This episode of CRACKCast covers Rosen’s Chapter 049, General Principles to Orthopedic Injuries. This is a new section of Rosen’s to cover and this episode lays a foundation for more a more in-depth look at specific injury patterns moving forward.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
[bg_faq_start]Management principles
- Reasons for urgent orthopedic consultation:
- Long bone #s
- Open fractures
- Fractures or injuries violating joints
- Neurovascular compromise
- See Table 49-1 for a list of >40 fracture eponyms
- Principles
- Get key information from patient re: age, mechanism of injury, chief complaint, medical Hx
- Do a physical exam to predict the injury and what additional imaging is needed
- If imaging shows no #, but patient examines as clinically having a # → TREAT as a fracture
- Get adequate imaging!
- Generally obtain an X-Ray before reducing a dislocation (unless in some potential field situations)
- Assess and document neurovascular status before, during and after any reduction / immobilization
- Don’t discharge any patient who can’t safely ambulate
- Patients need good discharge instructions: things to monitor and potential complications
Fractures
Fracture nomenclature
General descriptors:
- Closed or Open
- Open if the bone can be exposed to the outside environment in ANY way: e.g. A small puncture wound even in close proximity should be assessed and considered
- Exact anatomic location:
- Bone name, left/right, and reference points:
- g. Right posterior tibial tubercle
- Long bones are divided into thirds
- Bone name, left/right, and reference points:
- Describe the direction of the fracture line
- Transverse
- Oblique
- Spiral
- Comminuted (>2 fragments)
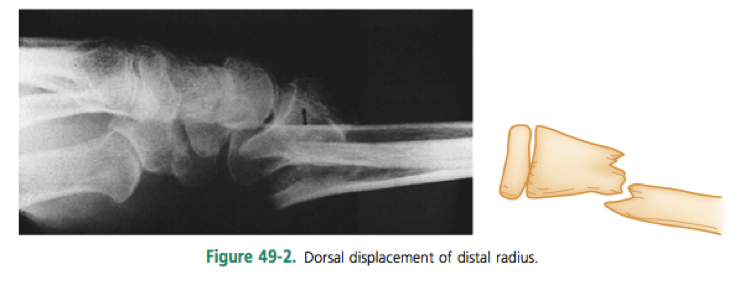
- Position and alignment of the fracture fragments:
- The amount of displacement of the distal fragment is always described first
- Valgus = angling AWAY from the midline
- Varus = angling of the part is toward the midline
- Alignment: the relationship of the long axis of one fragment to another → creating angulation. Defined by the apex
- Rotational deformity: very important in the hand
- Descriptive modifiers:
- Complete = both cortices disrupted. Incomplete = only one
- Assess articular involvement (at high risk for articular arthropathy)
- Avulsion: when a bony fragment is pulled away from its normal position due to a tendon / muscle / ligament (phalaynx or humeral head)
- Impaction: forceful collapse of a fragment into the bone – vertebral, humeral head
- Pathologic: a fracture through abnormal bone.
- Primary or metastatic cancer,
- Cysts,
- Osteogenesis imperfecta
- Scurvy
- Rickets
- Paget’s disease
- Osteoporotic bone – due to a disease (polio)
- Stress fracture: repeated low intensity forces leading to the resorption of bone: running, sports, dancing.
- Due to intrinsic and extrinsic causes: training regimen, equipment, nutrition, hormones.
- Tibia, fibula, metatarsals, navicular, cuneiform, calcaneus, femoral neck, femoral shaft.
- Fracture eponyms: used to describe fractures BEFORE radiography existed
Fracture Healing
- Process:
- Hematoma formation which bridges the fracture fragments
- Inflammation leading to granulation tissue formation
- Resorption phase – joints the fragments with a procallus
- REmineralization phase – calcium phosphate and osseous metaplasia
- Callus resorption
- Callus usually appears on radiographs around 3 weeks
- Takes 2-4 months for bone consolidation in normal adults
- Oblique fractures heal more quickly
- Healing faster in kids and slower in the elderly
- Factors affecting healing time:
- Age
- Type of bone: cancellous > cortical
- Fracture opposition
- Systemic states (hypothyroid, renal disease, illness)
- Drugs – steroids
- Exercise – helps speed healing, hypoxia slows healing
- Delayed Union: longer than usual time to unite
- Malunion: residual deformity post-union
- Nonunion : failure to unite → may lead to a pseudoarthrosis
Fractures in Children
- Properties:
- More common to have incomplete fractures
- Greenstick # – incomplete angulated fractures of long bones
- Torus # – incomplete fracture with wrinkling/buckling of the cortex ***can be VERY subtle***
- More common to have incomplete fractures
- Epiphyses – are made of cartilage and are radiolucent
- ***Don’t neglect to consider injury to the physis: as a potential fracture*** due to compression or shearing. This may require a comparison view of the other extremity – and should be described using the SALTER system.
- SALTER:
- I: a slip in the provisional calcification zone
- Dx clinically as tenderness and swelling over an epiphysis (.e.g lateral ankle)
- ***tenderness over an epiphysis = salter I fracture, NOT a sprain, because the ligaments are weaker*** (except lateral ankle – based on recent research)
- II: 75% of all epiphyseal #s.
- Very low risk of growth disruption, can be managed non-operatively
- III: involves the articular surface, germinal layer and growth plate
- At high risk for growth disturbance
- IV: through and through. Often need surgery and close follow-up
- V:
- Most commonly in the knee and ankle
- Difficult to see on radiograph
- NEED an MRI to dx in some cases to look for hemorrhage or edema
- Physical injuries most common in boys 12-15 yrs old. And girls 9-12 yr old
- Most common sites for growth arrest.
- Distal radius, phalanges, distal tibia
- Most salter I and II can be fixed with a closed reduction and follow-up for premature physeal closure: more prevalent if > 3 mm displacement post-reduction
- Growth arrest most common in the distal femur, distal and proximal tibia and distal radius.
- I: a slip in the provisional calcification zone
Diagnostic Modalities for Fracture Diagnosis
- Plain radiography
- 2-3 views are the mainstay
- Fractures best seen when x-ray is parallel to the beam
- NEVER accept one view
- Occult fractures may be missed – until bone absorbs at 7-10 days post injury
- Stress views – rarely helpful, and may make the injury worse
- Comparison views
- Helpful in pediatrics to assess growth plates and bone maturity
- Helpful to assess for congenital abnormalities that may be present bilaterally
- Help assess for fat/fluid levels
- Nutrient arteries may mislead as a fracture:
- They are fine: sharply corticated, and less radiolucent than fractures
- Pseudofractures may appear from folded clothing or bandages
- Accessory ossicles are well corticated and smoothly defined
- 2-3 views are the mainstay
- Bone scanning
- Radionuclide useful for:
- Stress #s
- Acute osteomyelitis
- Tumours
- CT
- Most accurate method of imaging bony #s, displacement, and fragmentation
- Very useful for
- Spinal imaging
- Knee
- Acetabulum
- Wrist
- Ankle
- Salter IV #s
- MRI
- Helpful for:
- Osteochondral lesions, cartilage, ligaments, meniscus, disks,
- Ultrasound
- Can very accurately dx disruptions of bony cortices:
- Long bones
- Orbital floor
- Ankle/foot
- Rib fractures
- Can very accurately dx disruptions of bony cortices:
- Helpful for:
- Radionuclide useful for:
1) List 10 complications of fractures
| Complication | Info | Key points |
| Hemorrhage | Blood loss, shock, and death! | Pelvic, femur, tib-fib |
| Vascular injury | See chapter 48! Knee – popliteal artery Femoral neck – AVN of femoral head | 10-20% of injuries may have normal palpable pulses These injuries can lead to late complications |
| Nerve injury | Neuropraxia – contusion to a nerve leading to transient paralysis and return to function in weeks – months Axonotmesis – crush injury to a nerve – slow nerve healing Neurotmesis – severing of a nerve that requires surgical repair | See table 49-4 Light touch is a good screening test, but two-point discrimination is more sensitive (especially for digital nerves). Compare the sensation bilaterally. Consider the O’Riain wrinkle test or the Ninhydrin sweat test for digital nerve injuries. |
| Compartment Syndrome | Any # or damage in an osseofascial space = can lead to CS:
1) increased compartment contents ○ Bleeding (1 or 2ndary)
○ Increased capillary filtration
○ Increased capillary pressure
2) Decreased compartment volume
3) External pressure
4) Misc:
| Sites:
Interesting causes (based on etiology): 1. Content increase
2. Dec. compartment volume
3. External pressure
|
| Osteomyelitis | Due to OPEN fractures = any communication of bone with the outside | ANCEF for prevention, add gentamicin for contaminated |
| Avascular necrosis | No blood flow, bone dies | comminuted/untreated fractures at ^ risk
|
| Complex regional pain syndrome – type 1 | “Pain syndrome that develops after a noxious event and extends beyond a single peripheral nerve and is disproportionate to the inciting event”
Etiology – unknown ● Central and peripheral sensitization after an event that is pathologic and leads to maladaptive sympathetic and brain mapping responses Provoking factors:
Diagnosis
Treatment:
| Type 1 CRPS – many different diagnostic criteria: ● Signs:
Distal-proximal gradient Type 2 – CRPS has a demonstrable peripheral nerve injury
|
| Fat embolism syndrome | Fat globules in the lung or peripheral circulation after a LONG bone fracture or major trauma ● Often subclinical ● ⅕ people with major trauma have them, but most are asymptomatic ● Signs:
| Common after Tib/fib fractures (young adults) or hip fractures in the elderly
Treatment
|
| Fracture blisters | Tense bullae from HIGH energy injuries
| High risk locations:
May precede compartment syndrome! |
| Complications of immobilization | Lead to many issues in the elderly patient:
| Fracture complications
Immobility complications
|
2) Describe the classification system for open fractures
As above:
- Recognize the emergency
- Begin irrigation (after pain control!!)
- Cefazolin (for Grade I)
- Add Gentamicin for Grade II-III
- Alternatively: broad spectrum such as Pip-Tazo.
- Advocate for early debridement and irrigation in the OR within 24 hrs
Exceptions:
- Open distal tuft fracture of the finger
- Need vigorous irrigation and debridement with adequate primary closure (assuming adequate arterial flow!).
3) Link the nerve injury expected with the following orthopedic injuries:
a) Distal radius
i) Median nerve
- Motor: OK sign
- Sensation to 1-3 fingers
b) Elbow
i) Median or Ulnar nerve
- As above
- Ulnar:
- Motor: finger abduction, squeezing a piece of paper in-between 4-5th digit
- Sensation: 4-5th digit
c) Shoulder dislocation
i) Axillary nerve
- Motor: deltoid
- Sensation: Sergeant’s patch
d) Sacral
i) Cauda equina syndrome
- Bladder and bowel symptoms
- Loss of anal wink
- Saddle anesthesia
e) Acetabular fracture
i) Sciatic nerve
- Motor: plantar flexion, knee flexion, lower leg muscles. Spares the hamstrings
- Sensory: peroneal, tibial, sural
f) Hip fracture
i) Femoral nerve
- Motor: quads weakness
- Sensation: anterior or medial thigh
g) Femoral shaft fracture
i) Sciatic
- Motor: leg weakness of the lower leg
- Same as sciatic.
h) Knee dislocation
i) Tibial or peroneal
- Peroneal
- Weak dorsiflexion and eversion
- dorsum of foot, first webspace, lateral foot.
- Tibial:
- Motor: foot muscle atrophy
- Sensation: sole of foot and distal toes.
i) Lateral tibial plateau fracture
i) Common Peroneal
- As above
4) List 10 causes of compartment syndrome
- See Box 49-3 for a huge list!
- Increased tissue pressure → increased venous pressure → impaired local circulation and hypoxia
- Pressures above diastolic BP, but below SBP
- Reduced aterio-venous gradient at the tissue level
- → histamine release to help dilate capillaries → increased capillary membrane permeability
- → leak of proteins and fluid into the surrounding tissue
- → compartment pressure keeps increasing!
- Venous blood flow impaired as capillary pressure is exceeded
- Arterial blood flow fails (pulses maintained until LATE!)
- Ischemic necrosis and cell death!
- Arterial blood flow fails (pulses maintained until LATE!)
- Venous blood flow impaired as capillary pressure is exceeded
- → compartment pressure keeps increasing!
- → leak of proteins and fluid into the surrounding tissue
- → histamine release to help dilate capillaries → increased capillary membrane permeability
| Compartment Syndrome | Any # or damage in an osseofascial space = can lead to CS: ● Closed OR open #
Pathophysiology: ● Mismatch between a closed, non-expandable space and its contents: – see Box 49-3 1) increased compartment contents ○ Bleeding (1 or 2ndary)
○ Increased capillary filtration
○ Increased capillary pressure
2) decreased compartment volume
3) external pressure
4) Miscellaneous:
| Sites: 1. Tibia
Interesting causes (based on etiology): 1. Increased Comp. Content a. BLEED: anticoagulant/coagulopathic/traumatic 2. Dec. compartment volume a. Postoperative closure of fascial defects 3. External pressure a. Comatose drug user 4. Miscellaneous: a. Interstitial infusion |
5) List 7 physical findings in compartment syndrome
- At risk locations: – see Box 49-4
- Calf
- Thigh
- Forearm
- This is a clinical diagnosis!
- “This is the hallmark diagnosis in a conscious fully alert patient who has pain that is disproportionate to the injury or physical findings”
- Subjective complaints are important indicators of compartment syndrome
- Skin colour, temperature, capillary refill, and distal pulses are all unreliable indicators (as are pallor, and loss of pulses!)
- Rate of extremity swelling peaks at the 36-48 hr mark post injury
- POOP to PxF
- Deep, burning, unrelenting, difficult to localize pain
- Increasing need for analgesics
- Pain on passive stretching of the muscle groups
- Pain with active flexion of the muscle groups
- Hypoesthesias or paresthesias in the distribution of nerves crossing the compartment
- Tenderness / tenseness of the compartment
The five P’s
- These are NOT signs of compartment syndrome, rather they are signs of acute disruption of arterial flow
6) Describe the management of compartment syndrome
- Elevating the limb may be counterproductive – because it decreases the local arterial pressure
- Normal compartment pressure is 0 mmHg
- Microcirculation is impaired when tissue pressures > 30 mmHg
- But this VARIES person to person based on their tolerance to ischemia
- “Inadequate perfusion and ischemia begin when tissue pressure in a closed compartment are within 20 mmHg of a patient’s diastolic BP
- OR Within 30 mmHg of the MAP
- When tissue pressure = or exceeds the patients DBP tissue perfusion ceases
- Microcirculation is impaired when tissue pressures > 30 mmHg
- Intra-compartmental pressures don’t measure muscle and nerve ischemia, they just identify a ripe environment where this ischemia could occur
Diagnostic tests:
- Two techniques:
- Slit-catheter
- Side-port needle
- Stryker compartmental pressure monitor:
- Make sure that it is zeroed in the plane in which the needle will be inserted
- A single measurement is not as important as serial measurements
- Doppler ultrasound is NOT useful.
- Stryker compartmental pressure monitor:
Management:
- Fasciotomy STAT
- Fasciotomy within 12 hrs
- Fasciotomy and DON’T elevate the limb (slight dependency)
- Manage rhabdomyolysis, hyperkalemia, lactic acidosis.
7) List 5 bones predisposed to AVN
- Femoral head
- Talus
- Scaphoid
- Lunate
- Capitate
Lippism: FeTal ScaPLuna?
- OR all the crescent moon-shaped bones in the hand and…
8) Describe diagnostic criteria for CRPS
| Complex regional pain syndrome – type 1 | “Pain syndrome that develops after a noxious event and extends beyond a single peripheral nerve and is disproportionate to the inciting event”
Etiology – unknown
Provoking factors:
Diagnosis:
Treatment: ● Controversial ● Multidisciplinary approach – PT, counselling, regional nerve blocks, surgical sympathectomy ● PO meds:
| Type 1 CRPS – many different diagnostic criteria: ● Signs:
Distal-proximal gradient Type 2 – CRPS has a demonstrable peripheral nerve injury |
9) List 6 complications of prolonged immobility
| Complications of immobilization | ● Lead to many issues in the elderly patient
| Fracture complications
Immobility complications
|
Wisecracks
1) Describe fat embolism syndrome and its management
| Fat embolism syndrome | Fat globules in the lung or peripheral circulation after a LONG bone fracture or major trauma
Signs:
| Common after Tib/fib fractures (young adults) OR hip fractures in the elderly
Treatment
|
2) What is the most common site of compartment syndrome?
- Anterior compartment of the lower leg
3) Are open or closed fractures at higher risk of compartment syndrome?
OPEN!
- But as many as 30% of people (based on the UK study listed in Rosen’s) only had soft tissue injuries WITHOUT fracture!
- High risk populations: men < 35, bleeding disorders, anticoagulation, MVC’s or sports injuries.
4) Please differentiate between sprain, strain and bursitis
Sprain: “Ligamentous injuries resulting from an abnormal motion of a joint”
- 1st degree – minor tearing of ligamentous fibers w/ mild hemorrhage and swelling.
- 2nd degree – partial tear of ligament with moderate hemorrhage / swelling
- 3rd degree – complete tearing of ligament
Strain: “injury to musculotendinous unit resulting from violent contraction or excessive forcible stretch”
- 1st degree – minor tearing of muscle and/or tendon fibers w/ mild hemorrhage and swelling.
- 2nd degree – partial tear of muscle and/or tendon fibers with moderate hemorrhage / swelling
- 3rd degree – complete tearing of muscle and/or tendon fibers with possible avulsion fracture
Bursitis. – bursa is mad. Usually overuse or traumatic. Supportive care.
5) Please differentiate between tendonitis and tendonosis
Tendonitis classic def: inflammatory condition characterized by pain at tendinous insertions into bone, occurring in the setting of overuse
- Now thought to be more than just overuse – load and use interact to affect cell-matrix interaction
Tendonosis – contentious name that describes more chronic conditions: eg. degenerative changes, chronic tendinopathy, or partial rupture
Common Sites for Tendinitis
- Rotator cuff of the shoulder
- Achilles tendon
- Radial aspect of the wrist (de Quervain’s tenosynovitis),
- Insertion of the hand extensors on the lateral humeral epicondyle (tennis elbow).
- Patellar tendon
- Biceps femoris, semitendinosus, and semimembranosus (hamstring syndrome);
- Posterior tibial tendon (shin splint syndrome)
- Iliotibial band;
- Common wrist extensors (medial epicondylitis) (little league pitchers and golfers)
Clinical Pearl:
- Don’t forget about calcific tendonitis common to the common shoulder, wrist, hand, neck, hip, knee, ankle, or foot
- Subluxations and dislocations …..go read the textbook!
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)