This episode of CRACKCast covers Rosen’s Chapter 043, Spinal Injuries. Continuing in our series on all things trauma, this episode tackles the issue of spinal trauma focusing on mechanism of injuries, imaging guides, and management of various trauma patterns.
Shownotes – PDF Link
[bg_faq_start]Rosen’s in Perspective
- MVC’s are 40% of spinal injuries
- Risk factors: speeding, ETOH and failure to use restraints
- Other common causes in order: falls, violence, sporting activities
- 80% of spinal injuries are men
1) Describe the anatomical contents of the anterior, middle and posterior spinal columns (aka 3 column model of Denis)
- Anterior: alternative vertebral bodies and intervertebral disks surrounded by annulus fibrosis and anterior longitudinal ligament
- Middle: posterior portion of annulus and post vertebral wall, posterior longitudinal ligament, spinal cord, paired laminae and pedicles, articulating facets, transverse process, nerve roots and vertebral artery and veins
- Posterior: spinous processes, nuchal ligament, interspinous and supraspinous ligaments and ligamentum flavum
2) List cervical spinal injuries for the following mechanisms, and indicated whether they are stable or unstable:
- Flexion – From top down
- Atlanto-occipital or atlantoaxial joint dislocation (+/- odontoid #)
- Unstable due to lack or relative muscle and ligamentous support
- Simple wedge injury
- Stable provided posterior column remains intact and loss of no more than half vertebral height or multiple in a row
- Flexion teardrop – flexion forces cause anterior displacement of small wedge
- Highly unstable – usually involves anterior and posterior ligament disruption
- Clay-Shoveler’s fracture: named as such for miner lifting a heavy shovelful in forced flexion, now MC is forced deceleration in MVC’s
- Oblique fracture of base of spinous process – stable as single column
- Spinal subluxation – pure ligamentous disruption often very subtle
- Potentially unstable depending on degree of ligamentous injury
- Bilateral facet dislocations – flexion force disrupts all the soft tissue resulting in anterior displacement above spinal level
- Extremely unstable
- Atlanto-occipital or atlantoaxial joint dislocation (+/- odontoid #)
- Shear / AP forces
- Shear injuries occur with trauma to the head can result in odontoid fractures. Three types of odontoid fracture Type I-III indicated the level of fracture, and coincidentally the level of stability (from mostly unstable to fully instable)
- Upper part of odontoid peg
- Base of odontoid peg
- Odontoid into the lateral mass of C2
- Shear injuries occur with trauma to the head can result in odontoid fractures. Three types of odontoid fracture Type I-III indicated the level of fracture, and coincidentally the level of stability (from mostly unstable to fully instable)
- Flexion-Rotation x 2
- Rotary atlantoaxial dislocation – best visualized with an open-mouth odontoid view as lateral asymmetry between odontoid and the base of C2.
- Unstable
- Unilateral facet dislocation – Flexion rotation injury where the facet acts as a fulcrum, causing contralateral facet to dislocate. They key in the ED is often torticollis, as the patient neck is mechanically locked in a twisted position
- Stable
- Rotary atlantoaxial dislocation – best visualized with an open-mouth odontoid view as lateral asymmetry between odontoid and the base of C2.
- Extension x 3
- Posterior neural arch fracture – fracture of neural arch of c1 (just look it up…) from compression of posterior elements of c2
- Unstable secondary to location
- Hangman’s fracture – classically described as forced extension against a noose, this traumatic spondylosis of both pedicles of c2, now more commonly seen in MVC
- Technically unstable, but often without cord damage secondary to the very large neural canal diameter here
- Extension teardrop – abrupt extension results in ALL pulling off corner of anterior body. Usually associated with diving injuries.
- Unstable in extension and can have central cord syndrome as ligamentum flavum buckles into cord
- Posterior neural arch fracture – fracture of neural arch of c1 (just look it up…) from compression of posterior elements of c2
- Vertical Compression – forces from above or below
- Burst fracture – appears like wedge compression fracture, but typically <40% height. CT or MRI will show fragmented body.
- Stable but may impinge on anterior cord
- Jefferson Fracture – an eponymous fracture for a British neurologist who described this fracture. I like to think perhaps he was a weekend cliff diver, as this fracture is often seen with shallow water dives. Quite literally this is a compression force on c1 which bursts open the arch of the atlas. Diagnosis is oft made on CT but an open mouth view with c1 lateral masses > 7mm from odontoid peg is diagnostic.
- Extremely unstable
- Burst fracture – appears like wedge compression fracture, but typically <40% height. CT or MRI will show fragmented body.
3) List 8 unstable C-spine injuries
- Jefferson
- Odontoid fracture
- Atlanto-occipital dislocation
- Neural arch (posterior)
- Wedge fracture
- Large, facet dislocation
- Bilateral spinal subluxation
- Tear drop
Jefferson (radiopedia.org link to article)
Odontoid fracture (radiopaedia.org link to article)
Atlanto-occipital dislocation (radiopaedia.org link to article)
Wedge Fracture (emedicine link to article and picture)
Large Facet Dislocation (radiopaedia.org article linked here)
Teardrop Fracture (radiopaedia.org article link here)
4) Describe an approach to C-Spine X-rays, and define normal:
Considerations:
- Predental space
- Soft-tissue spaces
- Line of Swischuck
STEP ONE: Choose your type
- 3 main X-rays: Lateral, AP, and odontoid view.
- Additional view: swimmers view
- Useful for assessing cervical-thoraco junction (c7 to T1).
- Oblique view? Flex-EX? Forget it – if your suspicion of a fracture is this high, get the CT. Leave these other views to delayed imaging for specialist use
STEP TWO: ABC’s of lateral C/S films
- Alignment – 3 lines of the c/s. Anterior, posterior margins of vertebral bodies and spinolaminal line. Any disruption in these lines suggests a fracture
- Note exception is pseudo subluxation c2/c3 in young children secondary to hypermobile spine. Line of swischuk: line is drawn from anterior aspect of posterior arch of C1 to anterior aspect of posterior arch of C3. If distance between line is >2mm out – this can be fracture in child
- Bony abnormalities. Look for area of decreased density first as in patients with RA, Osteoporosis or metastatic lesions, as they are more likely to fracture. Then look for increase in density suggesting compression fracture
- Cartilage space – pay attention to intervertebral spacing as this may indication subluxation or dislocation
- Predental space: space between the tubercle of C1 and anterior face of the dens. Maximum 3mm in adults, 5mm in children. Widening of this space suggests atlantoaxial dislocation, but can be normal in conditions which cause ligamentous laxity or bony disruption such as downs syndrome and RA
- S for Soft tissue spaces
- 6/2 Rule – 6mm at C2 or 22mm at C6. Increases in these soft tissue distances can indicate prevertebral swelling and hemorrhage. At C3 and C4 its 5mm.
- Children: 6mm at C2, 14mm at c6… pesky small people
- 6/2 Rule – 6mm at C2 or 22mm at C6. Increases in these soft tissue distances can indicate prevertebral swelling and hemorrhage. At C3 and C4 its 5mm.
- Alignment – 3 lines of the c/s. Anterior, posterior margins of vertebral bodies and spinolaminal line. Any disruption in these lines suggests a fracture
STEP THREE: Odontoid view
- View is adequate if you see lateral processes of c1 and c2
- Looks for distance between peg and c1 lateral masses, should be equal
- Look for subtle fractures of odontoid
STEP FOUR: AP view – less useful
- Alignment – lateral edges of the C-spine and spinous process should form straight line
- Bony abnormalities – look at each vertebra for fracture lines[bg_faq_end]
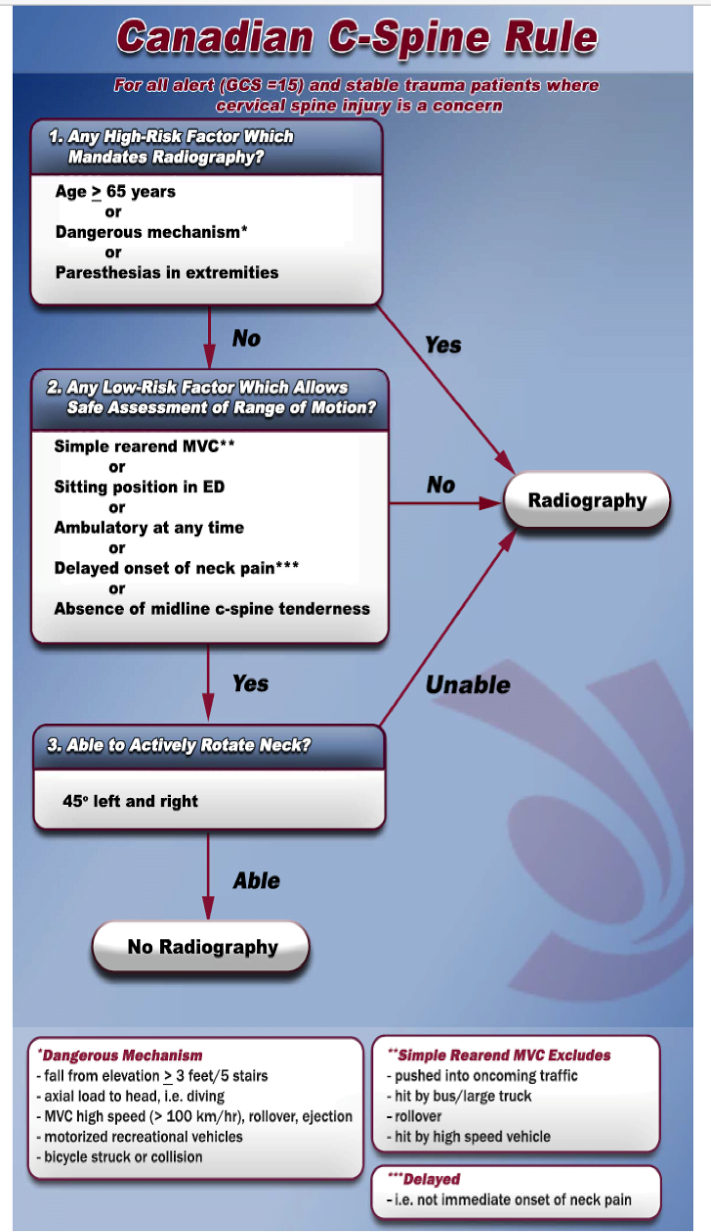
5) Describe the Canadian C-Spine Rule and Nexus Rule
CCS: prospective cohort study in Canadian adults presenting to tertiary care hospitals with acute trauma to the head or neck with GCS 15. Required one of the following: neck pain, or no neck pain + all of (injury above clavicles, non ambulatory and dangerous mechanism). Ian Stiells group generated a decision rule with sensitivity of 99.7% and specificity of 50.7 %.
Nexus rule: US single centre cohort (UCLA) of adult patients who suffered blunt trauma but sensitivity of 99.6, specificity of 12.9. Any of the following criteria mandates consideration for imaging of the C/S:
- Focal Neurologic Deficit Present
- Midline Spinal Tenderness Present
- Altered Level of Consciousness Present
- Intoxication Present
- Distracting Injury Present
6) Describe incomplete cord lesions
3 major types (account for 90% of incomplete injuries)
- Central cord syndrome
- Buckling of ligamentum flavour in patients with degenerative arthritis and hyperextension. Ligamentum flavum contuses the central grey matter. As distal nerve innervate the lower limbs, patients have relative sparing of the legs, however in severe cases only sacral sparing is seen. 50% become ambulatory again
- Anterior Cord Syndrome
- Hyperflexion or protrusion of bone/disk into canal or loss of anterior spinal canal (paresthesias and hyperalgesia with preservation of posterior column (position, touch, vibratory). Fast NS consult warranted for possible surgical fixes, as recovery is mostly within first 24 hours.
- Brown-Sequard
- Hemisection (lateral) of spinal cord. Often from penetrating trauma, but also masses. Results in ipsilateral loss of position, vibration and motor. Contralateral loss of pain and temperature. Pain and temperature loss may be variable in distribution and fibers cross over variable one or two segments above. Most patients become ambulatory again.
7) Describe the following clinical syndromes
- Wallenburgs Syndrome (aka lateral medullary syndrome)
- Loss of PICA circulation to the brain… remember your anatomy…PICA supplied by vertebral artery. Results in ischemia to lateral medulla = wallowing difficulty, or dysphagia, slurred speech, ataxia, facial pain, vertigo, nystagmus, Horner’s syndrome, diplopia, ataxia.
- Dejeune Onion Skin Pattern of Analgesia
- Damage to the spinal trigeminal tract = facial pain
- Other fun fact: the only link on google to this phenomenon links BACK to Rosen’s… so don’t ask me why ‘onion skin’
- Horners Syndrome
- Miosis, ptosis, anhydrosis.
- Damage to ipsilateral sympathetic cervical chain.
- Cauda Equina
- Every med student knows this one… bladder or bowel dysfunction, saddle paresthesias, diminished rectal tone, lower extremity weakness.
8) How does the bulbocavernosus reflex reflect the presence of spinal shock?
- What is spinal shock?
- Clinical syndrome characterized by temporary loss of neurologic function and autonomic tone below lesion. Lasts 24 hours to 2 weeks, and is heralded by the return of the bulbocavernosus reflex.
9) List features of sacral sparing
- Perianal sensation
- Rectal motor function
- Great toe flexor activity
10) List Dermatomes/ Myotomes / Spinal reflexes
11) List 6 causes of Horner’s Syndrome
- MS
- Encephalitis
- Tumours
- Lateral medullary syndrome
- Thyroid masses or removal
- Trauma to base of neck
- Pancoast tumor,
- Thoracic aneurysm
- Sympathectomy
12) For what C-spine injuries is CT-A indicated to rule out vascular injury
- C1-C3 #
- Any vertebral body fracture
- Transverse foramen fracture
- Facet sub/dislocation
- Ligamentous injury
This likely varies on a per institution basis
13) Are steroids indicated for C-spine injuries?
- Highly controversial – Cochrane review says yes, almost all other sources (guidelines and surveys) say no. Talk to your surgeon.
- Common dose is 30mg/kg IV methylprednisolone then infusion @ 5.4mg / kg/hr. Variable length of infusion
14) For whom is surgical intervention indicated immediately with a spinal cord injury
- Impingement on spinal cord by foreign bodies, herniated disks, bony fracture fragments or epidural hematoma
15) Define neurogenic shock and describe its management
- I prefer neurogenic hypotension (newest version of Rosen’s uses this). In contradistinction to spinal shock (see above), neurogenic hypotension is loss of vasomotor tone and lack of reflex tachycardia from disruption of autonomic ganglia.
- Should only be considered IF:
- Flaccid and areflexic
- Reflex tachycardia and peripheral vasoconstriction absent
- Exclusion of hemorrhage, tamponade, and tension pneumothorax
16) Define spinal shock
- As mentioned earlier – temporary loss of neurologic function and autonomic tone below the level of an acute spinal cord lesion
17) What is the risk of cervical injury in Down’s Syndrome? Rheumatoid Arthritis?
- Atlantoaxial instability leading to subluxation or dislocation for both – both diseases involve ligament laxity
18) What are the Denver criteria?
High risk vertebral signs and symptoms
- Any cervical spine fracture
- Unexplained neurological deficit incongruous with imaging
- Basilar cranial fracture into carotid canal
- Le Fort II or III fracture
- Cervical haematoma
- Horner syndrome
- Cervical bruit
- Ischaemic stroke
- Head injury with Glasgow Coma Scale score<6
- Hanging with anoxic injury
This post was copyedited and uploaded by Riley Golby (@RileyJGolby)