Inhalational injuries occur as a complication of approximately one-third of burns and may lead to significant morbidity and mortality if not correctly managed.1 Inhalational injury to the upper airway can occur as a result of direct thermal injury, leading to airway swelling and necessitating the need for early intubation for airway protection.2 Inhalational injuries can also damage the lower airways due to exposure to smoke and other chemicals. Respiratory distress may be further exacerbated by exposure to carbon monoxide, cyanide, and the development of methemoglobinemia.2 Lower airway injuries can result in delayed respiratory failure, occurring up to 48 hours after the initial injury.2
The literature currently demonstrates no clear consensus on criteria for intubation in patients with inhalation injuries, making it challenging to predict which patients with inhalational injuries will require intubation.3 As a result, recent research suggests that providers have moved towards a more aggressive prophylactic intubation strategy.3 It is important to consider the risks associated with intubation and mechanical ventilation when choosing an airway management strategy.
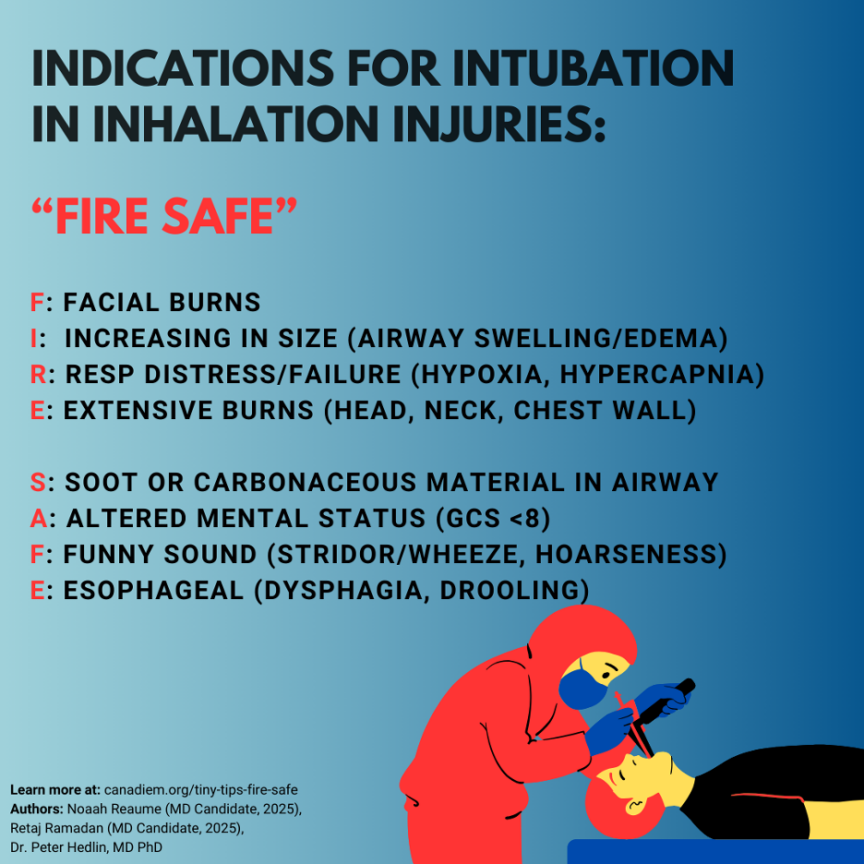
The decision to intubate should be made with consideration of the individual clinical context. The mnemonic FIRE SAFE highlights the most important criteria when considering early intubation in burn patients.2
F: Facial burns
I: Increasing in size (airway swelling/edema)
R: Respiratory distress or failure (hypoxia, hypercapnia)
E: Extensive burns (head, neck, chest wall)
S: Soot or carbonaceous material in airway
A: Altered mental status (GCS <8)
F: Funny sound (stridor/wheeze, hoarseness)
E: Esophageal symptoms (dysphagia, drooling)
This post was reviewed by Dr. Daniel Ting and copy-edited by Noaah Reaume.
References:
- 1.Heimbach D, Waeckerle J. Inhalation injuries. Ann Emerg Med. 1988;17(12):1316-1320. doi:10.1016/s0196-0644(88)80357-3
- 2.Badulak J, Schurr M, Sauaia A, Ivashchenko A, Peltz E. Defining the criteria for intubation of the patient with thermal burns. Burns. 2018;44(3):531-538. doi:10.1016/j.burns.2018.02.016
- 3.Palmieri T. Inhalation injury: research progress and needs. J Burn Care Res. 2007;28(4):549-554. doi:10.1097/BCR.0B013E318093DEF0
Reviewing with the Staff
Dr. Hedlin has reviewed this article and approved its content.