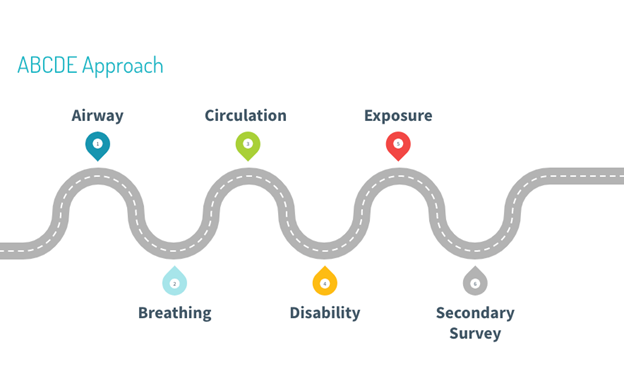
The ABCDE approach applies to the initial assessment of critically ill patients. For each step, appropriate treatment should be started regardless if there is a definitive diagnosis.
Airway1–3
- Fatal in minutes.
- Think of this separately from breathing!
- Consider what would you do if the airway became threatened, e.g. Have you assessed for predictors of difficult airway management?
| Assessment | Management |
| ● Determine if patient can speak. ● Inspect for secretions or foreign bodies. ● Check for signs of airway obstruction. | ● Assess for potential risks to the airway and difficulties in airway management. ● Call for help early. ● Start basic airway maneuvers (e.g. head tilt, chin lift). ● Suction. ● Remove foreign bodies. ● Place a nasopharyngeal, oropharyngeal or supraglottic airway. ● Examine for predictors of a difficult airway. ● Consider intubation. ● Treat the underlying cause, if known. ● Check for signs of airway obstruction. |
Breathing1–3
- Think ventilation vs. oxygenation
- Give oxygen
| Assessment | Management |
| ● Vital signs (respiration rate, O2 saturation). ● Signs of increased work of breathing. ● Reduced air entry or abnormal breath sounds on auscultation. | ● Apnea requires bag-valve-mask ventilation. ● Specific conditions require immediate treatment: ❖ Tension pneumothorax: Perform a needle decompression or thoracostomy followed by chest tube ❖ Bronchospasm: Administer bronchodilators ❖ Hypoxia: Administer O2 ❖ Anaphylaxis: Administer IM epinephrine |
Circulation1,3
- Identify the cause of shock
| Assessment | Management |
| ● Vital signs (heart rate, blood pressure, capillary refill time). ● Check volume status: ❖ Hypervolemia (e.g. edema, extra heart sounds, jugular-venous distension) ❖ Hypovolemia (e.g. decreased skin turgor, delayed capillary refill, dry mucous membranes) ● Auscultate for abnormal heart sounds. ● Palpate extremities, pulses, and abdomen. ● Inspect the five areas blood can go: ❖ Abdomen (including the retroperitoneum) ❖ Chest ❖ Pelvis ❖ Long bones ❖ Floor (i.e. external) | ● Insert two large bore IVs. ● Identify the type of shock, then treat. ● In the event of a hypertensive emergency, administer IV antihypertensives. |
Disability1–3
- Determine if this is in the brain (i.e. lateralizing lesion like blood) vs. something else (metabolic, toxins, drugs)
| Assessment | Management |
| ● Assess vital signs (i.e. GCS, pupils, movement of extremities, blood glucose level). ● Assess for agitation. ● Conduct pupillary exam. ● Assess for signs of increased intracranial pressure and meningitis. ● Attempt to identify common toxidromes. | ● Verbal de-escalation before using medications or restraints. ● Treat hypoglycemia with the Rule of 50s. |
Exposure1,3
- Check from head to toe to identify signs of trauma, toxins or stigmata of disease
| Assessment | Management |
| ● Vital signs (i.e. temperature, weight for pediatric patient). ● Check for signs of occult trauma: Examine the axilla, groin, and back with C-spine precautions (i.e. log roll maneuver). ● Collect a SAMPLE history and perform a full-body examination for signs of a possible underlying etiology. | ● Remove possible allergens or contamination sources (e.g. cholinergic toxins can affect providers; consider personal protective equipment for possible infectious disease). ● Provide patient with clean clothes/a hospital gown. ● In the event of hypothermia, offer a warm blanked and warm IV fluids, as well as antipyretics if indicated ● In the event of hyperthermia, consider immersing in cold water and administering cold IV fluids. ● Administer specific treatments if the diagnosis is known. |
Secondary Survey
The purpose of this stage is to search for an underlying cause. Here, you should obtain a detailed history and perform a full-body physical exam.1
This post was copy-edited by Geordon Omand.
References
- 1.AMBOSS . ABCDE Approach. AMBOSS. Published March 2022. https://next.amboss.com/us/article/YI0nYh?q=abcde#references
- 2.Rob W. Basic Airway Assessment: It’s as easy as… 1-2-3? CanadiEM. Published August 4, 2014. Accessed December 27, 2021. https://canadiem.org/basic-airway-assessment-easy-1-2-3/
- 3.Steve H. What to Do in a Resuscitation as a Junior Learner. CanadiEM. Published November 17, 2020. Accessed December 27, 2021. https://canadiem.org/what-to-do-in-a-resuscitation-as-a-junior-learner/
Reviewing with the Staff
The ABCDE approach is at the heart of answering the question - Is my patient sick? When reviewing undifferentiated patients it is important to not only identify current threats to life, but
also to anticipate potential difficulties. By breaking down the ABCDE into clear distinct steps of assessment, listing your potential key differentials and linking your acute managements you can cognitively rehearse what you would need to do. Visualizing these steps before you actually have to do them helps give you confidence and reassurance that when the time comes to act you recall what to do. Practice this approach daily, especially with not sick patients so you remove the stress of the situation and ensure you can hone your approach. You’ll only see a handful of sick patients in your training, so take the time with your other patients to simulate these steps until you have it down to a science!