This episode of CRACKCast covers Rosen’s Chapter 011, Neonatal Resuscitation. In these cases you hope you have help around you to care for these fragile patients, and this episode focuses on some of the key perinatal considerations.
Shownotes – PDF Link
[bg_faq_start]1) List the equipment needed for neonatal resuscitation
- PPE equipment – gown, gloves, mask etc.
- blankets to warm and dry the neonate
- radiant warmer
- airway stuff
- bulb syringe / meconium aspirator
- suction catheters size 5,8,10
- self-inflating BVM + reservoir bag
- various BVM masks: premee, infant, etc.
- laryngoscope with blades 00 , 0 , 1
- ET tubes with stylets: 2.5 / 3 / 3.5 / 4
- airway securing gear: tape, scissors
- confirmation equipment:
- CO2 detector
- stethoscope
- chest x-ray machine
- equipment for umbilical vein catheterization
- umbilical catheters # 3.5 and #5
- three-way stop-cock.
- provodine
- drapes
- PPE equipment
- scalpel, hemostats
- suture
2) List 5 questions to ask the mother during an imminent delivery
- What is the estimated gestational age?
- Is this a multiple gestation?
- Is meconium present?
- Is there a history of vaginal bleeding?
- Were medications given during delivery or drugs taken intrapartum?
3) Describe the components of the initial assessment of the newborn (APGAR)
- In the acute resuscitation phase we really only care about the HR and respiratory effort
- APGAR = Appearance, Pulse, Grimace, Activity, Respirations
4) What is the management of meconium?
- Meconium in amniotic fluid = sign of fetal distress in utero
- Previous guidelines recommended routine suctioning of non-vigorous neonates that had meconium stained amniotic fluid
- However, thinking has changed:
- Tracheal suctioning only if:
- absent or depressed respirations (gasping, poor oxygenation)
- poor muscle tone
- HR < 100 bpm
- usually need two passes of ETT guided suctioning:
- intubate child and place suction catheter inside ETT (to 100 mmHg suction) and withdraw both to aspirate the meconium
- if bradycardia and apnea continue → BVM and intubate
Bottom line: don’t let the meconium trip you up.
- Treat (suction) the neonate based on either:
- Inadequate respiratory effort or HR < 100 bpm
5) When should oxygen be used in the neonatal resuscitation period?
- oxygen is a drug, and a neonate should be initially resuscitated on room air
- goal is that the SP02 of a neonate be above 80% by ten minutes after birth
- supplemental oxygen is thought to be toxic to neonatal lungs, brains, and eyes – don’t routinely give it
- after 15-20min SP02 goal is 90-95% NOT 100%
6) What is the indication for CPR in a neonate?
- CPR is started if the HR is < 60bpm ** despite adequate ventilation for 30 seconds**
7) Describe how to perform CPR on a neonate
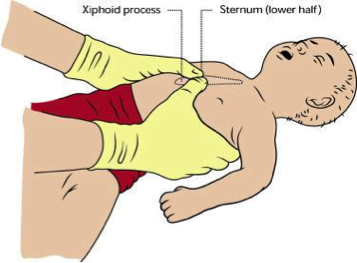
Either the encircling hands technique or two fingers on the lower ⅓ of the sternum. But the encircling hands generates higher systolic and coronary perfusion pressures
Don’t forget the 5 Ps!
Ratio is 3:1
8) What are the indications for intubation of a neonate?
Same as adults but a few more:
- respiratory distress
- increased work of breathing (retractions)
- desaturations
- tachypnea
- administration of surfactant via ETT
9) List 4 reasons not to resuscitate a newborn
- <23 weeks gestational age
- <400 g birthweight
- confirmed anencephaly
- trisomy 13
- trisomy 18
If unsure start resuscitation!
[bg_faq_end][bg_faq_start]Wisecracks:
1) What are some special considerations for resuscitating a preterm infant?
[bg_faq_start]Rosen’s in Perspective:
Key principles to guide resuscitation:
- newborns have rapidly changing cardiopulmonary physiology, and as such have:
- their own unique vital signs
- unique stress responses
- focus entirely on respiratory management (not cardiovascular)
- need special equipment
Three key components of neonatal physiology:
- Hypoxia
- Hypothermia
- Hypoglycemia
Pathophysiology of the transition for intra to extrauterine life
Two changes must occur:
1) removal of fluid from unexpanded alveoli to allow ventilation
2) redistribution of cardiac output to provide lung perfusion because:
- the fetal lung is poorly perfused
- due to vasoconstriction (only 40% of the RV cardiac output goes to the lung)
- most to the pulm. artery → ductus arteriosus → descending aorta
At birth
- baby breathes → alveolar oxygen decreases pulmonary vascular resistance
- the fetal shunt through the ductus arteriosus closes (due to increased systemic vascular resistance)
- shunt usually closes by 15 hrs of age
- after shunt closes all the RV output goes to the lungs
- **with hypoxia or acidosis the pulmonary vascular bed constricts and the ductus may reopen**
- this leads to persistent fetal circulation
- *** resuscitation facilitates the first few breaths – and prevents and reverses ongoing hypoxia and acidosis — is essential to the transition to extrauterine life ***
Key points:
- respirations do not necessarily = adequate ventilation
- hypoxia = cyanosis, lethargy, unresponsiveness
- bradycardia (HR < 100 bpm) = inadequate oxygenation and ventilation
- pulse oximetry will not be normal in a neonate until >15 mins
- bradycardia = hypoxia
Hypothermia:
- newborns are unable to generate heat by shivering and cannot retain heat due to low fat stores and large body surface area
- at risk for heat loss due to amniotic, wet fluid covering, the cool hospital environment
- low temperatures lead to:
- metabolic acidosis
- increased 02 consumption
- hypoglycemia
- apnea
- Treatment: dry and warm the baby!
Hypoglycemia
- peripheral glucose < 40 mg/dL (~2.5 mmol/L)
- at risk due to:
- poor glycogen stores
- immature liver enzymes
- diabetic mothers
- preemies or small for GA
- develops in response to:
- illness
- hypothermia
- polycythemia
- asphyxia
- sepsis
- may be asymptomatic!
- symptoms:
- apnea, colour changes, resp. distress, lethargy, jitteriness, seizures, acidosis
- poor myocardial contractility
2) Describe the Neonatal Resuscitation algorithm
Simply Described:
1) Preparation
- get the right people
- get the right stuff
2) 5 steps of resuscitative delivery
Dr. Lipp’s memory aid:
“WARM PASS neonate, Ventilate then Intubate, Compress LOW Rate, Avoid a cold fate”
- WARM/dry
- PASS- position, assess, stimulate, suction
- Ventilate – use CPAP or PPV with any signs of resp. distress
- Intubate – if you are going to suction, do CPR, or BVMs aren’t effective
- Compress at low rate – if any bradycardia start CPR at <60 bpm
- To avoid a cold fate – if there is neonatal asphyxia and ROSC after resuscitation start therapeutic hypothermia
Step 1: time 0-30 sec: warm, position, suction, stimulate, assess
- dry off amniotic fluid ASAP
- replace with warm blankets
- position to achieve maximum air entry
- put the neck in slight extension (put a folded towel under the infant’s shoulders)
- suction only if:
- meconium present AND:
- poor tone, poor respirations
- bradycardia,
- large volume of secretions
- ***deep suctioning can lead to vagal stimulation = bradycardia/apnea***
- meconium present AND:
- stimulate by rubbing feet, back, etc.
- assess:
- in the first 30 seconds:
- baby’s response to warming, drying and stimulation
- HR
- Palpate stump, listen, ECG
- if HR <100 or apnea
- start PPV (see step two)
- if no response and HR<60 start CPR
- APGAR scores:
- **in the acute resuscitation all we should care about is the HR and respiratory effort**
- in the first 30 seconds:
Step 2: 60-120 sec: ventilation, oxygen, intubation
- any cyanosis or respiratory distress:
- start CPAP or PPV
- first breaths need 30-40 mmHg, subsequent need 20 mmHg
- RR 40-60 breaths/min
- if you bag for >2 mins, put in an OG tube
- use room air initially
- ***know that the O2 sat. doesn’t reach >90% until more than 10 mins
- indications for intubation:
- need for tracheal suctioning
- ineffective BVM
- CPR started
- if there is any deterioration post intubation:
- think through the DOPE list (displacement, obstruction, pneumothorax, equipment failure)
- revert to BVM or insert an LMA
- start CPAP or PPV
Step 3: 180 sec – onwards: chest compression
- bradycardia in a neonate is an indication of hypoxemia
- ***any neonate with HR <60 despite adequate oxygenation and ventilation for a least 30 seconds should get CPR
- rate: 90 bpm with 30 vents / min
- ratio of 3:1 in general
- if it’s thought to be a cardiac cause then the 15:2 ratio can be used.
- use the encircling hands technique
- compress ⅓ the AP depth
- reassess every 30-60 seconds
Step 4: resuscitative medications
- medications are indicated:
- bradycardia/asystole
- hemorrhage
Suitable medications:
- Oxygen
- use for persistent bradycardia
- use for respiratory distress lasting 90 seconds (after all the other measures have been attempted (controversial)
- Epinephrine
- indications:
- i) asystole
- ii) HR < 60 despite effective ventilations with 100% O2 and CPR
- ideally administered IV
- i) dose:
- 01 to 0.03 mg/kg OR
- 1 ml to 0.3ml/kg of 1:10000
- ii) repeat q3-5mins
- i) dose:
- if the ET route is used a higher dose is needed (0.1mg/kg)
- indications:
- Naloxone
- only for the neonate who is adequately ventilated
- great for the mother who received opioids during labour
- shouldn’t be used for the narcotic addicted mother:
- i) it may precipitate withdrawal seizures
- dose: 0.1mg/kg IV, IO, or SC or IM
- repeat dosing at 4 hrs may be needed
- Glucose
- should be checked on every newborn
- any glucose < 3.5 mmol/L with symptoms should be treated:
- i) symptoms:
- irritability
- tremors
- jitteriness
- apnea
- tachypnea
- seizures
- cyanosis
- lethargy
- poor feeding
- i) symptoms:
- treatment:
- i) IV glucose
- D10W 2-5 ml/kg, with an infusion of D10W at 80-100 ml/kg/day
- ii) higher concentrations of glucose should be avoided because they are hyperosmolar
- i) IV glucose
- iii) **encourage breast or bottle feeds**
- asymptomatic neonates with very low glucoses (<~2.6) should be treated empirically
- volume expanders
- indicated with signs of acute bleeding or hypovolemia (cyanosis despite resuscitation, shock, CPR required)
- use O- PRBCs – 10 ml/kg
- NS
- Ringers
- dopamine
- rarely indicated
- infused at 5-20 mcg/kg/min
Vascular access:
- immediate access through the umbilical vein← best choice
- femoral line
- IO access (although very challenging due to fragile bones)
Medications that should NOT be used routinely:
- albumin
- dopamine
- calcium
- bicarbonate
- atropine
Step 5: Therapeutic hypothermia
- for early neonatal asphyxia:
- symptoms: altered LOC, seizures, hypovolemia, hyporeflexia
- in mod-severe hypoxemic encephalopathy: selective cerebral hypothermia in asphyxiated infants may protect against brain injury
- hypothermia at 33.5-34.5 degrees in the neonatal population leads to lower mortality and less neurologic disability at 18 months of age
- **controversy whether whole body vs. head alone should be cooled**
- start cooling within 6 hrs of birth and continue for 72 hrs
3) A quick review of specific neonatal disorders:
- Diaphragmatic hernia
- Meningomyelocele
- Omphalocele
- Choanal atresia
- Pierre-Robin sequence
Diaphragmatic Hernia:
- as soon as diagnosed, the child should be intubated!
- ventilation distends the stomach and worsen respiratory distress because it is in the chest cavity
Meningomyelocele/Omphalocele:
- should not be placed on the their backs:
- put on their sides / stomachs
- cover the spinal defect in sterile gauze pads soaked in warm sterile saline
- infants with gastroschisis or omphalocele should be resuscitated and have the defect covered in plastic to decrease water and heat loss
Choanal Atresia: (absence of nasal passageways)
- leads to bilateral upper airway obstruction and respiratory distress
- diagnosed by inability to pass catheter through either nare:
- Treatment: intubate or oral airway
Pierre-Robin Sequence:
- genetic disease
- small jaws, large tongue = upper airway obstruction
- Treatment
- nasal or oral airway
- intubation → may fail so be ready with LMA
4) Neonatal Resuscitation Case
You are working in a community ED. A code pink is called: g2p1 — 36 weeks with the head visible.
Elevator thoughts: get the right people, the right stuff
On arrival the infant is cyanotic, limp, with poor resp. effort:
- Cut and clamp the cord
- Dry, warm, stimulate!!
Pale, poor resp effort, HR 40
- how do you measure HR?:
- auscultation
- three lead ECG
- umbilical stump palpation
- Start PPV! with room AIR
- only increase the FiO2 ratio later on in the resuscitation.
No response after 30 seconds.
- ways to make ventilation better
- “MR SOPA”
- mask reposition
- suction
- open mouth
- increase pressure
- acquire airway
- intubate
- use an LMA
- “MR SOPA”
No response
- start CPR:
- sequence and timing for compressions and ventilations “1-2-3 breathe, 1-2-3- breath”
- give glucose
- give narcan
- start epinephrine.
Normal values:
- HR 100-180
- RR 40-60
- SP02 at 10 mins 85-90%
- 60% at 1 min
Initial steps:
- now have 1 min to start PPV
- stimulate, position, suction airway, dry and WARM.
- PPV:
- count it out:
- “Breathe – 2 — 3; breathe – 2– 3-”
- RR 40-60 goal
- IF HR < 60 despite CPR
- give epi
- NS bolus 10 ml/kg
- consider needle decompression
- Venous access issues:
- IO generally not that reliable in the first few days of life
- umbilical line
- look for the SMILE
- the arteries are symmetric like eyes.
- put it in the irregularly shaped structure.
- take a 5 FR flushed line with a stopcock insert to 5 cm, then check for blood return, insert till you get blood back, then get someone to hold the catheter in place
- look for the SMILE
- ET tube:
- don’t give narcan via ET tube
- epi can be given at a higher dose.
- count it out:
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)