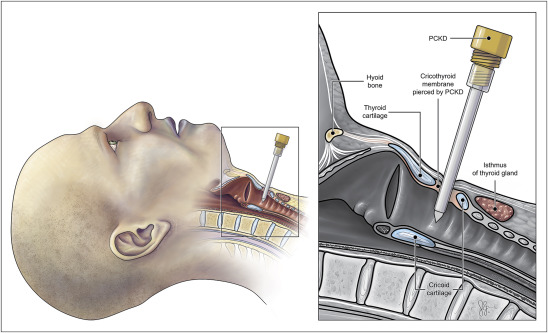
“Can’t Intubate, Can’t Ventilate” – a fearsome phrase for all airway providers that necessitates an equally fright-inducing procedure. Cricothyrotomy is an emergency procedure where an incision is made through the cricothyroid membrane and a tube is inserted for ventilation. Although there are percutaneous techniques, this article will discuss surgical techniques which have been shown to produce more favourable success, complication rates of the procedure, as well as address some common fears associated with teaching cricothyrotomy.1 The procedure is typically performed after endotracheal intubation has failed in cannot intubate, cannot oxygenate scenarios, such as: oral/ maxillofacial/ cervical spine trauma, profuse oral haemorrhage, copious emesis; or anatomical abnormalities preventing endotracheal intubation.2 When indicated, this procedure can be lifesaving, but statistics reveal some concerning findings.
In reality, cricothyrotomy success rates vary considerably depending on operator and location. A 10-year retrospective study in Korea found that success rates were as high as 82.4% in one centre and as low as 50% in another.3 Additionally, the success rate of emergency physicians, the group most likely to perform the procedure, was 68.4%.3 An important confounder inherent to this procedure and impacting both operator and location is that, by nature, cricothyrotomy is a high acuity, low-occurrence procedure (a “HALO” procedure). This means that the procedure is rare and stressful, which in turn affects success of those who perform it as well as presents a challenge when considering training providers to perform it: as resources for education are limited, should more common procedures be prioritised? How often should the procedure be taught?
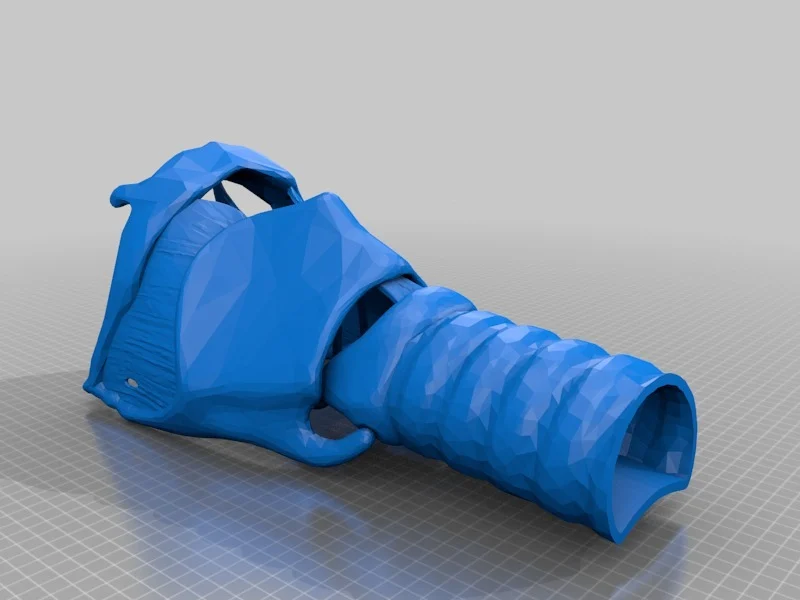
Similar to other procedures and scenarios in medicine, cricothyrotomy training is delivered sequentially with increasing difficulty. The “Sim Zone” framework of Roussin and Weinstock is an excellent model of this delivery where students and practitioners at various stages in training are initially taught with basic skills practice, then move on to applying skills in controlled environments; then in various scenarios; and then finally in complex life-like scenarios in multi-disciplinary teams.4 Skills training typically involves showing students educational instructional materials, like videos,5 then practising with various models, which were historically animal models or human cadavers,5 but have recently moved to 3-D printed models.6,7 Some centres and curricula may then move on to using mannequins in a realistic scenario, but it is unclear how often centres incorporate cricothyrotomy scenarios in multi-disciplinary mock codes.
Challenges in Teaching Cricothyrotomy
One of the issues with cricothyrotomy skill training with non-human models (like mannequins), which can generally be said about any training with models, is the lack of tactile fidelity. Although anything short of a real experience with a human can be criticized as having a “different feel,” current technology has come reasonably close. While past curricula used expensive mannequins or animal models, which are single use and difficult to store, current 3-D printed models have been found to be non-inferior with respect to handling.8 Although these 3-D printed models may have a larger up-front cost, they can generally be used multiple times unlike single-use animal models. Conversely, 3D-printed models lack realism, like the absence of neck hematoma complications, using non-obese models, and having variable tactile fidelity. Fortunately, modifications can be made such as adding red-dyed saline in tubing to simulate bleeding complications, or using hybrid 3-D printed-animal models like incorporating pork belly fat on 3-D printed tracheas to improve tactile fidelity and even simulate obesity.6
Another consideration of training, typically impacted by limited resources, is the decision of simulation frequency. One study found that the number of times needed to practice cricothyrotomy before consistently being able to successfully insufflate lungs in 40 seconds or less, is four attempts.9 Beyond that, curriculum makers need to consider skill degradation after simulation, as multiple studies have found significant skill degradation as little as 3 months after training, but typically at 12 months after.10 Does this then necessitate cricothyrotomy skills refresher simulation training to faculty and trainees every year? Given the low incidence of the procedure and the limited time, education, and simulation resources in an already strained healthcare system, this may not be a reasonable expectation for the majority of centres.
Teaching Cricothyrotomy in Special Populations
As discussed above, cricothyrotomy is a high acuity, low-occurrence procedure, but it is even more rare in the world of pediatrics. A study looking at procedures in pediatric presentations to emergency departments across 9 hospitals in the US over 5 years found that cricothyrotomy was never performed.11 The low incidence is not the only unique nuance in this population: tracheal anatomy changes across the lifespan, requiring more thought and resources to find realistic models for different sizes and ages of life. Some training programs use 3-D models of scaled down adult tracheae, however this lacks fidelity due to many differences beyond size, that exist for the pediatric airway (eg a more anterior and softer thyroid cartilage, a larger and more elastic cricoid cartilage etc).12 When clinicians are designing pediatric residency curricula or deciding when (or even if) to employ skills refresher courses, it will be difficult to justify spending healthcare dollars on multiple different models to practice an extremely rare procedure, especially when compared to more common procedures like dislocation reduction or lumbar punctures.
Teaching cricothyrotomy in rural communities may be even more challenging due to limited resources and staff, as well as other competing priorities. Though we would hope staff in rural settings would have access to refresher simulations and high-fidelity models for skills training, the reality is that most rural centres, even in Canada, are not afforded protected time or funding resources to ensure this occurs. Some emerging 3-D printing technology can allow for a more affordable, customizable solution, but may still be cost-prohibitive in certain centres.13 Lack of protected time and staff shortages also present barriers in rural settings, necessitating prioritization of procedures and skills to invest practise time in.14 Should these centers prioritize simulation training for high acuity, low-occurrence events, such as cricothyrotomy, or more frequent skills used such as quality CPR? Though virtual sessions may provide a supplement to traditional simulation education, there continues to be an “access gap” in rural healthcare provider training including for high acuity, low-occurrence procedures like cricothyrotomy.15
Final Thoughts
Cricothyrotomy is a critical procedure in cannot intubate, cannot oxygenate situations and has proven to be very difficult to teach as well as maintain competency in, because of its high acuity, low-occurrence nature. Although 3D printed models have helped reduce cost, the lack of tactile fidelity necessitates hybrid models which may be cost-prohibitive in some centres. Furthermore, special populations like pediatrics and rural communities require more tailored solutions due to changing anatomy and resource constraints, which adds a layer of complexity to its effective instruction. The ongoing struggle for educators and healthcare systems to find a balance between practicality and ideal healthcare delivery is magnified for this life-saving skill.
This post was copyedited by George Gainham and was edited by Daniel Ting.
References
- 1.Heymans F, Feigl G, Graber S, Courvoisier D, Weber K, Dulguerov P. Emergency Cricothyrotomy Performed by Surgical Airway-naive Medical Personnel: A Randomized Crossover Study in Cadavers Comparing Three Commonly Used Techniques. Anesthesiology. 2016;125(2):295-303. doi:10.1097/ALN.0000000000001196
- 2.McKenna P, Desai N, Tariq A, Morley E. statpearls. Published online February 4, 2023. http://www.ncbi.nlm.nih.gov/books/NBK537350/
- 3.Kwon Y, Lee C, Park S, Ha S, Sim Y, Baek M. Incidence and outcomes of cricothyrotomy in the “cannot intubate, cannot oxygenate” situation. Medicine (Baltimore). 2019;98(42):e17713. doi:10.1097/MD.0000000000017713
- 4.Roussin C, Weinstock P. SimZones: An Organizational Innovation for Simulation Programs and Centers. Acad Med. 2017;92(8):1114-1120. doi:10.1097/ACM.0000000000001746
- 5.Biron V, Harris M, Kurien G, et al. Teaching cricothyrotomy: a multisensory surgical education approach for final-year medical students. J Surg Educ. 2013;70(2):248-253. doi:10.1016/j.jsurg.2012.11.004
- 6.Kei J, Mebust D, Duggan L. The REAL CRIC Trainer: Instructions for Building an Inexpensive, Realistic Cricothyrotomy Simulator With Skin and Tissue, Bleeding, and Flash of Air. J Emerg Med. 2019;56(4):426-430. doi:10.1016/j.jemermed.2018.12.023
- 7.Yeggi W. Cricothyrotomy. 3-D printed model search. Accessed September 24, 2024. https://www.yeggi.com/q/cricothyrotomy/
- 8.Huang J, Licatino L, Ocariz S, Warner P, Sims C. A Novel Approach to Emergency Airway Simulation Using a 3D-printed Cricothyrotomy Task Trainer. J Educ Perioper Med. 2021;23(3):E670. doi:10.46374/volxxiii_issue3_sims
- 9.Wong DT, Prabhu AJ, Coloma M, Imasogie N, Chung FF. What Is the Minimum Training Required for Successful Cricothyroidotomy? Anesthesiology. Published online February 1, 2003:349-353. doi:10.1097/00000542-200302000-00013
- 10.Legoux C, Gerein R, Boutis K, Barrowman N, Plint A. Retention of Critical Procedural Skills After Simulation Training: A Systematic Review. AEM Educ Train. 2020;5(3):e10536. doi:10.1002/aet2.10536
- 11.Shappell E, Dutta S, Sakaria S, McEvoy D, Egan D. Variability in Emergency Department Procedure Rates and Distributions in a Regional Health System: A Cross-Sectional Observational Study. Ann Emerg Med. 2023;81(5):624-629. doi:10.1016/j.annemergmed.2022.12.016
- 12.Hampton, Z; Davis, A; Kalnow, D. Innovations in Airway Education: 3D Printed Neonatal and Pediatric Needle Cricothyrotomy Trainers. Journal of Education and Teaching Emergency Medicine. Published online 2020. doi:10.21980/J8R928
- 13.Siraj S, Sivanathan M, Abdo S, et al. Hands-On Practice on Sustainable Simulators in the Context of Training for Rural and Remote Practice Through a Fundamental Skills Workshop. Cureus. 2022;14(9):e28840. doi:10.7759/cureus.28840
- 14.Orrantia E, N. Orrantia M, Patchett-Marble R. The Occasional rural sim. Can J Rural Med. Published online 2023:136. doi:10.4103/cjrm.cjrm_73_22
- 15.Siraj S, Brunton G, Arutiunian A, Brock G, Dubrowski A. Developing a Partnership Model to Address Gaps in Rural Healthcare Provider Training Using Simulation-Based Health Professions Education. Cureus. Published online March 28, 2023. doi:10.7759/cureus.36789
- Title Image: href=”http://www.freepik.com”>Designed by Macrovector_Official / Freepik
Reviewing With The Staff
This article highlights the clinical importance of cricothyrotomy in life-threatening cannot intubate, cannot ventilate situations, where traditional airway management methods fail. Although cricothyrotomy can be life-saving, its effectiveness depends significantly on the provider\'s experience, the clinical setting, and the availability of proper training. Given its classification as a high acuity, low occurrence procedure, maintaining proficiency in performing cricothyrotomy is challenging. Training strategies, including the use of simulation models and 3D-printed anatomical replicas, have improved access to practice. However, limitations in fidelity and resource availability remain, particularly in pediatric and rural care settings. This underscores the need for targeted, regular training in diverse clinical environments to reduce complication rates, improve overall success, and align teaching practices with those of competence-based education.



