This episode of CRACKCast covers Chapter 57 of Rosen’s Emergency Medicine, Knee and Lower Leg. Continuing on with the orthopaedic chapters and objectives, this episode reviews the relevant approaches to knee and lower leg injuries that are actionable in the emergency department setting.
Shownotes – PDF Here
Also check out the EM Cases Rapid Review videos on Occult Knee Injuries Part 1 and Part 2
[bg_faq_start]Rosen’s in Perspective
- “Most complex joint in the body”
- Flexion, extension, rotation, gliding, rolling
- Joins the two longest levers in the body (tibia and femur)
- Main ER goals:
- Identify repairable vascular injuries
- Reducing dislocations
- Stabilizing fractures
- Giving antibiotics when needed
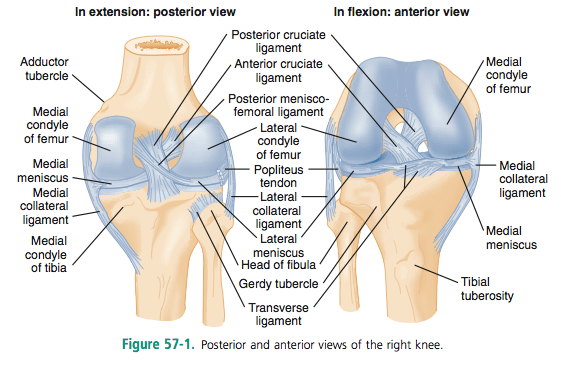
Has two joints:
- Tibio-femoral
- Femur = two condyles
- These articulate with the tibia, cushioned with the medial and lateral menisci
- Four strong ligaments anchor the tibia to the femur:
- Anterior cruciate ligament*
- Posterior medial femoral intercondylar notch → anterior surface of the tibial plateau at the notch
- Prevents anterior displacement of the tibia in relation to the femur
- Posterior cruciate ligament*
- Prevents posterior displacement of the tibia in relation to the femur
- Medial collateral ligament
- Prevents valgus deviation
- Lateral collateral ligament
- Prevents varus deviation
- * = rich blood supply
- Anterior cruciate ligament*
- Femur = two condyles
3 compartments
- Patello-femoral
- The patella slides up and down through the femoral trochlea
- Medial TBFM
- Includes the adductor tubercle and pes anerinus (goose foot)
- Lateral TBFM
- Includes the popliteus tendon
- The suprapatellar bursa communicates with the tibiofemoral joint
- The pre-patellar bursa does not communicate with the tibiofemoral joint
1) List contents of popliteal fossa
- Posterior rhomboid space:
- Laterally = biceps femoris tendon
- Medial = semimembranosus and semitendinosus tendons
- Superiorly = above muscle bellies
- Inferiorly = two heads of the gastrocnemius muscles
- Interiorly = popliteal artery + vein, peroneal and tibial nerves
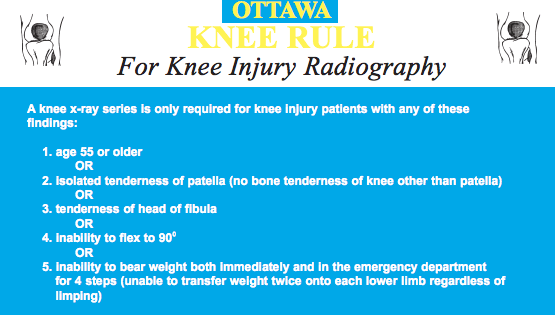
2) Describe Ottawa knee Rule
Goal of radiography = rule out a fracture!
- X-ray isn’t perfectly sensitive for finding subtle fractures
- Tips:
- Carefully trace the cortex
- Evaluate for a lipohemarthrosis
- Tips:
The OKR:
“Radiography necessary with any one of:”
- Age > 55 yrs
- Inability to transfer weight from one foot to the next four times at the time of injury AND in the ED (able to walk at least 4 steps)
- Inability to flex the knee to 90 degrees
- Isolated patellar tenderness
- Tenderness over the fibular head
- 97-100% sensitivity
According to Rosen’s, the OKR has been validated in kids (>5 yrs) with a 92-100% sensitivity depending on the study.
Pittsburgh knee rule:
X-ray if either:
- Age < 12 or > 50
- Unable to walk four full weight-bearing steps in the ED
3) Describe Schatzker classification for tibial plateaus fractures
- Normal mechanism of injury:
- Axial loading with valgus force (MVCs, falls from heights); fatigue and stress #s can occur in the elderly due to osteoporotic bones
- Most involve the lateral plateau and are INTRA-ARTICULAR
- A segond fracture = bone avulsion of the lateral tibial plateau
- Seen on the AP knee x-ray as a lateral avulsion #
- Lateral capsular ligament avulsion
- Can be associated with an ACL tear and rotatory instability
- Usually sports related injury: knee flexion, internal rotation and varus
- Seen on the AP knee x-ray as a lateral avulsion #
- Examination:
- Key to examine the distal pulses (high risk of popliteal artery injury)
- Must assess peroneal nerve function (foot dorsiflexion)
- Consider risk for co-comitant ACL/MCL injury
- Imaging:
- X-rays may show no overt displacement and isolated ˆlipohemarthrosis
- CT is the gold standard for evaluating tibial plateau #s, and should be done if operative intervention is considered (e.g. Displaced or multiple fragments)
- Patients with uncertain knee injuries should be non-weight bearing with orthopedic follow-up
- No weight bearing, and non-circumferential splint; usually 6-8 weeks
Classification system:
- Hohl (as in Rosen’s fig 57-6)
- Minimally displaced (<4mm)
- Displaced – 6 subtypes
- Schatzker classification
This system divides tibial plateau fractures into six types:
- Schatzker I: is a wedge-shaped pure cleavage fracture of the lateral tibial plateau, originally defined as having less than 4 mm of depression or displacement
- Schatzker II: split and depression of the lateral tibial plateau, type I fracture with a depressed component
- Schatzker III: pure depression of the lateral tibial plateau
- divided into two subtypes
- Schatzker IIIa: those with lateral depression
- Schatzker IIIb: those with central depression
- divided into two subtypes
- Schatzker IV: pure depression of the medial tibial plateau, without a fracture fragment
- Schatzker V: involving both tibial plateau regions
- Schatzker VI: fracture through the metadiaphysis of the tibia
=== copied from: https://radiopaedia.org/articles/schatzker-classification ===
4) Describe the Insall-Salvati ratio
Used to diagnose abnormal high/low riding patella
- Lateral knee x-ray with knee 30 deg. Flexed
- Patellar tendon length / patellar length
- Normal ratio 8 – 1.2 (0.74 – 1.5 in other sources)
- Patella Baja = < 0.8
- Patella Alta = >1.2
5) Describe the management of a knee dislocation
Big concern = popliteal artery injury! (Risk of limb loss in the future!)
- It is fixed in a fibrous tunnel tethered on the femur and tibia
- The peroneal nerve is in this tunnel as well
Five types of dislocation (described based on the position of the tibia relative to the femur) :
- Anterior (>50% of cases, with hyperextension mechanism)
- Posterior (high-velocity, knee flexion)
- Medial
- Lateral
- Rotary
History:
- Remember that many (>50%) spontaneously reduce before ED presentation
Physical exam:
- May be no effusion present due to joint capsule rupture
- May have large amount of associated soft tissue injury / edema making blunt vascular injury difficult to diagnose
- Hard signs:
- Large expanding hematoma
- Absent pulse
- Bruit or Thrill
- Pulsatile bleeding
- Limb ischemia
- Soft signs:
- Limb paresthesias
- Peroneal nerve:
- Dorsum of foot
- Foot dorsiflexion
- Posterior tibial nerve:
- Diminished plantar flexion and plantar sensation
- ****posterior tibial and dorsal pedal pulses will be normal in 5-15% of popliteal artery injuries****
- Peroneal nerve:
- Limb paresthesias
Diagnosis:
“Suspect injury to the popliteal artery injury in anyone with multiligament knee injury, high-force knee trauma, and knee dislocation regardless of spontaneous reduction!”
- Angiography – high morbidity due to need for femoral artery cannulation!
- CT angiography is preferred! (But no sensitivity reported in Rosen’s!)
- Duplex Ultrasonography – unsure of the role
- Ankle brachial index
- Ratio of systolic brachial BP / systolic ankle BP
- If > 0.9 = negative predictive value of 100% in knee dislocation
- Serial physical exams – 7% miss rate
- Pedal pulses serially
- Sens = 79%, spec = 91%, NPV = 93%
- Pedal pulses serially
- Ratio of systolic brachial BP / systolic ankle BP
Treatment:
- Reduction!
- Traction, counter-traction
- Splint in a long leg splint
- HARD signs: A disrupted artery needs to be repaired ASAP in the OR
- 90% amputation after 8 hrs of injury
- Isolated intimal tears identified on CT imaging are treated with observation vs. Anticoagulation
- ABI and or serial exams
- IF normal and ABI > 0.9
- Observe for 24 hrs,
- Splint at 15 deg. Flexion
- Pedal pulse check q 3 hrs
- At highest risk for compartment syndrome 24-48 hrs
- IF normal and ABI > 0.9
6) Describe the management and classification of patellar fracture and dislocation
[bg_faq_start]Fracture:
- Almost all of these fractures are intra-articular
- Classification
- Rim avulsion #s, transverse (70%), stellate, comminuted, longitudinal, marginal, proximal/distal poles
- Displaced or undisplaced
- If undisplaced = usually the medial and lateral retinaculum provide support to the extensor mechanism
- Treatment:
- If extensor mechanism is intact = non-operative management
- Long leg cast 4-6 weeks Or knee immobilization with non-weight bearing crutches
- ORIF for displaced/open fractures or non-intact extensor mechanism
- If extensor mechanism is intact = non-operative management
Dislocation:
- Most common in women (higher Q angle)
- Can occur due to a direct blow to the medial knee
- Causes a tear in the medial patellar retinaculum (almost always dislocates laterally)
- May cause an associated effusion if there is an osteochondral fracture
- Important to reduce these on the field or ASAP in the ER after sedation
- Smooth gentle knee extension passively
- Gentle anteriomedial assistance
- Important to get an AP, lateral and skyline view post
- Rosen’s states 3-6 weeks of knee immobilization ?!
- But this duration causes huge muscle wasting morbidity
- Patients should have good sports medicine followup
7) List 6 overuse syndromes
- Patello-femoral pain syndrome
- Iliotibial band syndrome
- Peripatellar Tendinitis
- Plica syndrome (redundant folds of synovium)
- Popliteus tendinitis
- Bursitis
8) Describe the sensory and motor function of nerves of the lower extremity
“Foot off the brakes (dorsiflexion), to the right (eversion), and on the gas (plantar flexion)!”
- Peroneal nerve
- Anterior compartment:
- Sens: first toe web space
- Motor: long toe extension
- Superficial peroneal nerve
- Lateral compartment
- Sens: dorsum of foot
- Motor: foot pronation / Eversion
- Sural nerve
- Superficial posterior compartment
- Sens: lateral foot
- Tibial nerve
- Deep posterior compartment
- Sens: plantar aspect of foot
- Motor: foot flexion, long toe flexion
9) Describe the 4 compartments of the lower leg and their contents
- Anterior
- Tibialis anterior
- Long toe extensors
- Anterior tibial artery
- Deep peroneal nerve (sensation to the first webspace of the foot)
- Lateral
- Foot everters:
- Peroneus longus and brevis
- Superficial peroneal nerve (sensation to the dorsum of the foot)
- Foot everters:
- Superficial posterior compartment
- Gastrocnemius, plantaris, soleus muscles
- Sural nerve (lateral side of the foot and distal calf)
- Deep posterior compartment
- Tibialis posterior, long toe flexor,
- Posterior Tibial and peroneal arteries
- Tibial nerve (sensation to plantar aspect of foot)
10) Describe the management of Tibial tubercle fractures and Osgood-Schlatter Disease
Tibial tubercle fractures
- # at the insertion of the patellar tendon
- Normally the tibial epiphysis and tibial tuberosity ossification centres fuse in late adolescence
- Usually occur with forced knee flexion against an activated quads.
- 3 grades according to the watson-jones classification
- I: hinged up with no displacement from the proximal base
- II: tubercle avulsed
- III: extend into the articular surface
- Xray
- Type 1: cast immobilization with knee in extension
- Type 2-3 usually need reduction, possible ORIF and immobilization
Osgood-Schlatter Disease
- “Osteochondritis of the tibial tuberosity”
- Traction apophysitis
- Usually occurs in athletic adolescents
- Painful swelling over the tibial tubercle – relieved by rest
- May be bilateral
- Pain with resisted knee extension
- Clinical dx, an x-ray may help rule out tumours or avulsions
- Usually self-limiting
- Rest, ice, analgesics, bracing
- Severe cases may be immobilized for 2-3 weeks
- Surgery not even considered an option until the epiphysis closes
11) List 4 complications of tibial shaft fractures
- Compartment syndrome (highest risk at 24-48 hrs)
- Infection – shallow easily exposed bone (look for subtle open #!)
- Nerve injury – “foot off the brake, to the right, and on the gas”
- DVT, pseudoaneurysm
- Fat embolism
- Delayed healing – average union times is 20-30 weeks
- Malrotation
- CRPS
(tenuous blood supply) = increased risk of osteomyelitis & non-union
12) Describe the management of proximal fibula fractures
- The fibula is a non-weight bearing bone that helps keep the tibial weight bearing surface in place on the plafond
- Isolated fibula #s usually occur from a direct blow
- But rare cases: Maisonneuve fracture
- Must assess peroneal nerve function (foot drop) and LCL status
- Important to get knee and ankle joint x-rays
Management:
- Symptom control
- Non-weight bearing initially
- Advance to wt. bearing as tolerated based on ortho opinion (should be pain free)
- Some non-displaced #s can be sent home on crutches in a walking boot
- No casting recommended in cases of nerve deficit due to risk of compartment syndrome and neuro / vasc. Injury
- Maisonneuve fractures need ORIF
Wisecracks
1) Describe the natural history of a Baker’s cyst
- Is a popliteal cyst – an actual herniation of the synovial membrane through the posterior capsule of the knee
- Becomes prominent with an enlarging knee effusion
- Noted in the posterior – medial popliteal fossa – maximal at full knee extension
- Soften or disappear in flexion
- Can rupture into the calf and produce a clinical picture similar to DVT
- Acute complications:
- Thrombophlebitis
- Leg ischemia
- Nerve entrapment
- Compartment syndrome
- Ddx:
- Cystic masses, lipomas, liposarcomas, popliteal artery aneurysms
- Ultrasound is the diagnostic modality of choice
- Treatment: investigate the cause of the knee effusion (degenerative, inflammatory, or reactive from joint injury)
- Intra-articular glucocorticoids
- Children with primary cysts usually don’t need treatment
- Surgery usually focused on treating the intra-articular pathology (e.g. meniscus repair)
- Huge morbidity with attempted cyst removal
- Acute complications:
2) Extensor mechanism injuries – what are they?
- Extensor mechanism:
- Quads – quad tendon – medial and lateral retinaculum (on either side of the patella) – patellar tendon – tibial tubercle
- Ruptures can occur anywhere in this complex
- Usually following vigorous contraction of a flexed knee, laceration or blow. The quadriceps tendon usually ruptures at its insertion on the patella
- The patellar tendon may also rupture at the inferior patellar border
- Risk factors:
- RA, Gout, SLE, Hyperparathyroidism, immunosuppression post organ transplant
- Steroid use, fluoroquinolones
- Signs:
- Pain, swelling, palpable defect
- Unable to extend heel off the bed
- Patella alta
- Patella baja
- Diagnosis:
- Clinical
- X-rays for patellar height
- MRI for possible incomplete tendon rupture
- Management:
- Treatment (surgery) should be done in 2-6 weeks post injury or sooner!
- Some partial tears can be treated with immobilization of the knee in full extension for 4-6 weeks
3) Differential diagnosis of of sudden onset calf pain with swelling:
- Fracture – stress/traumatic
- Compartment syndrome
- Necrotizing fasciitis
- DVT
- Thrombophlebitis
- Achilles tendon rupture
- Plantaris strain/rupture
- Gastrocnemius strain/tear/rupture (usually medial head)
- Bakers cyst rupture
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)