if there are focal urinary symptoms. Pyuria does not differentiate between ASB and UTI. A urine dipstick and microscopy with pyuria has a PPV 32-34% and NPV > 90% for a positive urine culture6–9.
6. Start broad-spectrum antimicrobials against urinary and non-urinary sources in older patients with bacteriuria and systemic signs consistent with sepsis and no other localizing source4.
7. Do not screen for or treat ASB in patients with indwelling catheters4.
8. UTI should not be high on the differential diagnosis of weakness, delirium, increased falls, or acute functional decline unless there are clear new UTI symptoms3,4,10,11.
9. Antibiotic treatment of ASB in older hospitalized patients does not improve outcomes, but is associated with longer hospitalizations and other adverse effects12,13.
10. Treat a UTI for appropriate durations: uncomplicated cystitis for 3-5 days, complicated cystitis (male, catheterization, urological abnormalities) for 7 days, and acute pyelonephritis for 7-10 days14.
This post was copyedited and uploaded by Maham Khalid.
References
- 1.Burkett E, Carpenter C, Arendts G, Hullick C, Paterson D, Caterino J. Diagnosis of urinary tract infection in older persons in the emergency department: To pee or not to pee, that is the question. Emerg Med Australas. 2019;31(5):856-862. doi:10.1111/1742-6723.13376
- 2.Cortes-Penfield N, Trautner B, Jump R. Urinary Tract Infection and Asymptomatic Bacteriuria in Older Adults. Infect Dis Clin North Am. 2017;31(4):673-688. doi:10.1016/j.idc.2017.07.002
- 3.Blondel-Hill E, Patrick D, Nott C, Abbass K, TY Lau T, German G. AMMI Canada position statement on asymptomatic bacteriuria. Official Journal of the Association of Medical Microbiology and Infectious Disease Canada. Published online March 2018:4-7. doi:10.3138/jammi.3.1.02
- 4.Nicolle LE, Gupta K, Bradley SF, et al. Clinical Practice Guideline for the Management of Asymptomatic Bacteriuria: 2019 Update by the Infectious Diseases Society of Americaa. Clinical Infectious Diseases. Published online March 21, 2019. doi:10.1093/cid/ciy1121
- 5.Five things physicians and patients should question. Choosing Wisely Canada . https://choosingwiselycanada.org/geriatrics/
- 6.Diagnosis and Management of Urinary Tract Infection in Long Term Care Facilities Clinical Practice Guideline. Accelerating Change Transformation Team Alberta Doctors . https://actt.albertadoctors.org/CPGs/Lists/CPGDocumentList/urinary-tract-infection-guideline.pdf
- 7.Ducharme J, Neilson S, Ginn J. Can urine cultures and reagent test strips be used to diagnose urinary tract infection in elderly emergency department patients without focal urinary symptoms? CJEM. 2007;9(2):87-92. doi:10.1017/s1481803500014846
- 8.Yusuf E, Van H, van S. Performance of urinalysis tests and their ability in predicting results of urine cultures: a comparison between automated test strip analyser and flow cytometry in various subpopulations and types of samples. J Clin Pathol. 2017;70(7):631-636. doi:10.1136/jclinpath-2016-204108
- 9.Boscia J, Abrutyn E, Levison M, Pitsakis P, Kaye D. Pyuria and asymptomatic bacteriuria in elderly ambulatory women. Ann Intern Med. 1989;110(5):404-405. doi:10.7326/0003-4819-110-5-404
- 10.Caterino J, Kline D, Leininger R, et al. Nonspecific Symptoms Lack Diagnostic Accuracy for Infection in Older Patients in the Emergency Department. J Am Geriatr Soc. 2019;67(3):484-492. doi:10.1111/jgs.15679
- 11.Mayne S, Bowden A, Sundvall P, Gunnarsson R. The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing – a systematic literature review. BMC Geriatr. 2019;19(1):32. doi:10.1186/s12877-019-1049-7
- 12.Petty LA, Vaughn VM, Flanders SA, et al. Risk Factors and Outcomes Associated With Treatment of Asymptomatic Bacteriuria in Hospitalized Patients. JAMA Intern Med. Published online November 1, 2019:1519. doi:10.1001/jamainternmed.2019.2871
- 13.Dasgupta M, Brymer C, Elsayed S. Treatment of asymptomatic UTI in older delirious medical in-patients: A prospective cohort study. Arch Gerontol Geriatr. 2017;72:127-134. doi:10.1016/j.archger.2017.05.010
- 14.Using Antibiotics Wisely in Long-Term Care. Choosing Wisely Canada. https://choosingwiselycanada.org/campaign/antibiotics-ltc/
- 15.Nicolle L. Urinary Tract Infections in the Older Adult. Clin Geriatr Med. 2016;32(3):523-538. doi:10.1016/j.cger.2016.03.002
- 16.Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, Prevention, and Treatment of Catheter-Associated Urinary Tract Infection in Adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clinical Infectious Diseases. Published online March 1, 2010:625-663. doi:10.1086/650482
- 17.Rowe T, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28(1):75-89. doi:10.1016/j.idc.2013.10.004
- 18.Warren J, Tenney J, Hoopes J, Muncie H, Anthony W. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146(6):719-723. doi:10.1093/infdis/146.6.719