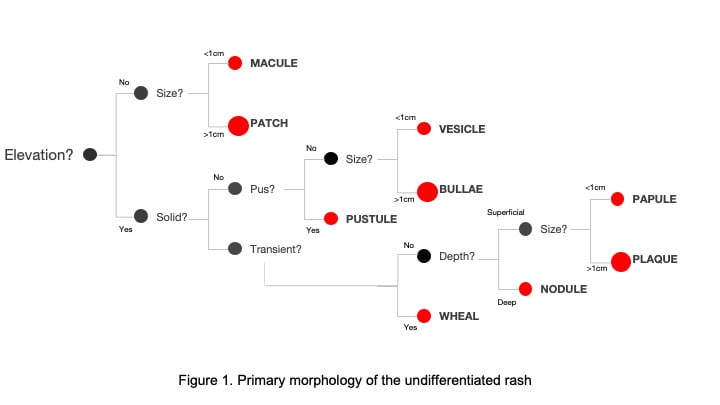
When describing a rash there are many characteristics to make note of, including its primary morphology, secondary morphology, demarcation, colour, configuration, and distribution. The focus or this article will be on primary morphology.
Reasoning through the first blush
Within primary morphology you can stratify a lesion based on whether it is flat or elevated. If the lesion is flat, then it will be either a macule or patch. A macule is a flat lesion smaller than 1 cm and a patch is a flat lesion larger than 1 cm.
Elevated lesions are either solid or fluid-filled. Solid lesions can be described as either a papule, plaque, nodule, or wheal. A raised solid lesion is a papule when it is less than 1 cm and a plaque when it is a confluence of papules greater than 1 cm. A nodule is a solid lesion with a deeper cutaneous involvement. A wheal is essentially a papule or plaque that is characteristically evanescent. It is often white at the core with an erythematous base. A fluid-filled lesion would be a vesicle, bulla, or pustule. A vesicle is less than 1cm while a bulla is greater than 1cm. A pustule is similar to a vesicle where it is usually less than 1 cm but instead of simple fluid, it is filled with pus.
It is always important to examine the rash in the context of a detailed history and physical examination. However, by determining a rash’s primary characteristics, you can narrow your differential diagnoses. Here are some common examples of dermatological findings and their associated primary morphology.
- Freckles (macule)
- Seborrheic keratosis (papule)
- Psoriasis (plaque)
- Lipoma (nodule)
- Mosquito bites (wheal)
- Herpes rash (vesicles)
- Large burn blisters (bullae)
- Folliculitis (pustule)
It’s not always so easy
There are also less common examples that you do not want to miss. If you see red macules or red/purple plaques that do not blanch, you start to think about petechia or purpura. In a sicker patient, you would worry about thrombotic thrombocytopenic purpura (TTP), disseminated intravascular coagulation (DIC), meningococcemia, and other life threatening illnesses. If you see a vesiculobullous rash that is very localized, you may be concerned about necrotizing fasciitis. If you see a diffuse pustular rash and the patient has recently started a medication, you may consider acute generalized exanthematous pustulosis (AGEP). Other life threatening rashes such as Staphylococcal scalded skin syndrome (SSSS), toxic epidermal necrolysis (TENS), and Stevens-Johnson syndrome (SJS) may have bullous lesions however can present with a variety of primary morphologies.1–4
This post was copyedited and uploaded by Josiah Butt
References
Reviewing with the Staff
Determination of the primary morphology of a cutaneous lesion is critical in making a diagnosis. Correctly utilizing these specific terms will allow one to quickly access electronic resources and get to relevant content. Understanding the terminology is also important for communication in the medical record and for consultation.
As highlighted in the introduction, further description of secondary lesions (e.g. scale, ulceration), configuration, color, demarcation, and distribution will further assist in narrowing the diagnosis. The specific size is helpful as well; 1mm papules have a different differential diagnosis than 1cm papules.
I would like to highlight two tips for those learning to diagnose and describe skin lesions.
As you learn the more specific dermatologic terminology, do not be afraid to use regular English when uncertain. A flesh coloured verrucous papule in the lateral nail fold is the same as a warty raised bump next to the nail. Plain English is better than using a specific term incorrectly.
Another common pitfall is seeing only the lesion the patient has brought to your attention. A full exam is often beneficial. Take for example a rash on the hand.
• Changes in the scalp or nails may help make the diagnosis of psoriasis.
• Associated tinea pedis may suggest tinea manuum “two feet one hand syndrome”.
• Oral vesicles will help make the diagnosis of hand foot and mouth disease.
• Facial rash may clue you in to the diagnosis of gottron’s papules in dermatomyositis.
With this in mind, for any new patient with a skin concern, my practice is to have my medical assistants have the patient wear a gown.