This episode of CRACKCast cover’s Rosen’s Chapter 038, Pediatric Trauma. Fortunately most emergency departments do not see major pediatric trauma frequently; however, it is important for the emergency physician to have the knowledge and skills to feel confident managing these high stakes, and at times high stress, situations.
Shownotes – PDF Link
[bg_faq_start]Rosen’s in Perspective:
Compared to adults, kids have:
- proportionally larger abdominal organs
- less subcutaneous fat
- less protective abdominal muscles
- proportionally larger kidneys
- flexible cartilaginous ribs that can compress internal organs without showing fractures
Diagnosis can be more difficult:
- very difficult to obtain complete history
- physical exam is plagued with difficulty
- tachypnea
- abdominal tenderness / bruising
- shock
- shoulder pain
- vomiting (late sign in child with duodenal hematoma or pancreatic injury)
- rectal exam is insensitive
- many orthopedic injuries can be missed in children
- head to toe exam: pit to finger exam!
- remember to remove backboard ASAP
- SERIAL exams are essential!
Pediatric Shock:
- have significant ability to compensate for blood loss
- Clinical Signs cool distal extremities, decreases in peripheral vs. central pulse quality, delayed cap refill, altered sensorium
- consider ultrasound early to detect occult bleeding
Family considerations:
- whenever possible, allow family to be there for the resuscitation
- keep them informed
- utilize social work and child life specialists if available
Investigations:
Labs:
- initial hemoglobin is unreliable – serial labs are necessary
- don’t forget to get a blood glucose
Radiology:
- Chest x-ray
- Pelvic x-ray Unless:
- age >3 and no complaint of injury
- no impaired LOC
- no major distracting injury
- no complaint of pelvic pain
- no signs of fracture on inspection
- no pain on pelvic stressing
- no pain on hip rotation or flexion
- more complete skeletal survey in young children suspected of having non-accidental trauma (NAT)
Here are some key formulas to know:
- cuffed ET:
- age in years/4 + 3.5
- uncuffed ET
- age in years/4 + 4
- tube depth
- age in years/2 + 12
- appropriate tube size X 3 = number of cm at the teeth that the ETT should be taped at.
- chest tube size:
- 2 x ETT size
- femoral line: 3-6 F.
1) List 5 relevant anatomic/physiologic differences between children and adults in relation to trauma management
1. More widely distributed forces in a child = multiple injuries more likely to occur due to structural differences
- Brain is less protected: thinner cranial bones, less myelination
- More anterior inner organs with less muscle and fat: liver, spleen, and less protected spleen
- Pulmonary injuries occur without skeletal injuries due to elastic ribs
- Open growth plates = salter-type fractures with long term implications
- Spinal Cord Injuries without Radiographic Abnormalities (SCIWORA) injuries occur due to an elastic vertebral column and tenuous blood supply.
2. Larger surface area = prone to heat loss —> hypothermia = negative effect on cardiac function, inotropy, LV contractility, platelet function, renal and hepatic drug clearance, metabolic academia, and can result in coagulopathy.
3. Higher proportional requirements for free water, electrolytes, minerals due to higher metabolism
4. Higher 02 consumption and glucose utilization per kg = need energy and calories sooner – due to increased metabolism
5. Great capacity to maintain BP despite 25-30% blood loss
- little role for inotropy: blood pressure mostly dependent on chronotropy and SVR
- tachycardia and slow cap. refill are warning signs of impending decompensation!**
2) List 8 airway differences between pediatrics and adults with their relevant implications
| Differences | Implications | |
| Physiologic | Increased vagal response to laryngoscopy | Bradycardia – have atropine on hand! |
| Anatomic | Larger tongue | #1 cause of airway obstruction; need better head positioning +/- OPA/NPA |
| Larger adenoidal tissues | Nasotracheal intubation and NPA’s are tougher to insert | |
| Floppy epiglottis more U shaped | “use miller blade” (false dogma) and change in intubation technique – ‘insert Miller blade into the esophagus and then SLOWLY withdraw until you see the glottis’ | |
| Cephalad, anterior larynx | tougher to visualize the cords, need to angle 45 deg. forward to see them | |
| Cricoid ring the most narrow part of the airway (the first cricoid cartilage of the trachea) | May need uncuffed tubes in kids <8 yrs (or need to downsize slightly) | |
| Narrow tracheal diameter and distance between rings | Needle cric. for kids <12 yrs: not surgical airway | |
| SHORTER tracheal length; large airways more narrow | Right mainstem intubation (neck extension) and EASY dislodgement of tube (neck flexion) ; greater airway resistance |
3) List potential fluid therapies for hemorrhagic shock and their doses
- standard trauma/resus protocol : MOVIE
- Monitor
- Oxygen
- Vitals
- IV
- ECG
- 10-20ml/kg of crystalloid IV bolus repeated up to three times then consider:
- PRBCs: 10 ml/kg
- FFP: 25 ml/kg
- Platelets: 10 ml/kg
4) List 3 ideal IO sites in pediatrics and describe the procedure
Need to use the mantra “1-2-IO” – safe and effective way to establish venous access. Don’t waste precious minutes on the peripheral IV.
- IV access: if not readily available do an IO
- proximal medial tibia
- proximal humerus
- anterior distal femur
Check out LITFL for more on IO insertion.
[bg_faq_end] [bg_faq_start]5) Describe the pediatric Glasgow Comma Scale (GCS)
AVPU system / age appropriate GCS score
- the problem with the pediatric GCS is that it DOESN’T help you prognosticate neurological outcome (no validation) and has poor inter-rater reliability
- children with poor scores can have great outcomes
| Eyes | Verbal | Motor: |
| 4 – Spontaneous | 5 – appropriate cry and coo | 6 – normal spontaneous movement |
| 3 – To voice | 4 – irritable cry | 5 – withdraws to touch |
| 2 – To Pain | 3 – inconsolable cry | 4 – withdraws to pain |
| 1 – Unresponsive | 2 – grunts | 3 – flexion to pain |
| 1 – no verbal response | 2 – extension to pain | |
| 1 – no motor response |
Signs of herniation might be indicated by:
- pupil size and reactivity
- extremity movement and tone
- posturing and reflexes
Treatment:
- mannitol 0.5 g/kg IV; maintain CPP of at least 50
assess for spinal injury
6) List 7 indications for laparotomy
- hemodynamic instability despite aggressive resuscitation
- free fluid on FAST and unstable vitals signs
- massive bleeding (intraperitoneal)
- pneumoperitoneum / intraperitoneal bladder rupture / grade V renovascular injury
- gunshot wound
- evisceration
- peritonitis
[bg_faq_end] [bg_faq_start]
7) List 6 signs of elevated ICP in infants and children
Signs of increased ICP in infants
- full fontanel
- split sutures
- altered state of consciousness
- paradoxical irritability
- persistent emesis
- setting sun sign
Signs of increased ICP in children
- headache
- stiff neck
- photophobia
- altered mental status
- persistent emesis
- cranial nerve involvement
- papilledema
- hypertension, bradycardia, hypoventilation
- decorticate and decerebrate posturing
8) What is an impact seizure?
With respect to head injury, there are several important anatomic differences between pediatrics and adults:
- larger, heavier cranial vault
- high amount of torque on the cervical spine axis in toddlers and infants
- malleable sutures
- brain parenchymal damage without skull fractures
***this highlights the principle that in kids: they get soft tissue damage WITHOUT showing fractures!!***
Less myelinated brain with higher water content
- more susceptible to shearing forces and further injury
Key points on history:
- height of fall, method of landing, surface of impact, use of restraints, helmet use, LOC immediately after injury, signs of progressive lethargy/irritability/ recurrent vomiting/etc.
- vomiting is an unclear prognostic indicator : may just be a familial predisposition to vomiting vs. intracranial injury
- impact seizure: a seizure with immediate return to normal mental status after the post-ictal period: usually NOT associated with parenchymal injury.
- seizures > 20 mins from injury portend greater possibility of TBI and need for CT and neurosurgery consult.
Physical exam:
- ABC’s interventions
- maintain oxygenation and perfusion
- optimize glucose
- euvolemia
- CPP = MAP – ICP
- no matter what a child’s neuro presentation in the ED careful resuscitation is needed
9) List the 5 layers of the scalp and describe 3 types of extra cranial bleeding in pediatrics
Layers of the scalp – use the SCALP mnemonic:
S – Skin
C – Connective Tissue
A – Aponeurosis
L – Loose Connective Tissue
P – Periosteum
Caput succedaneum: hematoma, freely mobile and crosses suture lines
Cephalohematoma:
- blood UNDER periosteum = does NOT cross suture lines
- scalp bleeding can be profuse and lead to shock in infants
Cerebral contusions
- clearly demonstrable on CT scan as a brain parenchymal injury
- neuro features with altered MS
10) What is the difference between a linear and a diastatic skull fracture
Skull fracture factors associated with poor outcomes:
1) fracture over a vascular channel
2) a depressed fracture
3) a diastatic fracture
- cross through/along suture lines and leptomeningeal cysts (growing fractures) may develop (>2mm of separation)
4) fracture extending over the area of the medial meningeal artery
5) rhinorrhea, otorrhea
[bg_faq_end] [bg_faq_start]11) Describe the typical presentation and etiologic cause of an epidural hematoma and a subdural hematoma
Epidural hematoma
- “head injury: lucid interval: followed by rapid deterioration”
- due to VENOUS bleeds in kids (adults = arterial bleed)
- delayed signs and symptoms
- highly associated with overlying skull fractures
Subdural hematoma
- usually associated with rupture of bridging veins.
- most common in kids <2 yrs. of age
- may be chronic in the child
- with “shaken baby syndrome” or NAT
- vague: vomiting failure to thrive, altered LOC, seizures.
- need fundoscopic exam to rule out retinal hemorrhage pathognomonic of NAT (non-accidental trauma)
- with “shaken baby syndrome” or NAT
[bg_faq_end] [bg_faq_start]
12) Describe the management of elevated ICP
Diagnostic strategies:
- serial exams are key
- absence of focal findings doesn’t rule out injury
- papilledema requires days to develop
- cushing’s response is ominous
- monro-kellie doctrine
- as ICP increases – brain perfusion/ability to autoregulate decreases
- herniation syndromes:
- uncal herniation
- unilaterally dilated pupil
- compression of ipsilateral third nerve, contralateral hemiplegia, hyperventilation
- “down and out pupil”
- may progress to frank apnea and cardiac arrest
- unilaterally dilated pupil
- uncal herniation
Treatment:
- **prophylactic treatment with anticonvulsants not recommended **
- incidence of post-traumatic seizures is low
- treatment of increased ICP: non-pharmacologic methods and pharmacologic methods
- 1) non-pharmacologic
- elevate HOB >30 deg
- head in midline
- avoid hyperthermia
- mild hypothermia
- maintain euvolemia
- decompressive craniotomy
- 2) Pharmacologic
- Mannitol (0.5 g/kg IV)
- rapid osmotic diuresis
- Hypertonic saline (0.1-1 mL/kg of 3% saline)
- Pentobarbital / phenobarbital
- lowers cerebral metabolism
- Neuromuscular blockade
- Sedation
- Treat seizures aggressively
- Mannitol (0.5 g/kg IV)
- Stop gap therapies:
- hyperventilation for ACUTE increase in ICP (temporary fix)
- 1) non-pharmacologic
13) List 10 anatomical differences between the pediatric and adult cervical spine
Spinal Cord Injuries in Pediatrics:
- rare
- higher cord injuries are more common
- SCIWORA (Spinal Cord Injury without Radiography Abnormality) – found in 25-50% of spinal injuries
Principles of disease
- C-spine features approach adult patterns around age 8-10.
- Key differences in the pediatrics cervical spine:
- higher fulcrum C2-3 (higher c spine injuries)
- larger head size – greater flexion and extension injuries
- smaller neck muscle mass
- increase interspinous lig. flexibility
- flatter facet joints
- incomplete ossification at multiple bony sites
- anterior surfaces of the vertebral bodies are more wedge shaped
- Epiphytes of spinous processes tips mimic fractures
- Narrow predontoind space
- Pseudosubluxation of C2-3 seen on 40% of children 8-12 yrs
- Pre vertebral space varies with respiration
Clinical features
- need to consider MOI; standard trauma primary survey
- C-spine injury indicators
- tenderness in the body c-spine area
- paralysis or paresthesias
- ptosis
- priapism
- incomplete (some motor or sensory function below the level of the lesion) vs complete lesions
- NOT a one-time assessment: to be continued until spinal shock resolves
- exam tests:
- bulbocavernosus reflex
- rectal or anal wink
Cord syndromes:
| Central cord | Anterior cord | Brown_sequard | |
| Extension injury | Flexion injury | Hemisection of the cord | |
| arm tone < leg tone distal symptoms > proximal **burning dysesthesias in fingers and hands*** | complete motor paralysis, loss of pain and temperature sensation position and vibration is preserved
| ipsilateral loss of motor function and proprioception at the level of transection contralateral loss of pain and temperature sensation one or two levels below the lesion |
Radiology
- NEXUS criteria:
- but very few kids in the study actually had SCI and no cases of SCIWORA
- <1% of the kids in the study had an injury
- most of the injured cases were older than 9 years
- CT C-spine is the imaging of choice:
- don’t bother with x-ray if you’re actually suspicious of a cervical injury
- poor sensitivity of plain radiographs at detecting bony fractures
- Plain radiographic clearing requires:
- imaging the C7-T1 interface
- three views of the c spine
- predental space < 6mm in kids less than 6 years
- prevertebral space < 1/2-1/3 the vertebral body width
- the four cervical radiographic lines:
- patients with persistent neck pain despite negative radiographs and CT should get an MRI
- flex / ext. views are rarely helpful
Management:
- Two phases of SCI
- Direct injury : irreversible injury
- due to ischemia, hypoxia, tissue death
- Spinal shock
- Injury above T1:
- lower extremity findings of SCI: flaccid paralysis of skeletal and smooth muscle leading to hypovolemia due to decreased SVR
- resolves in hours to day(s)
- Injury above T1:
- Neurogenic shock
- injury above T6
- loss of sympathetic tone and have UNOPPOSED parasympathetic tone: hypotension and bradycardia
- treatment: atropine, ino-pressors, fluids are used
- backboards should be removed ASAP: only use is for extraction
- Direct injury : irreversible injury
14) How can you discern between true subluxation and pseudosubluxation at C2/C3
- Pseudosubluxation of the c-Spine at C2-3 is common in kids
- Swischuk line
- spinolaminar line of C1-3, If the line crosses C2’s anterior cortical margin by less than 2 mm, (and no cervical soft tissue swelling and no fracture is seen) the image demonstrates pseudosubluxation
- Swischuk line

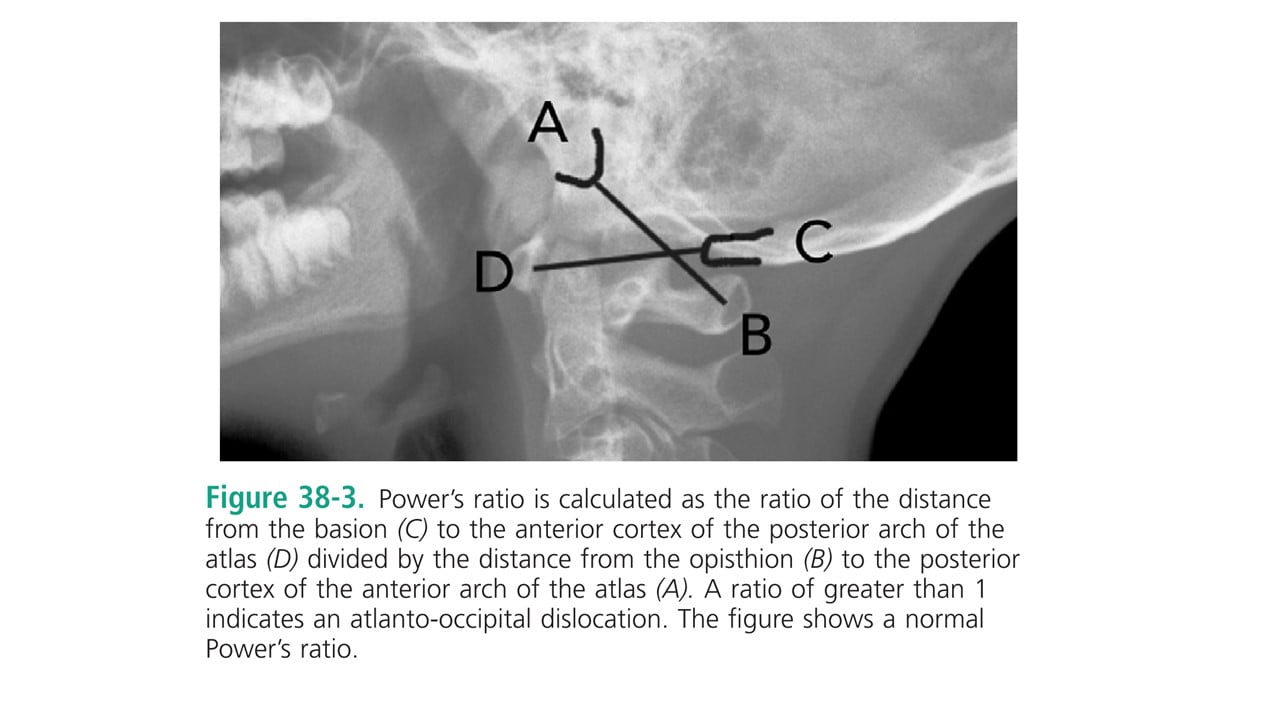
- occipital cervical junction injuries:
- suspect in any child pedestrian vs. vehicle injury
- with a big chin laceration
- most of these injuries are immediately fatal
- Power’s ratio > 1 indicates atlanto-occipital dislocation
- Normal = 0.77
- distance from D to C / distance from A to B
- suspect in any child pedestrian vs. vehicle injury
15) List 2 ways to choose the size of chest tube in pediatrics
2 X ETT size
4 X ETT size
[bg_faq_end] [bg_faq_start]
16) What are indications for ER resuscitative thoracotomy in chest trauma?
- RARE
- same indications as adults (see episode on Major Trauma)
- penetrating chest trauma with signs of life and less than 15 min of CPR
- blunt trauma with signs of life and pericardial tamponade with <10 mins of CPR
17) List pediatric specific cardiovascular and abdominal injury patterns
Principles of disease:
- impairment of diaphragmatic breathing impairs ventilation
- children’s only way of improving ventilation is with increased RR
- gastric distension impairs vital capacity
- end-tidal CO2 is helpful
- ribs are more compliant, so rib fractures are usually associated with massive trauma or in the setting of abuse: their absence doesn’t rule out a serious injury
Specific injuries:
Pneumothorax:
- widespread transmission of breath sounds can mislead the clinician
- **listen in the axilla***
- <20% pneumothorax with no need for transport or ventilation may be watched
- ultrasound highly sensitive and specific for detecting ultrasound
Open pneumothorax:
- bidirectional flow of air
- significantly impairs oxygenation and ventilation
- treatment:
- three sided occlusive dressing
- separate incision with chest tube
Tension pneumothorax
- one-way valve
- signs are often SUBTLE in pediatric patients
- emergent decompression with needle or finger
Hemothorax:
- difficult to identify on supine CXR
- rare; associated with big mechanism of injury
- need large tube drainage
- operating room thoracotomy if:
- >15ml/kg of blood immediately exudes
- continuous air leak
Pulmonary contusion:
- chest compliance in children puts them at increased risk of contusion even in the absence of external chest trauma
Traumatic diaphragmatic hernia
- associated with MVC’s and lap belt use
- need to consider comorbid small bowel injury/hematoma and CHANCE fractures
- Treatment insert NG tube to decompress the stomach; avoid BVM; intubation and surgery
Cardiac and vascular injuries:
- rare
- similar signs and symptoms as in adults
- watch for pericardial tamponade
- need thoracotomy
- commotio cordis
- sudden impact to the anterior chest which stops cardiac function or leads to a dysrhythmia
- shock may persist despite resuscitation efforts
- may need long term antiarrhythmic agents, pacemakers, and cardiac support
Abdominal injury
- most common cause of unrecognized fatal injury in children
- most often associated with MVC’s
So now to answer the specific question:
- Three injuries assoc. with lap belt use:
- small bowel injury/hematoma
- pancreatitis
- chance fractures
- bike handlebar injuries
- duodenal hematoma
- pancreatic transection/trauma
- sports related:
- spleen, kidney, intestinal tract
Diagnostic strategies and management:
- abdominal distention is common due to ingested air
- early foley catheter helps decompress the bladder and assess U/O
- FAST ultrasound: If positive and patient stable –> on to CT +/- angiography
- indications for laparotomy:
- hemodynamic instability despite aggressive resuscitation
- free fluid on FAST and instability
- massive bleeding intraperitoneal despite blood
- pneumoperitoneum / intraperitoneal bladder rupture / grade V renovasc. injury
- gunshot wound
- evisceration
- peritonitis
Spleen injury
- most common injury
- need hospital admission
Livery Injury
- most common cause of lethal hemorrhage
- need close hospital observation, serial exams and hemoglobins
Penetrating injury:
- DPL : only performed in low resource settings
Disposition
ED role:
- resuscitation and stabilization and transfer to appropriate facility
- avoid extensive imaging if your centre can’t deal with the results
- low threshold for admission with serial exams
Cessation of care:
- obvious if
- livor mortis, rigor mortis, massive injuries
- attempts should be made if there are signs of life
- parental presence during resuscitation should be encouraged
This post was uploaded by Ross Prager (@ross_prager)