Case: You are working as a 3rd year clerk in the ED and your staff has asked you to see Kathy, a 24 year old female caught in a house fire presenting with burns in multiple areas and difficulties breathing.
Burn injuries result in the partial or complete destruction of the skin and can affect any of its three layers: the epidermis, dermis, or subcutaneous tissue.1 In this article, we will explore a basic approach to managing burns in the ED and learn how to manage the case of Kathy.
Test yourself: Kathy comes in through an ambulance, what is the first most important step?
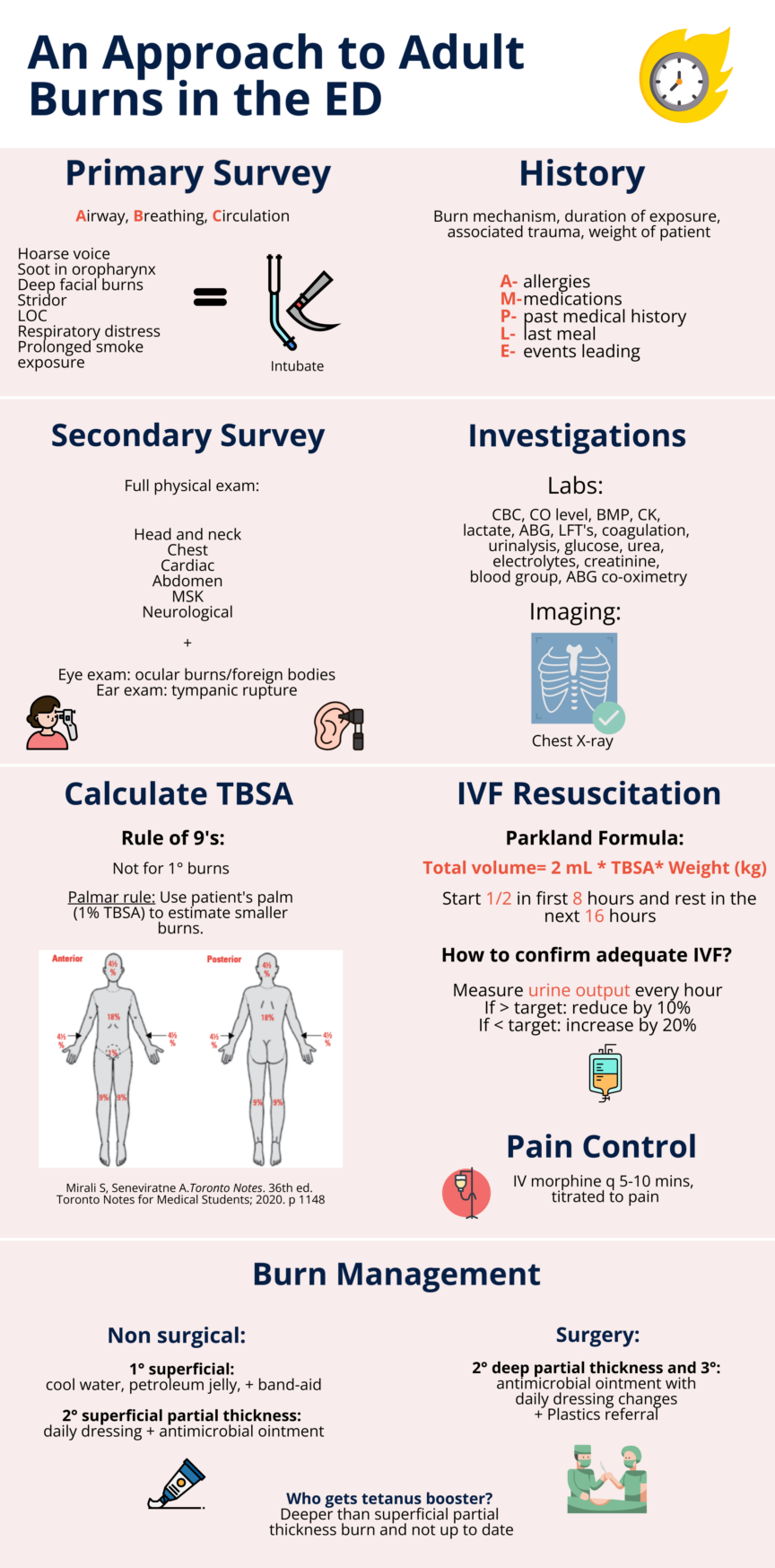
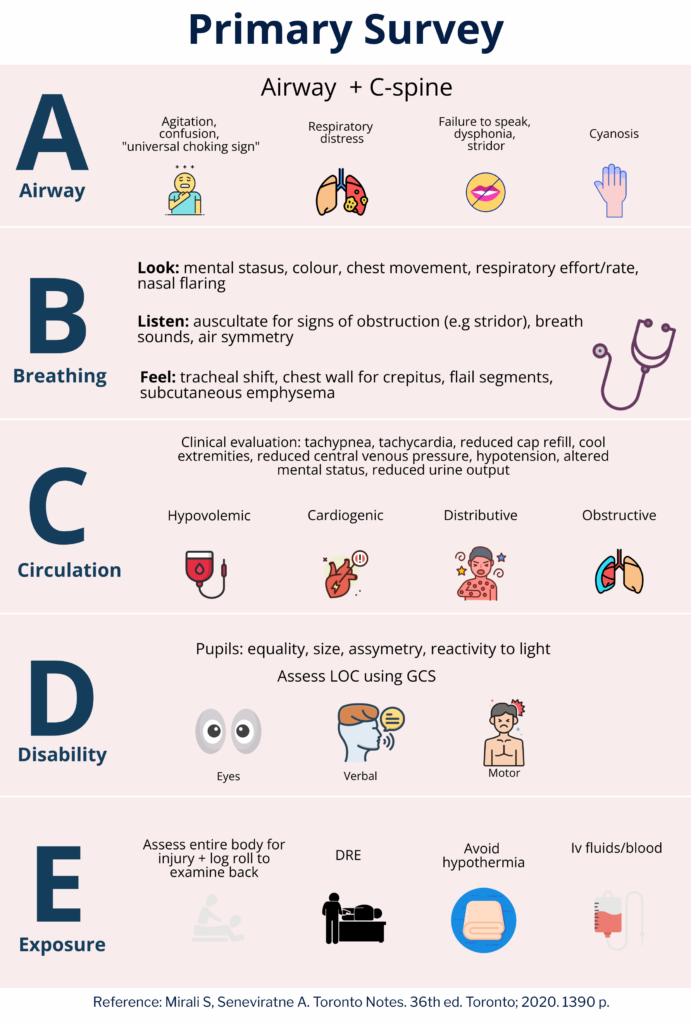
Primary Survey
Although it is important to assess all components of the primary survey, the utmost priority in a burn patient is the airway. Burns can lead to upper airway injuries above the vocal cords, resulting in severe edema, while lower airway injuries are typically caused by smoke particles and result in inflammation and edema. Key indicators of airway injury in a burn patient include hoarseness of voice, soot in the oropharynx, deep facial burns, stridor, loss of consciousness, and prolonged smoke exposure. 2,3 To evaluate the severity of the burn and prepare for intubation, a non-invasive endoscopic examination of the airway while the patient is awake can be beneficial. In any case of burn injury, suspicion for airway injury is paramount, and patients should receive supplemental oxygen and undergo X-ray evaluation.4
Test yourself: Upon primary survey, Kathy is able to answer all your questions with some coughing in between and rapid breathing. You use an endoscope to examine her airway and see a thin smooth tracheal wall with some black-stained mucous. Her GCS is 15. Does she need to be intubated?
Yes. It appears that there is soot present in Kathy’s airway, as evidenced by the black-stained mucous. In order to prevent potential airway obstruction due to anticipated edema, it is crucial that we take steps to stabilize her breathing. Therefore, we should intubate Kathy to ensure that her airway is properly splinted open with a tube. This will help to ensure her safety and stabilize her condition. For intubating Kathy, use the largest endotracheal tube (8 mm) to account for potential airway swelling common in severe burn patients. Ensure the tube’s correct placement by checking for equal breath sounds on both sides using a stethoscope and avoid any misplaced sounds, like those over the stomach. A chest X-ray can further confirm its optimal position relative to the lungs
History
Test yourself: While you were conducting your primary survey, your staff was taking a history from her mom. What are the most important questions to ask on history?
It is crucial to start by obtaining the mechanism of the burn which can include electrical, chemical, radiation, friction, and the most common being thermal. Next, determine the duration of exposure, extent of injury, risk of smoke inhalation, associated trauma, and co-existing comorbidities. 5 Assessing for any loss of consciousness is paramount.

When evaluating a burn patient, it is essential to follow the AMPLE approach, which includes assessing for allergies, medications, past medical history, last meal, and events leading to the presentation. 4 Furthermore, knowing the patient’s weight is crucial for determining appropriate treatment. The answers to these questions will guide your plan.
Case continued: Kathy’s mom describes Kathy being stuck in a house fire for 15 minutes which has resulted in burns to her right leg. She states that Kathy has no associated trauma, allergies, medical conditions, or medication use, and had her last meal about 12 hours ago. Kathy weighs 80 kg.
Resuscitation
Resuscitation of a burn patient is a crucial aspect of management and is performed concurrently with the primary survey. Intravenous fluid (IVF) resuscitation is not indicated for 1° burns, but it is generally required for 2° burns or higher if the total body surface area (TBSA) affected is greater than 15%. However, it is important to note that 15% TBSA is not an absolute threshold, and less aggressive fluid resuscitation may be administered for TBSA lower than this. Aggressive IVF resuscitation is usually necessary due to the systemic inflammatory response that frequently develops with more extensive burns. This response can lead to burn shock, hypovolemia, and ultimately, organ failure. The primary goals of resuscitation are to maintain adequate tissue perfusion and oxygenation, which can help prevent these complications and improve patient outcomes.3 It is important to note that a 16-18 gauge IV should be used and placed on non-burned skin of upper extremity.
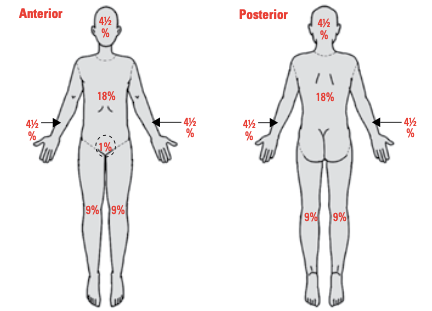
How to calculate burn size?
Rule of 9’s: The burn size is expressed as % of TBSA and is not calculated for 1° burns. 3 To calculate the burn size we can use the rule of 9’s. See figure 2.
Palmar rule: The palm of the patient (not fingers or wrist area) is about 1% of the body. It is uncommon for a burn to cover the whole arm, chest or leg. In such cases, the patient’s palm can be used to estimate the burn size. 3
Test yourself: Calculate Kathy’s burn size in %TBSA assuming the following areas are affected: 1/2 of her chest, 1/2 of her stomach, 2/3 anterior right leg and foot and 3 palms covering the anterior left leg.
- 1/2 the chest ~4.5%
- 1/2 stomach ~4.5%
- 2/3 anterior right leg and foot ~6%
- 3 palm width covering the anterior left leg ~3%
Total % TBSA ~ 18%
How to determine the amount of IVF resuscitation?
The total volume of resuscitation required for the patient is based on the Parkland Formula:2
- Total Volume = 2 mL Ringers lactate * TBSA (%) * Weight (kg)
- Administer ½ in the first 8 hours the rest in the next 16 hours
Note: This formula is not a rule to be strictly adhered to but rather serves as a useful guideline to determine where to begin.
Burn patients often experience intense pain. In the Emergency Department (ED), it’s essential to follow established guidelines for pain relief. Morphine dosing guidelines recommend 0.1 ml/kg for children and 2.5-5 ml/kg for adults, administered every 15 minutes via IV until comfort is achieved.
Test yourself: Calculate the total volume needed for Kathy. Recall that Kathy weighs 80 kg. Bonus question: Calculate the hourly rate of fluid infusion.
- Total Volume = 2 mL * 18 % * 80 kg= 2880 mL= 2.88L
- First 8 hours= 2.88 L/2= 1.44 L
- Hourly rate: 0.18 L/hr
- Other 16 hours= 1.44 L
- Hourly rate= 0.09 L/hr
How to confirm appropriate IVF administration?
Proper monitoring of urine output is critical in patients undergoing resuscitation to ensure optimal organ perfusion. To achieve this, insertion of a Foley catheter is recommended, with a target urine output of 0.5-1 mL/kg/hr. It is imperative to measure urine output hourly to accurately assess the patient’s condition.4
- If urine output exceeds the target then reduce fluid resuscitation by 10% because over-resuscitation can lead to edema and eventual tissue hypoxia. 4
- If urine output is falls below the target then increase fluid resuscitation by 20% because under-resuscitation can cause hypotension and eventual renal failure.4
In addition to monitoring urine output, vital signs such as heart rate and mean arterial pressure should be monitored every 5-15 minutes. The aim is to maintain a heart rate of less than 120 and a mean arterial pressure greater than 70 to ensure adequate organ perfusion. Any other life-threatening conditions should also be identified promptly.3
Secondary Survey
Physical Exam
The secondary survey should be conducted after the primary survey. This involves a thorough physical examination of the head and neck, chest, abdomen, musculoskeletal system, and neurological system. It’s important to also perform an eye exam to check for intra-ocular foreign bodies and ocular burns, as well as an ear exam to look for tympanic rupture for blast injuries.4
Pain Control
Pain control should be initiated after starting IV fluids, and IV morphine can be given every 5-10 minutes, titrated to pain.5
Investigations
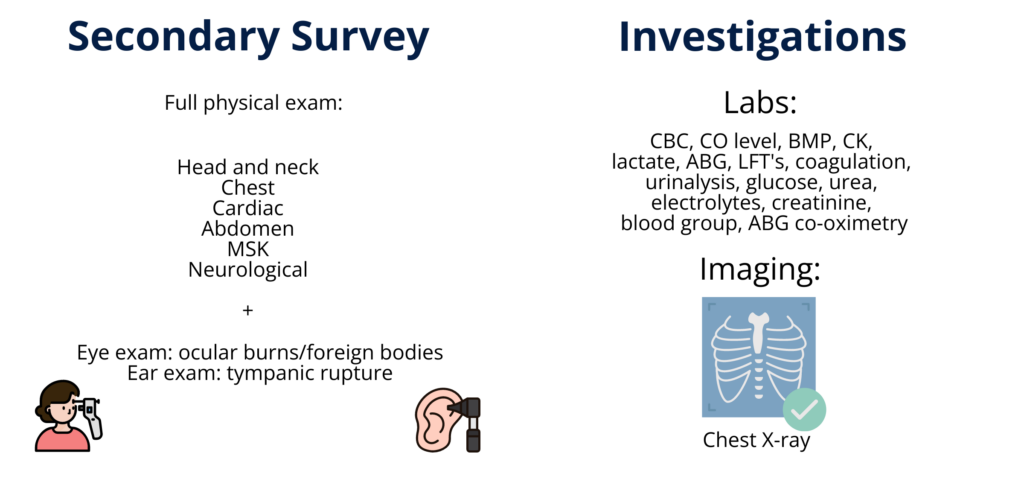
Simultaneously we want to order crucial labs including CBC, electrolytes, urea, creatinine, CO level, BMP (basal metabolic panel), CK, lactate, LFT’s, coagulation, urinalysis, blood group, and glucose.5 We must also order an ABG with co-oximetry to assess for potential CO exposure that might require treatment modifications.
Imaging
Initial imaging should include a chest x-ray to assess for possible lung damage in the case of a suspected inhalation injury.1
Case continued: We have now stabilized Kathy by intubating her and starting IVF resuscitation, and are now controlling her pain as well as ordering key labs and investigations. Next, we must manage the burn itself.
Burn Management
Burn Classification
Accurate assessment of the degree of burn injury is crucial in determining the appropriate management strategy, whether surgical or non-surgical modalities are indicated. A systematic approach to burn classification, as illustrated in figure 3, should be employed to ensure optimal management outcomes. Notably, the initial estimation of burn depth can be challenging and requires reassessment after a 24-hour period. It is worth noting that burn injuries are often not uniform, with the central region experiencing the most significant impact, while the periphery may exhibit a milder degree of injury. Consequently, the edges of the burn wound may display characteristics more consistent with a first-degree burn, despite the presence of a deeper partial-thickness burn. Most burn centres employ a laser doppler which can assist in assessing burn depth.
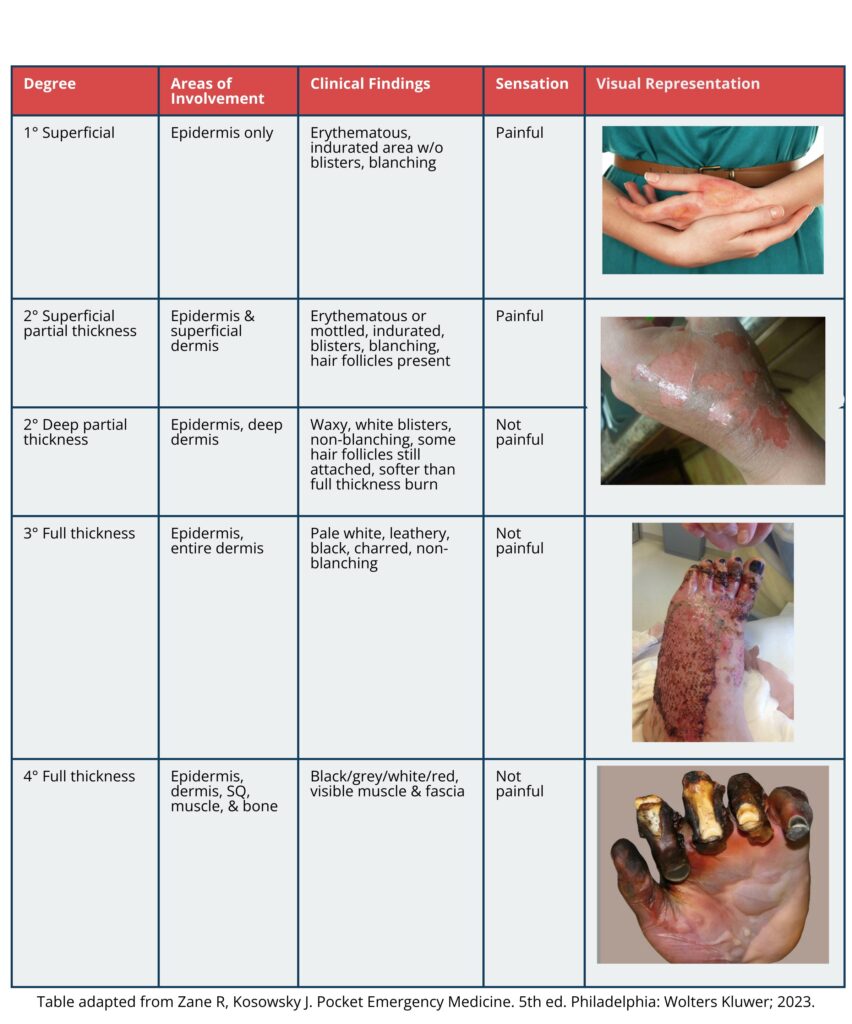

Test yourself: You take a look at the skin on her right leg and it appears red, dry, blistered, and hair remains attached. The skin is non-blanchable and demonstrates a lack of sensation in areas with deeper burns, with localized pain surrounding these areas. What degree of burn is this?
2° deep partial thickness burn
Burn Treatment
The first initial step for a burn is to urgently cover the burn wounds with saran wrap. This approach not only controls pain and minimizes heat loss but also allows for a definitive examination by the burn team later on. Using Saran Wrap avoids the unnecessary effort by primary care providers in applying dressings that the burn team would eventually have to remove, thus saving time and resources.
| 1° Superficial | 2° Superficial Partial | 2° Deep Partial Thickness | 3° Full Thickness | |
| Prognosis | Require no surgery and will heal in 2 weeks with no scars. | Require no surgery and will heal in 2 weeks with no scars. | Requires more than 2 weeks for healing, requires surgery, and will create a hypertrophic scar. | Requires more than 2 weeks for healing, requires surgery, and will create a hypertrophic scar. |
| Management | Immerse the burn in cool tap water, apply petroleum jelly 2 or 3 times a day, apply a band aid over the burn, and give acetaminophen as needed. | Daily dressing changes with antimicrobial ointment (polysporin, bactroban, flamazine, silver nitrate, hypochlorous acid). Acetaminophen as needed. | Daily dressing changes with antimicrobial dressings (Silver Dressings/ Acticoat). Refer to plastics for a flap or skin graft.6 | Daily dressing changes with antimicrobial dressings. Refer to plastics for a flap or skin graft.6 |
Patients with deeper than superficial-partial thickness burn require tetanus booster if they are not up to date to help prevent the spread of infection.
Patients with deep second-degree and full-thickness burns require surgical intervention within the initial week following the burn by burn trained surgeons. Notably, approximately 70% of these severe burns lead to the formation of hypertrophic scars—raised, red, and often itchy. Over time, these scars undergo a transformative healing process, evolving into mature scars over months or even years
Complications
| Acute | Subacute | Chronic |
| Airway compromise Burn shock Impaired perfusion Hypothermia | Sepsis Hypermetabolism Compartment syndrome | Hypertrophic scar7 Contractures |
Indications for Transfer to Burn Unit
- TBSA >10% in child and older than 65 years old for partial thickness burns
- TBSA >20% partial thickness burns.
- > 5% for full thickness
- Respiratory insufficiency
- Partial or full thickness burns involving face, neck , genitalia, eyes, ears, and or major joints
- Burns with significant electrical, chemical, inhalational, or traumatic injury6
In certain areas, it is possible that a designated burn center may not be readily accessible. In such cases, the presence of key indicators such as those mentioned above may serve as valuable guidance to prompt consultation with a specialized burn unit. Whether a patient needs to be transferred or not will depend upon their injuries and local resources.
Case Conclusion:
To manage Kathy’s 2° deep partial burn, it is important we apply antibiotic ointment such as polysporin alongside a tetanus shot as her skin is exposed and at risk for infection. To prevent drying out of the wound and possibly delay healing, we must order daily dressing changes to the wound. Given the severity of the burn and the potential for complications, it is unlikely that the wound will heal on its own, necessitating further interventions such as referral to Plastics for a skin graft. Finally, a tertiary survey will be conducted in a calm environment after all initial investigations are completed to fully characterize all her injuries.
This post is copyedited by @aafia-maqsood and @mauz-asghar.
References
- 1.Schaefer T, Szymanski K. Burn Evaluation and Management. StatPearls. Published online August 23, 2022. http://www.ncbi.nlm.nih.gov/books/NBK430741/
- 2.Walls R, Gausche-Hill M, Hockberger R. Rosen’s Emergency Medicine: Concepts and Clinical Practice: 2-Volume Set. . 9th ed. Elsevier; 2022.
- 3.Mirali S, Seneviratne A. Toronto Notes. 36th ed. Toronto Notes for Medical Students; 2020.
- 4.Kwan P. Acute Burn Injuries . YouTube. Published 2019. https://www.youtube.com/watch?v=4hcPn9f2gNY
- 5.Zane R, Kosowosky J. Pocket Emergency Medicine. 5th ed. Wolters Kluwer; 2023.
- 6.Jeffrey J. Essentials of Plastic Surgery. Thieme Publishers New York; 2022.
- 7.Wong J, Lin W, Ding J, Tredget EE. Prevention and management of scarring after thermal injury. PAR. Published online January 28, 2021. doi:10.20517/2347-9264.2020.171
Reviewing with the staff
Dr. Tredget is a distinguished plastic surgeon affiliated with the University of Alberta. He holds esteemed positions as the Director of both the Firefighters\' Burn Treatment Unit at the University of Alberta Hospital and the Burn Wound Healing Research Laboratory within the university. His research predominantly involves wound healing, hypertrophic scarring, and tissue engineering post burn injuries.
Reviewing with the staff
Dr. Brent Thoma is a medical educator, blogging geek, and trauma/emergency physician who works at the University of Saskatchewan College of Medicine. He founded BoringEM and is the CEO of CanadiEM.