This episode of CRACKCast covers Rosen’s Chapter 045, Thoracic Trauma. This is a large topic, but these are often life-threatening presentations where effective management done quickly is essential for patient survival.
Shownotes – PDF Link
[bg_faq_start]Rosen’s in Perspective
Epidemiology
- Direct thoracic trauma leads to ¼ of all deaths from trauma
- This stuff kills!
- Usually caused by MVC’s leading to immediate death
- Myocardial wall rupture
- Thoracic aorta rupture
Death in 30 minutes – 3 hours: WE CAN FIX THESE!!!
- Tension pneumothorax
- Cardiac tamponade
- Airway obstruction
- Uncontrolled exsanguination
- Generally 75% of thoracic trauma can be managed expectantly with simple tube thoracostomy and blood
- Need a trauma system to do well post ER resuscitation
- CT’s are becoming more common, and they show things that can be missed:
Multiple structures involved:
- Airway – Tracheobronchial injury, traumatic asphyxia
- Lung – Pulmonary contusion, PTx, Hemothorax, Bronchiopleural injury
- Cardiac – Tamponade, Comotio cordis, myocardial contusion
- Chest Wall – rib #, flail chest
- Vascular – intercostal / great vessel disruption, blunt aortic dissection
- GI – esophageal perforation / disruption
Disruption of these structures can cause catastrophic consequences, since the chest wall is critical for ventilation and oxygenation. As the thorax expands outwards, the diaphragm expands down and creates negative pressure. Injuries to this region can disrupt this physiology with significant consequence.
[bg_faq_end][bg_faq_start]1) Differentiate chest wall injury, rib fracture, flail chest, costochondral separation and non-penetrating ballistic injury
[bg_faq_start]Chest Wall Injury
Chest wall injury (CWI) is a comprehensive term, including:
- Soft tissue injury
- Rib fracture
- Flail chest
- Sternal fracture
- Costochondral separation
50% with thoracic trauma have a CWI
- Often not obvious, and may be overlooked in the secondary survey!
- But an intact chest is essential to normal ventilation – for the inspiration and expiration cycles
- Those with limited reserve have more difficulty
- Elderly patients with pre-existing pulmonary disease – can’t tolerate even minor injury
- Many CWL can be missed if you don’t fully disrobe and observe RR, adequacy of tidal volumes, Respiratory Effort, palpation for tenderness, deformity, crepitus.
Rib fracture
- Most are simple rib#s
- Susceptibility increases with AGE
- Rib #’s don’t matter to us,
- Their potential complications DO!!
- Pneumothorax, hemothorax, pulmonary contusion, post-traumatic pneumonia, liver/spleen injury
- In children- rib fractures are correlated with underlying pulmonary injury
- Their potential complications DO!!
Anatomy and Physiology
- Ribs break at the point of impact or the weakest area, which is commonly the posterior angle/posteriolateral area.
- Usually ribs #4-9 break (1-3 are protected) and (9-12 are mobile and can penetrate intra-abdominally!)
- Think about spleen and liver injuries in LOW rib #’s
- Think about intra-thoracic injuries for ribs 1-3
- >2 ribs #’s = risk for internal injuries
Clinical features
- Tenderness, bony crepitus, ecchymosis, muscle spasm
- “Barrel compression test” for pain at the fracture site
Diagnostic features
- Clinical impression and physical findings are NOT specific to rib #’s
- CXR = often miss rib #s, but can find the intra-thoracic injuries.
- Rib specific views shouldn’t be ordered (in general!)
- Rib series, expiratory, oblique, cone-down views
- The only reason to get an x-ray in addition to **clinical suspicion** of rib fractures, is to look into intra-thoracic pathology.
- 50% of isolated single rib #’s are missed
- CT scans = much more sensitive
- Order a CT IF:
- Big mechanism of injury, physical exam findings of multiple rib #’s
- Elderly patient
- Lower rib #s
- Hemodynamic or respiratory compromise
- Rib specific views shouldn’t be ordered (in general!)
Management
- Two goals:
- Pain control
- Maintain pulmonary function – continue daily activities, and deep breathing
- Chest wall binders should be avoided – because they promote hypoventilation and atelectasis (this has never been supported with research or science though)
- Generally people with >3 rib #s may need hospitalization for pulmonary therapy and analgesia
- Especially elderly patients!
- Intercostal nerve blocks: – give about 12 hrs of analgesia
- 1% lido with 0.25% bupivacaine along the inferior rib margin several cm. Posterior to the site of fracture
- Block one rib above and one rib below
Clinical course:
- Most rib #s heal within 3-6 weeks
- Analgesia usually needed for weeks 1-2
Complications:
- Pneumothorax, hemothorax, pulmonary contusion, post-traumatic pneumonia, liver/spleen injury
- Post-traumatic neuroma
- Costochondral separation
- Separated rib #’s can lead to delayed hemorrhage → death
- Torn intercostal artery that re=bleeds
Flail chest
- Can be a life-threatening injury – due to large energy injury
- Usually associated with lung parenchymal injury
Definition:
- 3 or more ribs, fractured at 2 points leading to PARADOXICAL chest wall motion
- Can also occur with a vertical sternal fracture/costochondral injury
- This is one of the MOST SERIOUS chest wall injuries – 8-36% mortality rate, esp. in those with bilateral flail segments
- The lung contusion/parenchymal injury leads to altered ventilation/oxygenation
- The pain from the fractures leads to hypoventilation, hypoxia, atelectasis, etc
Physical exam:
- Requires thorough examination of the entire chest for asymmetrical movement
- Specific visual inspection can be guided by pain/crepitus
- Endotracheal intubation will mask the paradoxical movement
Imaging:
- May be missed on x-ray
- The exact rib#’s and pulmonary contusion will be found best on CT
Management:
- No ideal pre-hospital management
- Important to watch and deal with pain and hemo-pneumothorax ASAP
- These should be treated before considering intubation
- CPAP / non-invasive oxygenation strategies should be attempted first
- Consider cardiac monitoring and enzymes given the risk for cardiac injury/dysrhythmias
- Intubation only for ventilatory failure despite:
- Chest physiotherapy, oxygen/NIPPV, analgesia, high-nerve blocks, epidural analgesia
- People treated with these have much fewer complications
- Consider open-reduction and fixation of the rib #’s for patients with multiple ribs involved leading to decreased respiratory function, ventilated patients, incessant pain
- Evidence to support improved recovery, better cosmetics, improved function in those getting surgery
- Long term issues:
- Chronic pain, dyspnea, chest wall deformities
- Chest physiotherapy, oxygen/NIPPV, analgesia, high-nerve blocks, epidural analgesia
Costochondral separation
- Due to blunt trauma
- Rare
- Due to an injury to the cartilage
- Patients have a snapping sensation with deep inspiration
- Poorly detected on X-ray
- Takes many weeks to heal fully
Non-penetrating ballistic injury
- “-the chest wall cavity is intact-”
- But the kinetic energy is still enough to damage liver, lung, kidney, heart, spinal cord
Situations:
- Trauma caused by people wearing bullet resistant/bulletproof vests
- Trauma due to rubber bullets, bean bags
Clinical findings:
- Pain, areas of bruising and ++tenderness
- Key features not to miss
- Crepitus, subcutaneous air, retained foreign bodies, bony step-offs
Imaging:
- Basic radiography to exclude foreign bodies and associated pneumothorax/hemothorax
- CT should be considered
Management:
- Most should be admitted for overnight observation and serial examination
- Consider serial abdominal exams vs. CT abdomen
- *** Do not underestimate the risk and extent of injuries in the absence of penetration! ***
2) Describe the clinical presentation and management of a sternal fracture
>>> Check out this SGEM Article on Sternal Fracture!
- Due to anterior blunt chest wall trauma
- More likely in restrained passengers!
- Usually due to the diagonal strap running across the sternum
- A sternal # can mean less of the energy was dissipated to the internal organs
- More likely in restrained passengers!
- May be associated – in 10% of cases – with rib and lung contusions
- Non-displaced sternal #s
- Benign, <1% mortality, and low intra-thoracic morbidity, although mediastinal injuries should be considered.
- Cardiac complications are rare:
- 1-6%
- No association with aortic rupture
Main complications are mediastinal hematomas – which can lead to blood loss
- Clinical features:
- Anterior chest pain with point tenderness, swelling, ecchymosis, deformity
- Diagnosis
- CT > U/S > CXR
- Anyone with a suspected sternal # should get a CT
- Everyone should get an ECG
- Management
- Analgesia
- Discharge home if no other injuries
- Rarely surgery if very displaced.
3) Describe injuries to lung parenchyma:
[bg_faq_start]Subcutaneous emphysema
- In itself, free air in the sc. tissue is benign,
- But in the presence of thoracic trauma it represents an injury to air-containing structures:
- **clinical pearls***
- SC air in the supraclavicular and anterior neck area —> due to pneumomediastinum causes
- SC air in the chest wall. – due to intrapleural injury or penetrating trauma
- Extra-pleural injury
- From the tracheo-bronchial tree –
- Leads to air in the mediastinum, and neck
- RARELY leads to tension pneumo-mediastinum
- May have “hamman’s crunch” on heart auscultation
- Worsened by positive pressure ventilation
- Intra-pleural injury
- Due to a break in the visceral & parietal pleura
- Air then tracks into the SC tissue.
- Other etiologies
- Boerhaave’s syndrome – air in the neck and supraclavicular area
- Blunt or penetrating chest trauma – with or without an intrapleural injury
- Management:
- Tension pneumothorax or tension pneumomediastinum = all need drainage ASAP
- Chest tube or pericardiocentesis
- Smaller accumulations are treated based on underlying injury:
- Bronchial wall rupture
- Pneumothorax
- Esophageal injury
- Patients with isolated SC air – from a Valsalva – should receive high flow oxygen to help absorb the nitrogen-rich SC air which causes discomfort
- Tension pneumothorax or tension pneumomediastinum = all need drainage ASAP
- From the tracheo-bronchial tree –
Pulmonary Contusion
- Most common significant injury in blunt chest trauma – 30-70% of cases have a PC
- High risk populations:
- MVCs
- Pedestrian struck by motor vehicle
- Shock-wave induced injury from a bomb blast in air or water
- Ballistic or missile injuries
- Very common in children
- High risk populations:
Definition:
- Bruise to lung parenchyma tissue leading to alveolar hemorrhage and edema
- ****must be suspected clinically: the onset may be insidious and quickly become life threatening***
Clinical features:
- No clear signs to suggest Pulmonary contusion
- Commonly present with rib #s and flail segments
- BUT the MOST severe contusions occur in the absence of rib#s – as in pediatric patients (elasticity of the chest leading to more force transmitted to the lung)
- Symptoms:
- Dyspnea,
- Absent breath sounds, rales, hypotension, hypoxia, hemoptysis
- Tachycardia, cyanosis
Diagnosis:
- Must be careful not to miss the diagnosis based on clinical suspicion and distraction from other injuries that obscure the x-ray
- rib#, sc air, pneumonitis
- Xray = may show frank consolidation or patchy, irregular, alveolar infiltrates
- ARDS vs pulmonary contusion:
- PC appears in the first minutes to 6 hours and lasts 24-48 hrs
- ARDS is diffuse and bilateral, has a slow onset and comes on after 24-72 hrs
- X-ray is MUCH MORE effective at diagnosing clinically significant pulmonary contusions
- ARDS vs pulmonary contusion:
- CT scan
- CT chest, is more sensitive (2x) than x-ray, especially in the acute phase, and will find other potential injuries/issues
- However, many of the contusions may be occult and not as clinically important
- ABG:
- Probably the best means of assessing progression in the contusion (increasing A-a gradient)
- Bottom line:
- If the pulmonary contusion can only be seen on CT – it’s probably not clinically significant enough to change outcomes (handle it like any other blunt trauma to the chest), however…
- If seen on CXR and CT = these carry a high morbidity
- If the pulmonary contusion can only be seen on CT – it’s probably not clinically significant enough to change outcomes (handle it like any other blunt trauma to the chest), however…
Management
- Lung protective strategies
- Avoid over-administration of IV fluids
- Good pulmonary toileting
- Good pain control
- NO colloids
- No prophylactic antibiotics
- AVOID intubation and mechanical ventilation, especially in the context of flail chest (shown to increase morbidity)
- IF intubation is needed use a double lumen tube so that ventilation strategies can differ between the lungs
- Consider using CPAP and BiPAP
- Role for ECMO in severe cases
Pulmonary laceration
- Due to penetrating trauma, rib segment tearing the lung, a torn pulmonary adhesion
- Rare
- Can lead to persistent bleeding, hemopneumothorax
- Management:
- Oxygen
- Observe
- +/- thoracostomy, operative repair etc.
Pneumothorax
- Due to an injury in the parietal pleura
- Leads to paradoxical lung movement (collapse with inspiration due to negative intra-pleural pressure; and expansion with expiration
- Different types of pneumothorax:
- Simple
- “No communication with the atmosphere, NO mediastinal or diaphragm shift”
- May be
- Small
- Moderate – 15-60% of lung collapsed
- Large
- Often due to
- Rib#/penetrating trauma tearing the parietal pleura,
- May be due to blunt chest trauma with a full breathe and closed glottis leading to an alveoli rupture
- Communicating
- Due open connection with the world, creating a “sucking chest wound”
- Common in shotgun trauma
- Leads to paradoxical chest wall and lung movement
- Tension
- Sucking chest wound leading to a one-way valve, drawing more and more air into the chest without an escape.
- Leading to lung collapse, and contralateral compression of the lung, great vessels and veno-caval structures
- Leads to shock, hypoxia, decreased cardiac output and death
- Simple
Clinical features:
- Dyspnea
- Subcutaneous Air
- Wide spectrum based on severity: cyanosis ←-> no symptoms
- May have tachypnea, tachycardia, altered mental status
- Triad of tension pneumothorax:
- JVD
- Absent breath sounds (hyper-resonance)
- Tachycardia
- Hypoxia occurs first, and hypotension is a pre-terminal state
Diagnosis
- Can be very accurately dx’d on E-FAST ultrasound during the primary survey
- Thought to be more accurate than x-ray
- X-ray:
- Upright! Chest x-ray on max inspiration
- This may miss 30% of pneumothoraces initially
- If still suspected, do another film on expiration
- CT:
- Much more sensitive
- May find “occult” pneumothorax that wasn’t found on x-ray
- Tension pneumothorax is a CLINICAL dx, and x-ray rarely should delay treatment, although findings may be subtle at times.
- Upright! Chest x-ray on max inspiration
Management
- Depends on the size and clinical condition of the patient
- General rules:
- Blunt trauma:
- If initial CXR is negative, then a repeat should be done at 6 hours
- Penetrating trauma:
- If CT done with no pneumothorax – patient may be discharged
- IF CXR done and negative, a repeat CXR should be done at 3 hrs
- Simple:
- Size and symptoms usually guides treatment:
- If <15%
- Whether blunt or penetrating or spontaneous or traumatic
- Usually observation is adequate
- If >15% and/or symptomatic
- Tube thoracostomy is the best option
- If there are apical pneumothoraces:
- In the setting of penetrating trauma: stable patients with <25% involvement may be followed conservatively
- IN the setting of multisystem trauma – conservative observation is rarely safe or indicated, but this is based on clinical judgement
- Placement at the 4-5th intercostal space -AAL
- Safer and less scarring than going anteriorly in the 2nd ICS MCL
- Ensure it is place apical-posteriorly
- Ensure radiographic lines are inserted fully into chest
- Size depends on age
- Complications:
- Bronchopleural fistula, empyema, scarring, pleural leaks, inter-costal artery/vein injury, pneumonitis,
- Rosen’s recommends that anyone with a chest tube be on prophylactic antibiotics
- ***increased risk of re-expansion pulmonary edema for pneumothoraces that have been present for >3 days
- Communicating
- Care to have an occlusive dressing, that allows air to escape
- When in the ER – patient can get a tube thoracostomy in preparation for OR or intubation
- Tension Pneumothorax
- must be decompressed with finger thoracostomy or at least a 5 cm 14Ga angiocath
- In the 2-3rd ICS @ the MCL line
- OR
- The lateral chest 4-5th interspace AAL
- ****Must be suspected in the cardiac arrest patient who is getting PPV with CPR*****
- Ribs are at high risk of injuring the pleura
- This would be indicated by rapid difficulty in bagging
- must be decompressed with finger thoracostomy or at least a 5 cm 14Ga angiocath
- If <15%
- Size and symptoms usually guides treatment:
- Blunt trauma:
Hemothorax
- Can occur with blunt or penetrating trauma
- May lead to massive blood loss and altered chest ventilation
- Can occur with extra-thoracic injury
- Etiologies:
- Lung parenchyma (most spontaneously stop) >>> intercostal > internal mammary > other vessels. These don’t stop spontaneously and need surgery!
- Management
- See list of indications for OR thoracotomy
- Most worrisome:
- Continued loss of blood >200ml/hr for 3 consecutive hours
Clinical signs:
- Varying degrees of hypovolemic shock,
- Increased tactile fremitus and decreased breath sounds
Diagnosis:
- An upright CXR:
- Best test, as a supine film will often miss blood unless there is a large amount that layers posteriorly
- Need at least 200-300 ml of blood to blunt the costophrenic angles
- May see a tension hemothorax (rare)
- U/S may be used to see a pleural effusion with accuracy
- CT chest is much more accurate, finding 25% more compared with x-ray
Management
- Priorities:
- Restore blood volume
- Airway control
- Drain hemothorax using a large tube attached to a pleurivac
- CT is important, because the presence of a hemothorax often leads to tube drainage (when it is symptomatic or moderate in size)
- Small hemothoraces may be observed – but no study has been done to exactly describe which sizes of hemothorax need drainage
- Massive hemothoraces need operative thoracotomy or VATS
- Video assisted thorascopic surgery
Complications:
- Delayed hemothorax – leading to empyema and fibrothorax
- Errors in tube placement leading to lung parenchymal injury or persistent air
Tracheobronchial Injury
- Rare injury, with up to 10% mortality, may be occult
- May be due to penetrating or blunt injury
- Penetrating chest trauma from knives or GSW’s can injury any section
- Blunt trauma usually affects the tracheo-bronchial junction at the carina
- The tracheal cartilages can be burst from a forced punch to the neck or blunt chest trauma with a closed glottis (MVCs are the most common cause of TrachBronch Injury)
- Clinical signs:
- SC air, hamman’s crunch
- Group 1: Persistent air leak from chest tube – due to pleural injury
- Group 2: massive SC air, hamman’s crunch, pneumomediastinum
- Often due to 1-5th rib #s
- Diagnosis:
- Fibre optic bronchoscope is the most accurate
- CT also accurate
- Management:
- High flow oxygen
- Mediastinoscopy and possible repair with bronchoscope
- Small injuries with no complications can be watched conservatively
- Larger defects need:
- Fiberopotic intubation (so that a larger defect isn’t created) – with conversion to tracheostomy
- And operative thoracotomy for repair
- Associated esophageal injury must be evaluated
- Fiberopotic intubation (so that a larger defect isn’t created) – with conversion to tracheostomy
- SC air, hamman’s crunch
4) What is traumatic asphyxia?
- Rare problem due to marked massive influx of blood to the head and neck due to sudden thoracic compression, causing retrograde blood flow from the right heart backwards into the SVC
- 30% have a LOC
- Most people have a violet face/neck, bilateral conjunctival and petechial hemorrhages from the increased venous pressure
- Some may have anoxic brain injury due to prolonged hypoxia
- Managed by supportive care, screening for neuro deficits, signs of retinal hemorrhages,
- most-neuro deficits resolve spontaneously
- Consider CT chest based on mechanism
5) List 6 indication for tube thoracostomy (Box 45-1)
6) Indications for OR thoracotomy (Box 45-2)
7) What is the management of diaphragmatic injury?
Obvious herniation of abdominal compartments: consider intubation for PPV to bridge compression of lung parenchyma
Occult: Rosen’s recommends mandatory VATS to rule out diaphragmatic injury: REMEMBER there is high risk of future herniation if an injury is missed. Consult your local thoracic or trauma surgeon.
8) Differentiate between myocardial concussion, contusion and rupture
Myocardial concussion: commotio cordis “agitation of heart” result of direct blow to anterior chest. Result in non-perfusing rhythm, can be fatal (asystole or VF)
Contusion: direct injury to cardiac muscle cells: hemorrhage and edema can lead to immediate ventricular dysfunction or delayed pericarditis / scar formation and possible spontaneous rupture
Rupture: acute traumatic perforation on atria or ventricles and their surrounding structures (intra atrial or ventricular septum, chordae, valves, coronary arteries)
9) Review indications for ED thoracotomy (Box 45-3)
10) Describe your approach to identification and management of pericardial tamponade
Always think of this when patient profoundly shocky
- Beck’s Triad – hypotension, distended neck veins, muffled heart sounds
- CVP > 15 (who measures CVP in the ED?)
- When in doubt – sounds it out! EFAST for the win
11) CXR findings for blunt aortic injury
Possible in severe chest trauma or deceleration mechanisms (think motorbike crashing into wall)
Imaging findings on CXR
- Wide mediastinum in 50 – 92% of cases (Remember 6cm wide in erect PA, 8cm in AP supine)
- Obscured aortic knob
- Loss of PA window
- Displaced NG tube
- Widened paratracheal stripe
- Depressed left main bronchus
- Left pleural effusion
- Left apical cap
- Left tracheal deviation
12) List the 6 most common causes of esophageal perforation (Box 45-4)
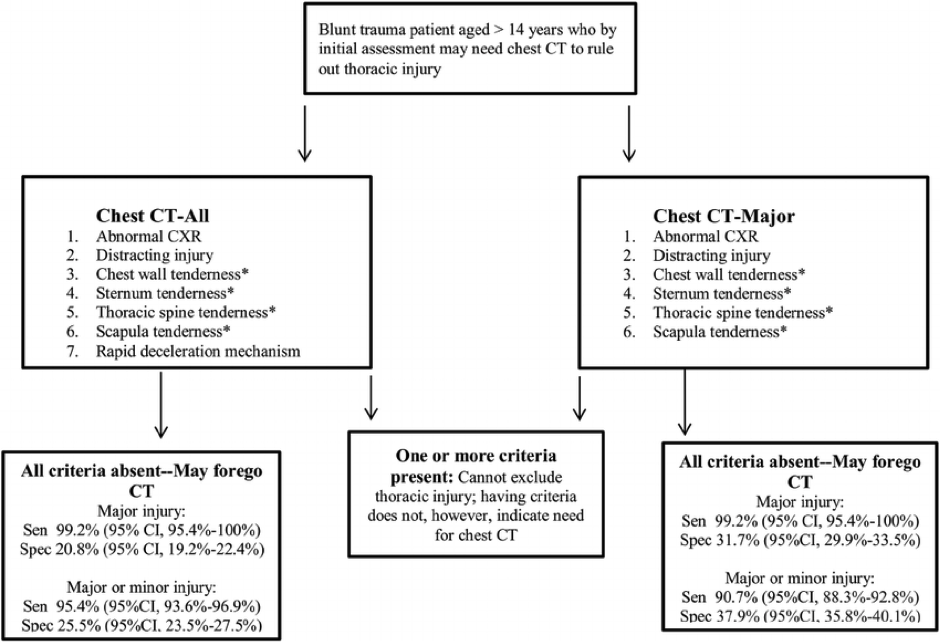
13) What is the Nexus CT Chest Rule
https://www.aliem.com/2015/nexus-chest-ct-decision-instruments-in-blunt-trauma/
http://www.mdcalc.com/nexus-chest-decision-instrument-for-blunt-chest-trauma/
Wise Cracks
1) Clinical conditions that mimic esophageal perforation (Box 45-5)
2) Describe the basic approach to ED thoracotomy
3) What is electrical alternans?
Produced as heart swings in massive pericardial effusion – QRS axis changes from swing to swing
[bg_faq_end]
This post was copyedited and uploaded by Riley Golby (@RileyJGolby)