Case Presentation
You are a clinical clerk on your rural family medicine rotation working in the local emergency department. Your preceptor asks you to see a 25-year-old male who presents shortly after having hit his left index finger with a hammer while building a new deck this afternoon. He is otherwise healthy, he is not taking any medications, and he has no known drug allergies. He is right-handed and works as an electrician. He appears well, his vital signs are within normal limits, and he denies any other injuries besides his left index finger. The involved fingernail is intact, but there is an area of dark blue-black discolouration starting at the proximal nail fold and involving more than 50% of the nail. The remainder of the left second finger and hand appear normal. There is no obvious bleeding or deformity. The involved finger has normal neurovascular status and normal extension at the distal interphalangeal (DIP) joint.
Management Plan
As you review a management plan with your preceptor, she asks you a few questions
[bg_faq_start]1. What is the medical name for this injury?
A subungual hematoma refers to the collection of blood under a fingernail or toenail following a traumatic injury to the distal phalanx. Patient’s often present with blue-black discoloration under the nail and describe the pain as throbbing
[bg_faq_end][bg_faq_start]2. What are the clinically relevant features of nail anatomy?
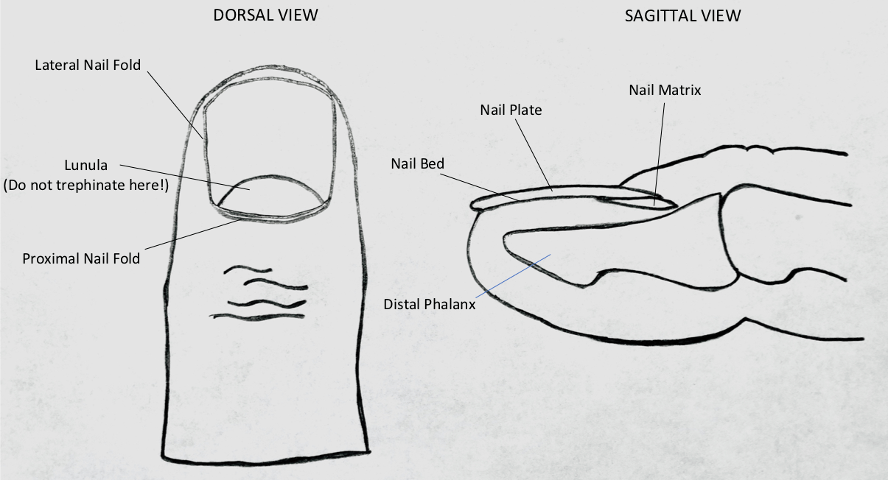
- Nail Folds: the nail is surrounded on three sides by the lateral and proximal nail folds.
- Lunula: the white crescent-shaped area of the nail along the proximal nail edge. This corresponds to the distal portion of the nail matrix.
- Nail Matrix: a collection of specialized epithelial cells that are responsible for nail growth. It begins 7-8 mm under the proximal fold and its distal end is the lunula. The matrix is anchored to the periosteum of the distal phalanx.
- Nail bed: highly vascularized area of skin underneath the nail that is adherent to the nail.
3. What other injuries are important to rule out that are commonly associated with this injury?
- Distal phalanx fracture
- Mallet finger – injury to the distal extensor tendon
- Fingertip avulsion
- Nail bed laceration
4. Does this patient need an X-ray of the affected digit?
Distal phalanx fractures are commonly associated with subungual hematomas, especially when the hematoma involves more than 50% of the nail bed. In one series of 47 patients with subungual hematoma, 32% had an associated distal phalangeal fracture.1 Given that the presence of a fracture of the distal phalanx would affect our management plan, it would be reasonable to obtain AP, lateral, and oblique views of his injured finger.
[bg_faq_end][bg_faq_start]5. Some subungual hematomas will require a procedure called nail trephination. What is nail trephination? Describe the indications, contraindications, potential complications, and procedure.2
Nail Trephination
Nail trephination is the process of making a hole in a nail to drain a subungual hematoma. Nail trephination is most likely to be successful if performed within 48 hours of injury.
Indications3
- Painful/symptomatic
- Large hematoma involving more than 50% of the nail
Contraindications (for electrocautery trephination)
- Acrylic nails (flammable!)
Complications
- Secondary infection of the nail bed and deeper structures
- Pain caused by pressure against or contact with the nail bed during the procedure
- Potential for clotting to plug the nail hole, leading to reaccumulation of blood
Procedure
The most common methods of trephination are with electrocautery or using a needle to bore through the nail.
Steps for electrocautery trephination:
- Remember to wear eye protection, a procedure mask, and gloves, as sometimes the blood may spurt from the nail under high pressure.
- In selected patients, perform a digital block or sedation. This step is often not required, as performing the nerve block is often more painful than the trephination itself.
- Clean the nail with povidone iodine swabs using sterile technique. Isopropyl alcohol is highly flammable and should be avoided if electrocautery is used.
- Puncture the nail with an electrocautery device. Press the device against the nail in the center of the hematoma while avoiding the lunula and its associated nail matrix. Avoid contact with nail bed. The hole should be large enough (3 to 4 mm) for continued drainage, which may occur for 24 to 36 hours after injury.
Steps for needle trephination:
- Remember to wear eye protection, a procedure mask, and gloves, as sometimes the blood may spurt from the nail under high pressure.
- In selected patients, perform a digital block or sedation. This step is often not required, as performing the nerve block is often more painful than the trephination itself.
- Select a large gauge needle (e.g., 18 gauge) for trephination.
- Use a twirling motion with gentle downwards pressure to create a hole in the nail until blood begins to drain. Again, be careful to avoid the lunula so as to not damage the underlying nail matrix. Usually one hole created with a larger gauge needle is sufficient, but multiple holes may be required if you choose to use a smaller gauge needle.
What about using a heated paper clip?
The classic technique of using a heated paper clip is probably best reserved for situations where there are no other alternatives available. Nowadays, most paper clips are made of metals like aluminum that are very difficult to heat sufficiently to melt through a nail.4 Furthermore, the rapid cooling of the paperclip means that excess pressure may need to be applied to melt the nail, causing excess pain for the patient and the potential for injury to the underlying nail bed due to sudden penetration of the nail with excess force.
[bg_faq_end][bg_faq_start]6. Does the fingernail need to be removed to rule-out a nail bed laceration?
Nail removal was traditionally recommended for hematomas that involved more than 25 to 50 percent of the nail or if a fracture was found on radiographs, as these features were associated with nail bed lacerations longer than 2 to 3 mm. It was thought that these nail bed lacerations should be repaired to prevent long-term nail deformity.
However, more recent evidence supports the use of trephination in patients with intact nail folds even when large hematomas or non-displaced underlying fractures are present. Nail removal and laceration repair is not required for these patients with intact nail folds as it has not been shown to result in improved short- or long-term outcomes such as reduced rates of infection or nail deformity.5,6
That being said, nail removal should be performed when a nail laceration threatens the preservation of the nail or digit. For example, patients with nail fold injuries, broken nails, or clear fingertip or toe avulsion injuries should have the nail removed to facilitate proper repair of the underlying nail bed.
[bg_faq_end][bg_faq_start]7. If the patient has an associated distal phalanx fracture, what is the management?
Even though a subungual hematoma with an underlying fracture can technically be considered an open fracture, patients with intact nail folds do not routinely require prophylactic antibiotics after trephination.6
Nondisplaced distal phalanx fractures should be splinted with the DIP joint in extension for three to four weeks.
Consultation with a hand surgeon should be considered for patients with displaced or intraarticular distal phalanx fractures.
[bg_faq_end][bg_faq_start]8. What would your discharge instructions be?
The digit should be kept clean and dry to lower the risk of bacterial infection. Patients should return to care if there is reaccumulation of the hematoma with pain or if any signs of infection develop (e.g., warmth, redness, or fever).
[bg_faq_end]Case Conclusion:
After a detailed discussion with your preceptor, you apply what you have learned to John’s case. He has an acute, painful, non-draining subungual hematoma with intact nail folds, making him a good candidate for trephination. Given the size of his hematoma (involving >50% of the nail), you appropriately obtain radiographs of the affected finger, which do reveal a non-displaced extraarticular fracture of the distal phalanx of the left second finger. After obtaining informed consent, you use an electrocautery to trephinate his nail, being careful to avoid the lunula, which results in drainage of the trapped blood. You then provide John with a splint to keep his finger in extension for 3 to 4 weeks to allow his fracture to heal. You encourage him to keep his finger dry and clean over the next couple of days and to return to care if he is at all concerned about reaccumulation of blood or infection. He thanks you for your care and states that his pain is already greatly improved.
This post was edited by Daniel Ting and copyedited by @jamievanderende.
- 1.Simon RR, Wolgin M. Subungual hematoma: Association with occult laceration requiring repair. The American Journal of Emergency Medicine. Published online July 1987:302-304. doi:10.1016/0735-6757(87)90356-1
- 2.Fastle RK, Bothner J. Subungual Hematoma. UpToDate. Published 2018. Accessed July 16, 2020. https://www.uptodate.com/contents/subungual-hematoma
- 3.Mailot T, Lyn E. Fingertip Injuries. In: Rosens Emergency Medicine. Saunders; 2014:561-562.
- 4.Antevy P, Saladino R. Management of finger injuries. In: Textbook of Pediatric Emergency Procedures . 2nd ed. Lippincott Williams & Wilkins ; 2008:929.
- 5.Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. The Journal of Hand Surgery. Published online November 1999:1166-1170. doi:10.1053/jhsu.1999.1166
- 6.Seaberg DC, Angelos WJ, Paris PM. Treatment of subungual hematomas with nail trephination: A prospective study. The American Journal of Emergency Medicine. Published online May 1991:209-210. doi:10.1016/0735-6757(91)90077-w
Reviewing with Staff
Fabulous summary of subungual hematomas. This is a very common and particularly painful condition. Nail plate trephination is so fast and satisfying to provide instant pain relief without analgesia.
Please do not forget to have a very low threshold to x-ray. I have had 2 recent distal phalanx open fractures fully hidden underneath the subungual hematomas. These were more involved and can require nail plate removal, extensive washout, nailbed laceration repair, antibiotics, and plastics consults for hand clinic follow-up. In 2020 in Calgary, I\'ve had plastics surgeons expect open washout and repair prior to hand clinic follow-up. Local practice may vary.



