Venus is a 29-year-old female who presents to the ED with tremor and diaphoresis. You learn that she has presented to the ED with similar symptoms before, and has a 5yr history OUD, using about 5 points (0.5 g) a day. She has no other medical conditions and blood work is within normal limits. Venus is tachycardic at 105 bpm, with dilated pupils, piloerection, slight tremors, and flushed face. You remember a previous CanadiEM article on application of the COWS Scale in the ED, and note that Venus’s COWS score is 13.
In the opioid epidemic, emergency departments play a crucial role in managing opioid use disorder (OUD), overdose, injection-related infections, and withdrawal. Due to limited primary care access, Emergency physicians are increasingly managing OUD cases.
Opioid Agonist Therapy (OAT) is the chief treatment modality, and includes Buprenorphine/naloxone (buprenorphine/naloxone) and methadone. Buprenorphine/naloxone is often favored due to lower overdose risk, fewer drug interactions, and no QT prolongation concerns.
ED-initiated buprenorphine and a brief negotiation interview resulted in twice as many patients in OUD treatment at 30 days.1 Patients treated with Buprenorphine/naloxone require maintenance therapy upon induction. Withdrawal management alone and tapering is not recommended; these strategies are associated with high rates of relapse, increased risk of fatal and non-fatal overdoses, and increased rates of infections such as HIV and Hepatitis C.2
CanadiEM has previously discussed identifying opioid poisoning, obstacles to OAT initiation in the ED, Buprenorphine/naloxone initiation as QI, and the COWS Scale. This article provides an overview of front-line OAT treatments, initiation methods, and briefly covers other therapies with Addiction Medicine specialist support.
Buprenorphine/naloxone Treatment
Buprenorphine/naloxone induction traditionally required waiting for moderate opiate withdrawal before beginning Buprenorphine/naloxone, to avoid inadvertently precipitating more severe withdrawal. Buprenorphine is a partial opioid-agonist which can displace full-agonists (like fentanyl) from opioid receptors, which leads to a rapid reduction in opioid effects, causing severe withdrawal. This has been a barrier to buprenorphine/naloxone induction in the ED. However, a few mitigation strategies have emerged:
- Microdosing (lower doses of buprenorphine/naloxone than the standard dose) has emerged as a method to avoid withdrawal entirely.
- Macrodosing (higher doses of buprenorphine/naloxone than the standard dose) has evolved as a method of induction for people who are not likely to follow up with healthcare providers because it allows for very rapid initiation, rather than having the patient return over several days
- Home induction is also another option, especially for those that have already passed the withdrawal period. An approach to choosing an induction method is reviewed by this excellent Ottawa EM article.
Regular Induction
Regular induction of Buprenorphine/naloxone using a COWS scale has been described on CanadiEM before. Because Buprenorphine/naloxone is a partial agonist, it risks pushing a person into withdrawal by kicking off other molecules of opiates (fentanyl, heroin, etc.) Thus, we wait until a person scores ≥12 on the COWS scale (moderate withdrawal). It is important to also consider the timing of the last used opioid and the specific opioid used prior to initiating Buprenorphine/naloxone therapy.
Before Starting
- Insure the person meets criteria for OUD, and that informed consent has been obtained
- Liver function panel (involve an addictions specialist if 3 to 5 times normal upper level)
- Consider STI/Hep C/HIV Screen
- Ensure no opioids have been used 12 to 24 hrs prior to induction
Starting
Regular Induction of Buprenorphine/naloxone

* If the person is not scoring on the COWS scale, delay induction until they reach withdrawal.2 If it is because they are taking short or intermediate acting opioids, you can initiate or consider microdosing, or home start; see this excellent Ottawa EM article.
Click here for the MD CALC COWS Scale.
Click here for a useful decision support tool from LOUD in the ED.
After Induction
- Ensure follow up (at an OAT clinic, with their Family Doctor, etc.)
- Provide Narcan/Naloxone Kit and teaching (in case of relapse)
Microdosing
Microdosing begins with very small doses to avoid precipitating withdrawal. Thus, inducing withdrawal prior to administering Buprenorphine/naloxone is not needed.3 This more recent approach is gaining more popularity as increasing research supports its use.4,5
Before Starting
- Insure the person meets criteria for OUD, and that informed consent has been obtained
- Liver function panel (considers risks and benefits if 3 to 5 times normal upper level)
- Consider STI/Hep C/HIV Screen
Starting
Microdosing induction of Buprenorphine/naloxone
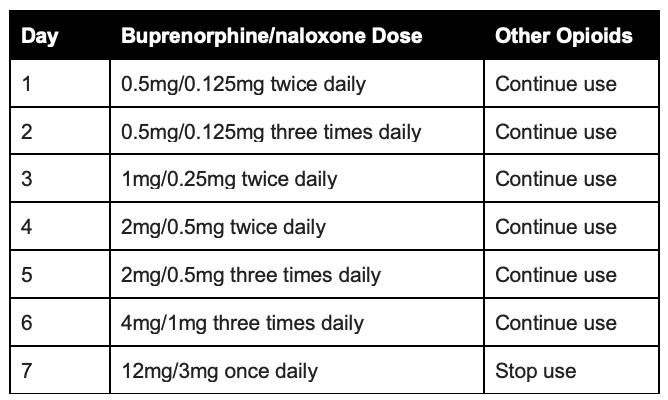
After Induction
- Ensure follow up (at an OAT clinic, with their Family Doctor, etc.)
- Provide Narcan/Naloxone Kit and teaching (in case of relapse)
Macrodosing
Macrodosing can be done in cases where any delays in treatment could pose a risk, and when a person has a high tolerance for opioids. A dose of ≥12 mg of Buprenorphine/naloxone is given to start, once a person reaches a COWS ≥13.7
Before Starting
- Insure they meet criteria for OUD, and they have a known high tolerance of opioids
- Informed consent
- Liver function panel (ALT/AST)
- Consider STI/Hep C/HIV Screen
Macrodosing induction of Buprenorphine/naloxone
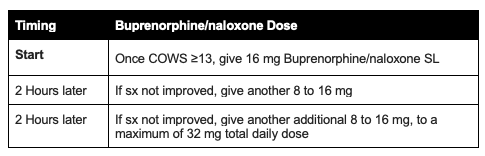
Click here for a useful infographic from META:PHI.
After Starting
- (Attempt) to arrange follow up (at an OAT clinic, with their Family Doctor, etc.)
- Provide Narcan/Naloxone Kit and teaching (in case of relapse)
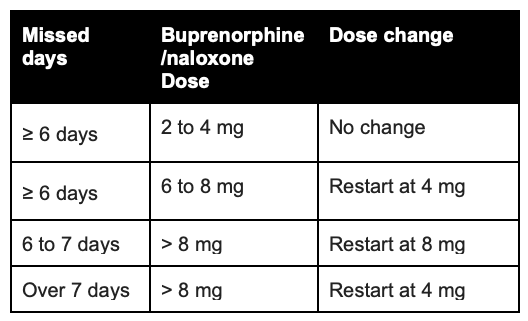
Missed doses, and restarting Buprenorphine/naloxone
Some patients may present because they have missed a dose. It is recommended that you ensure that they have not been using any other opiates save for their Buprenorphine/naloxone dose.
Approach to missed doses of Buprenorphine/naloxone
Methadone
Methadone is equally (at times, more) effective as Buprenorphine/naloxone, however, it has a higher overdose risk, and leads to QT prolongation. Furthermore, methadone is trickier to start in the ED, given its long half-life and long monitoring period required. It is recommended to consult the Addictions Medicine team and/or consider a Buprenorphine/naloxone induction instead. However, In some circumstances, a methadone induction may be performed in the ED.
N.B., In some jurisdictions (e.g., British Columbia), healthcare providers are required to take a specific course before being allowed to prescribe methadone.
Regular Induction
Before Starting
- Insure they meet criteria for OUD
- Consider medication interactions, through CYP3A4 (Antiretrovirals, antibiotics, anticonvulsants, etc.)
- Consider QTc prolongation, especially once doses reach 100 mg. Consider ECG especially in those with a history of syncope, arrhythmia, structural heart issues, prolonged QTc, etc.
Regular induction of Methadone

Click here for a useful infographic from META:PHI.
After Starting
- Ensure follow up (at an OAT clinic, with their Family Doctor, etc.)
- Provide Narcan/Naloxone Kit and teaching (in case of relapse)
Missed doses, and restarting Methadone

Additional Notes
Symptomatic management of withdrawal
In addition to OAT, or if you have maximized OAT therapy, and the person continues to feel withdrawal, they can be addressed symptomatically with
- Acetaminophen, Ibuprofen
- Loperamide, Ondansetron, Dimenhydrinate
- Clonidine
Managing pain in the context of OAT treatment
If there is acute pain, it is important to consult the addictions medicine team. Broadly speaking, OAT is continued, and pain management is optimized with non-opioid strategies first, and then opioids are added as needed. An excellent UpToDate article summarizes the approach.
Follow-Up
It is important to bridge Buprenorphine/naloxone initiation in the ED with timely referral to appropriate community outpatient addictions programs for follow-up. Buprenorphine/naloxone induction with rapid referral to an outpatient community-based addictions clinic led to a 6-month treatment retention rate of 37%, as well as a reduction in ED visits compared to control at 3 and 6 months.8 A list of rapid access addiction medicine clinics in Canada can be found here.
Tapering
Once a patient reaches a therapeutic dose of OAT, that dose is generally continued indefinitely. Tapering is not recommended. In clinical trials, the majority of people that taper from Methadone or Buprenorphine/naloxone relapse (89.2% within 6 months of a Methadone taper; and 91.4% within 8 weeks of a Buprenorphine/naloxone taper).2 Withdrawal management alone is associated with increased risk of overdose and infection. If a patient prefers to taper, we recommend doing so in consultation with an addictions physician.
Psychosocial Treatments
Psychosocial treatments alone have similar risks to tapering/withdrawal management alone. There is mixed evidence regarding augmentation of pharmacological treatment with psychosocial treatment. An older Cochrane review found no evidence that adding psychosocial modalities helped.9 A more updated meta analysis found that contingency management (using positive reinforcement to encourage/reward desirable behaviors) may improve treatment retention, but there was no other evidence of an effect of psychosocial treatments.10 Patients should never be required to undergo psychosocial treatment to remain on pharmacological treatment.
Case Summary
With a COWS score of 13, Venus meets the criteria for ED initiation of Buprenorphine/naloxone. Venus is counseled on the use of Buprenorphine/naloxone for OUD and she provides informed consent to treatment. You order a liver function panel and offer STI screening. Since she is already in withdrawal, and is willing to remain in the ED, you start with 4mg of Buprenorphine/naloxone. A referral is sent to an OAT clinic for follow-up after discharge from the ED.
This post was copy-edited by @aafia-maqsood.
References
- 1.D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency Department–Initiated Buprenorphine/Naloxone Treatment for Opioid Dependence. JAMA. Published online April 28, 2015:1636. doi:10.1001/jama.2015.3474
- 2.British Columbia Centre on Substance Use. A guideline for the clinical management of opioid use disorder. . BCCSU. Published online February 8, 2017:77.
- 3.Randhawa PA, Brar R, Nolan S. Buprenorphine–naloxone “microdosing”: an alternative induction approach for the treatment of opioid use disorder in the wake of North America’s increasingly potent illicit drug market. CMAJ. Published online January 19, 2020:E73-E73. doi:10.1503/cmaj.74018
- 4.Ahmed S, Bhivandkar S, Lonergan BB, Suzuki J. Microinduction of Buprenorphine/Naloxone: A Review of the Literature. American J Addict. Published online December 30, 2020:305-315. doi:10.1111/ajad.13135
- 5.Button D, Hartley J, Robbins J, Levander XA, Smith NJ, Englander H. Low-dose Buprenorphine Initiation in Hospitalized Adults With Opioid Use Disorder: A Retrospective Cohort Analysis. Journal of Addiction Medicine. Published online May 17, 2021:e105-e111. doi:10.1097/adm.0000000000000864
- 6.British Columbia Centre on Substance Use. . Opioid use disorder practice update. . BCCSU. Published online January 2022:33. https://www.bccsu.ca/wp-content/uploads/2022/02/Opioid-Use-Disorder-Practice-Update-February-2022.pdf
- 7.Herring AA, Vosooghi AA, Luftig J, et al. High-Dose Buprenorphine Induction in the Emergency Department for Treatment of Opioid Use Disorder. JAMA Netw Open. Published online July 15, 2021:e2117128. doi:10.1001/jamanetworkopen.2021.17128
- 8.Hu T, Snider-Adler M, Nijmeh L, Pyle A. Buprenorphine/naloxone induction in a Canadian emergency department with rapid access to community-based addictions providers. CJEM. Published online April 22, 2019:492-498. doi:10.1017/cem.2019.24
- 9.Amato L, Minozzi S, Davoli M, Vecchi S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database of Systematic Reviews. Published online October 5, 2011. doi:10.1002/14651858.cd004147.pub4
- 10.Rice D, Corace K, Wolfe D, et al. Evaluating comparative effectiveness of psychosocial interventions adjunctive to opioid agonist therapy for opioid use disorder: A systematic review with network meta-analyses. Mathes T, ed. PLoS ONE. Published online December 28, 2020:e0244401. doi:10.1371/journal.pone.0244401
Reviewing with the staff
As the opioid epidemic continues to evolve, the role of emergency providers has become increasingly pressing; it is crucial to support emergency providers with the necessary knowledge and tools to effectively help people with opioid-use disorders (OUD). Despite the growing number of management options available, primary care physicians report feeling unprepared, and uncertain how to effectively treat and manage addictions. This article aims to lay out options for emergency providers to address opioid-use disorders, with the aim to help facilitate immediate intervention and prevention, reduce stigma, and connect people to comprehensive care.
The emergency department serves as a primary entry point for individuals experiencing opioid- related crises, including overdose, withdrawal, and the initiation of treatment for OUD. For many people struggling with OUD the ER represents the first, and often the last point of contact with the healthcare system. It is important that clinicians know how to provide emergency supply for Methadone/suboxone if clinics are closed, or use Macrodosing to induce suboxone when there is a low chance that patient will be able to follow up on a consistent basis. There is strong evidence for the use of suboxone in the ED, with positive effects seen on OUD management long-term.
The emergency department provides a crucial opportunity to address the stigma associated with substance use disorders. Emergency providers play a pivotal role in establishing a pattern of judgment-free and compassionate care. By fostering an atmosphere of empathy and understanding, we can increase the likelihood of continued patient engagement with the healthcare system and ensure they receive the necessary care and support they need.
The emergency department serves as the front door of our healthcare system. Therefore, it is vital to initiate OUD treatment in this setting and subsequently connect patients to other specialists as needed to address intersecting issues. This comprehensive approach promotes continuity of care and maximizes the chances of successful treatment outcomes. By equipping emergency providers with the necessary knowledge and resources, we can significantly enhance our ability to care for patients with OUD.