A career in emergency medicine involves management of risk and uncertainty. We balance multiple competing priorities and make important trade-offs on a daily basis. None more so than the delicate balance between speed and safety.
You may have heard the CT scanner being spoken about in a tongue in cheek fashion as “the doughnut of death.” While there is an element of dark humour here, there is also an element of truth. So why, you may ask, do we want to take out sickest, and often most complex patients, to this unfamiliar and dangerous environment?
Well… we can’t usually fix these patients in our resus room. Many patients in this cohort have multiple injuries, or have a time critical emergency which requires urgent intervention. CT scanning is an important aid to decision making in adult trauma patients, and appropriate CT scanning has a proven mortality benefit.1 Acquisition of these images requires moving complex and unwell patients from the resuscitation room to the CT suite in a time-critical manner.
At Gold Coast University Hospital in Southport, Australia we have been exploring how to do this better through the lens of simulation. This blog post offers five tips we have found useful thus far on our journey.
Tip 1: Not all traumas are made the same.
Fast can be defined in a number of ways. The BMJ cites 15 minutes as the target time to CT for a multiply injured trauma patient.2 However, we have found “fast enough” (considering patient and context factors) to be a more sensible goal. For example, if a patient has an isolated head injury and needs urgent neurosurgical intervention, they need to be through the scanner and into the operating room very quickly. If a patient has multiple injuries and appears in shock, they often have competing priorities that may mean the scan gets slightly delayed.3 Finally, there are patient cohorts who require imaging but are stable enough to wait, we see more than trauma in our emergency, and our other patients should not suffer due to an arbitrary time cut off.
Tip 2: The importance of the decision
Like many other important pressure points in medicine, actually making this decision is hugely important to the efficiency of transfer. Communicating this decision and the rationale clearly with the team is even more important. We have found specific timeframes to be useful and explicit communication with the team in CT to be essential. The ability for the CT radiographers to observe our progress via video link is advantageous for workflow planning.
Tip 3: The pack up
This is a different scenario than when we initially receive the patient in our resus room, and therefore requires different role allocation. Explicit communication about what equipment we need to take is vital. Negotiation with porters about how we (as a medical staff) can help them to get us to our destination safely and efficiently, has been found to empower everyone to do their job better.
It is also worth noting at this point what we do not need to take, and who does not need to come. One example of unnecessary equipment is the use of sedation via infusion pumps. We have found bolus sedation can be safe, and fewer infusion lines means a reduced chance of these being caught and dislodging lifesaving IV access points.
Tip 4: The arrival
Once we arrive in the CT scanner with a sick ED patient, it is important to note that the purpose and personnel of your team has again changed. Introducing yourself to the radiographer is simple and costs minimal time, but is invaluable in opening a dialogue which breeds safety and efficiency.4 We suggest a brief summary at this stage with a minimum data set including:
- The purpose of the scan.
- The priorities in order.
- The location and number of IV access points: contrast is almost always required and can cause competing priorities if there is a massive transfusion protocol in action.
- Anticipated issues or complications.

Tip 5: Time in the scanner
This can be the most dangerous part. The monitoring must be visible and the resuscitation must continue whilst in the scanner. Crowd control has been noted to be a big issue. If we overcrowd the control room and obstruct the radiographer, it can be neither safe nor fast. We suggest nominating 2-3 key decision makers to be allowed into the control area. It may also be useful to nominate a separate 2-3 team members to continue monitoring and ongoing treatment. Plan ahead and include the radiologist, as hot reporting may aid disposition decisions. Everyone needs to know where we’re going next.
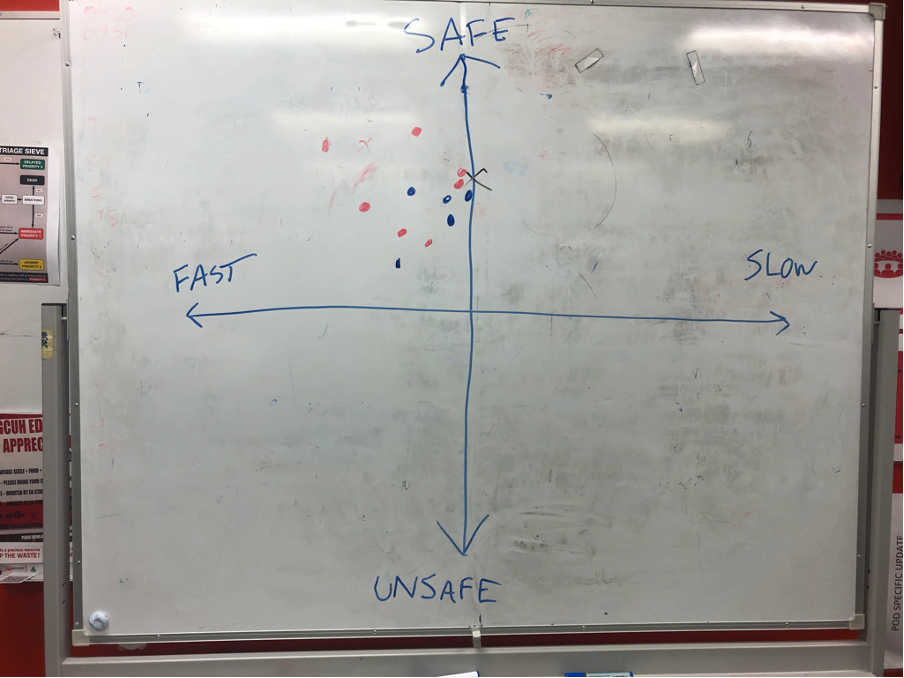
In summary, the need to move our sickest patient to a dangerous and unfamiliar environment is often unavoidable. However, there is definitely scope to make it safer. Most of that scope is related to how our teams mitigate and manage trade-offs.5 Sometimes safer is faster. Sometimes fast enough is safe. Plotting perceived speed and safety has been an interesting way to explore this complexity with our groups (Figure 1).
We continue our work in this field and hope to make 1% gains with every scenario we do. We find that our teams are already taking broader lessons about trade-offs back into their work environments.
Most of all, we have learned it’s not only the destination that matters, but also the journey.
This post was copyedited by Casey Jones and edited by Daniel Ting.
References
- 1.Hajibandeh S, Hajibandeh S. Systematic review: effect of whole-body computed tomography on mortality in trauma patients. J Inj Violence Res. 2015;7(2):64-74. doi:10.5249/jivr.v7i2.613
- 2.Mercer S, Kingston E, Jones C. The trauma call. BMJ. 2018;361:k2272. doi:10.1136/bmj.k2272
- 3.English W, West A, Durge N. Time to scan – factors that affect time to CT scan in major trauma. In: ; 2016.
- 4.Gittell JH, Seidner R, Wimbush J. A Relational Model of How High-Performance Work Systems Work. Organization Science. Published online April 2010:490-506. doi:10.1287/orsc.1090.0446
- 5.Capella J, Smith S, Philp A, et al. Teamwork Training Improves the Clinical Care of Trauma Patients. Journal of Surgical Education. Published online November 2010:439-443. doi:10.1016/j.jsurg.2010.06.006
Q&A with Dr. Chris Speirs (Author) and Dr. Daniel Ting (CanadiEM Editor-in-Chief)
DT: How does a team decide what is “fast enough”? Are there any defined goals for common conditions?
CS: I think the message here is that it’s case specific and defined goals can be helpful but are not always useful. Using trauma as an example, saying all traumas should be in CT within 15mins is unreasonable and would be at the expense of other conditions such as CVA which may take clinical priority. The time goals are often defined by the team at the time. We have found explicitly stating these to be more helpful than a rigid departmental rule or guideline.
DT: The video link idea is interesting, I do not know of any EDs in Canada that use this, but this is a neat idea. Was this something that was implemented after this work was carried out, or pre-existing?
CS: This can be a contentious issue. It was already available but had been removed due to some concerns about patient privacy. Some of the ED staff had been worried about the Radiology team viewing things they felt they shouldn’t be. However, our work has highlighted the radiographers as part of the clinical team and thus people who DO have a business in looking at what is going on in the resus room. It allows them to facilitate their scans as there are often competing priorities. We often ask them to hold the CT and promise to come immediately, when in reality we are not always ready to come immediately and this can delay other scans which are required elsewhere in the department or the hospital.
DT: Does the emergency physician go to the CT scanner for all of these patients? Or only if unstable? What if another team like trauma/ICU is already involved – does the staff emergency physician still accompany the patient? If not, how are these lessons/team culture communicated to the consulting teams?
CS: If the patient is sick enough that a physician is going with the patient, it will be an emergency physician. The Trauma and ICU team may also come but never take over care at this stage, it is considered an extension of ED care. If the patient is less sick, they would have a nursing escort but also by definition would not require urgent CT in the context of this project. Officially the hand over of care in these patients tends to happen in theatre or in the ICU.
DT: In the white board figure, it’s interesting how only 1 quadrant is used (the good one), at least in this depiction. Who gets to rate the team performance?
CS: Strangely enough, this is often the case when we do this exercise. The sim participants and the observers both the opportunity to rate the performance. Observers will become participants in the next sim, or they may already have been earlier participants so perhaps everyone is quite generous with their assessment. In general, the ratings tend to be positive or suggest things could have been quicker. I have yet to see the team’s performance be rated as unsafe.


