This episode of CRACKCast covers Rosen’s Chapter 74, COPD. This airway disease process is one of the most common causes of death worldwide. Approximately 20% of all hospital admissions for patients over age 65 are related to COPD, and so an approach to management will have nearly daily benefit for an emergency physician.
Shownotes – PDF Here
[bg_faq_start]Rosens in Perspective
Pathophysiology of COPD
According to Global Initiative for Chronic Obstructive Lung Disease (GOLD), COPD is:
“a preventable and treatable disease with some significant extra-pulmonary effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible… the airflow limitation is usually progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.”
This used to include elements of reversible airflow limitation (i.e. asthma) and chronic bronchitis (increased sputum for x 3 months for last 2 consecutive years, +/- airflow limitation)
- Don’t make the rookie mistake of mixing up COPD and emphysema:
- The latter is a destructive process. Classically centrilobular emphysema is a component of COPD. Alternatively, severe panacinar emphysema is associated with α1- antitrypsin deficiency, an enzyme that inhibits neutrophil elastase (ie stops your neutrophils from melting your lung parenchyma) (Big shout out to all my friends with this disease, you know who you are!).
Elements of COPD: Comes down to Airway obstruction and Airway obliteration
- Chronic inflammation from trachea down to alveolar.
- Neutrophils/CD8+/Macrophages/Lymphocytes
- Differs from ASTHMA which is primarily eosinophils
- Mucous plugging
- Increase in goblet cell proliferation and size, increase mucous production and plugging
- Endothelial barrier damage
- Mucociliary response inhibited
- Centrilobar emphysema
- Loss of connective tissue and subsequent airway patency/stenting through expiration via radial support (OBLITERATION)
- In the end patients end up with Type 1 & Type 2 respiratory failure (Hypoxemia <<< Hypercapnia)
- DECREASE in pulmonary vascular bed w/ chronic hypoxia = thickening of the vessel walls
- Net result = pulmonary hypertension, polycythemia: right- sided heart failure (cor pulmonale)
[1] Define acute exacerbation
According to GOLD:
“An event in the natural course of the disease characterized by a change in the patient’s baseline dyspnea, cough, and/or sputum that is beyond normal day-to-day variations, is acute in onset, and may warrant change in regular medication in a patient with underlying COPD”
- Remember viral induced tend to be protracted course.
- Common viruses include: rhinovirus, respiratory syncytial virus, coronavirus, and influenza virus
- Bacterial pathogens: controversial of acute versus chronic versus acute on chronic – think H. influenzae, M. catarrhalis, S. pneumoniae, P. aeruginosa.
[2] Describe GOLD classification for COPD
[3] List factors of decompensation or triggers of an AECOPD
[4] Name 4 mimics for AECOPD
- Pneumonia
- Congestive heart failure (CHF)
- Pneumothorax
- Pulmonary embolism (PE)
- Lobar atelectasis (plugging / mass)
- Pleural effusion
- Dysrhythmias
[5] What are the clinical features used to diagnose AECOPD?
The old school description of blue bloater (polycythemia, core pulmonale from chronic obstructive bronchitis) and pink puffer (crazy V/Q mismatch from emphysema leading to increased RR to compensate minute ventilation) have gone the way of the dodo bird. But they still have some utility for pattern recognition.
On History and Physical, look for:
History
- Cough with/without expectoration
- Increased WOB or air hunger
Physical
- Wheeze
- ALOC “Irritable Somnolence” (hypercapnea: often has asterixis with it)
- Right heart failure: JVD and peripheral edema
[6] Describe the ED management of AECOPD
Remember: Beta agonists, anticholinergics and corticosteroids are our workhorses for AECOPD.
Little or no evidence:
- Nebulized saline
- Chest physiotherapy
- Heliox
- Oral expectorants
[7] What does the end tidal tracing look like in COPD?
Remember Lipp’s top hat description for capnometry?
Well instead of Abe Lincoln, we have Jaws. Think shark tooth for airway obstruction:
[8] List indications and contraindications to NIPPV in COPD
[9] Which patients with AECOPD should be treated with antibiotics?
- Any patient who gets snorkelled: all intubated and NIPPV patients
- Increased sputum purulence with:
- Increased dyspnea, OR
- Increased sputum volume
**Note** Patients with clinical pneumonia without radiographic evidence may benefit as well
**Double Note: ** Drug selection should target local sensitivities to:
- S. pneumoniae
- H. influenzae
- M. Catarrhalis
Five days course of respiratory fluoroquinolones > 7-10 days with beta lactams and tetracycline
[10] Which patients with AECOPD require admission?
[11] List indications for intubation for AECOPD
Wise Cracks
[1] List 4 CXR and 3 ECG findings in COPD
CXR:
- Hyperinflated lungs
- Decreased vascular markings
- Small cardiac silhouette OR late stage cardiomegaly
- Increased vascular markings
- Bullae may be many or may be large, mimicking pneumothorax.
Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8512
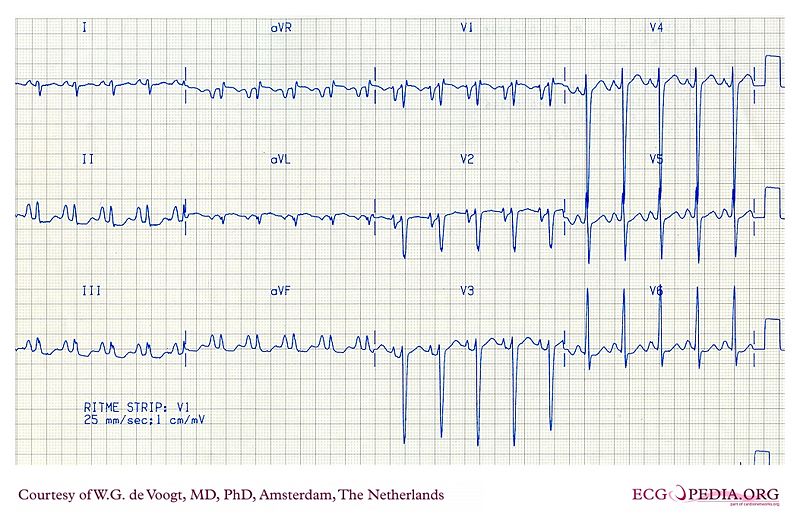
ECG:
- P pulmonale: Peaked P waves in leads II, III, and aVF
- Low QRS voltage (hyperinflated chest)
- Clockwise rotation & poor R wave progression in the precordial lead (classically described from RV hypertrophy or dilatation, but this is non specific)
- Tachydysrythmias: AFIB/Multifocal atrial tachy
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)