Welcome to “Tox in 10,” a new infographic series that exposes learners to medical toxicology topics that they can absorb in 10 minutes or less! This series is meant to introduce medical students and junior residents to the wonderful field of toxicology in an easy-to-reference-to manner! Each infographic covers the basics of the principles of toxicity, clinical features, diagnostic testing, management, and disposition that is associated with a specific toxic substance or toxidrome.1
Today we will be looking at anticholinergics!
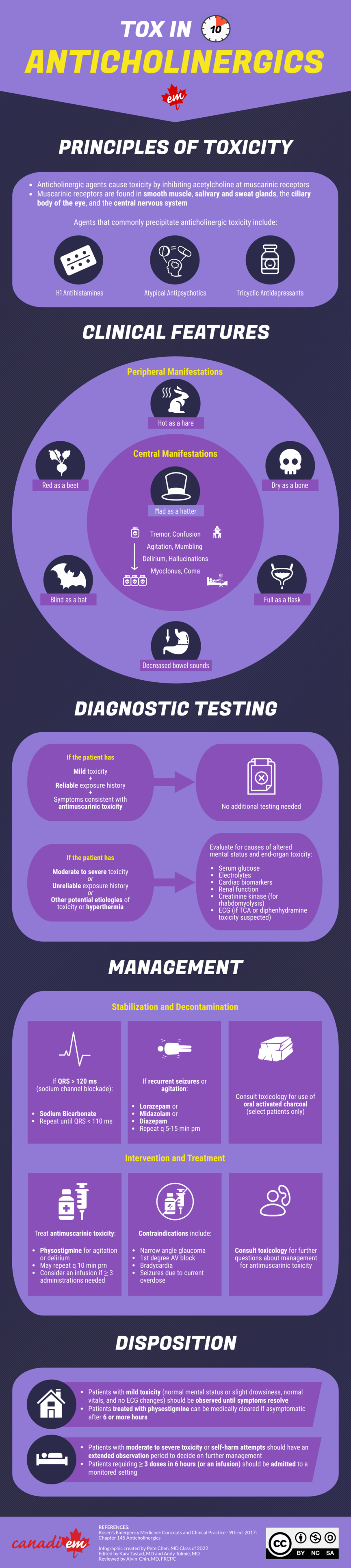
Anticholinergic agents cause toxicity through inhibiting acetylcholine receptors. A subset of these agents known as “antimuscarinics” is what produces the anticholinergic toxidrome. We will therefore be using the term “antimuscarinics” throughout the rest of the infographic.
Antimuscarinic agents have been used medicinally from antiquity to present day. When taken in toxic doses, these agents can affect both the peripheral nervous system (PNS) and the central nervous system (CNS). Most patients who exhibit mild symptoms do not usually require additional testing and may be observed in the ED until symptoms resolve. Other patients may require some level of investigations and management, such as administration of physostigmine for ongoing agitation or delirium.
Check out our infographic for more details, and let us know if you find the infographic useful and/or have suggestions on how we can improve! We would love to hear your feedback, as it would help us titrate the amount and level of content in future infographics for medical students and junior residents. We want to keep it above the minimum effective dose but under the maximum effective dose for learning.
Stay tuned for our next infographic on acetaminophen toxicity!

References
- 1.Monte AA, Hoppe JA. Anticholinergics. In: Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Elsevier; 2017:1863-1867.
Expert Review
While uncommon, anticholinergic (muscarinic) toxicity is an important differential to include in the hot and altered patient. Prompt recognition of the signs and symptoms, along with knowledge of common drugs with anticholinergic properties, will expedite appropriate treatment of the toxic patient. As always with toxicological emergencies, seek guidance from your local poison center as local treatment practices may differ.