This is part of the CanadiEM Teaching That Counts Infographic Series, where we take the current research and evidence on how to teach well in the emergency department, and distill it down into bite-sized chunks that are rapidly digestible and memorable.
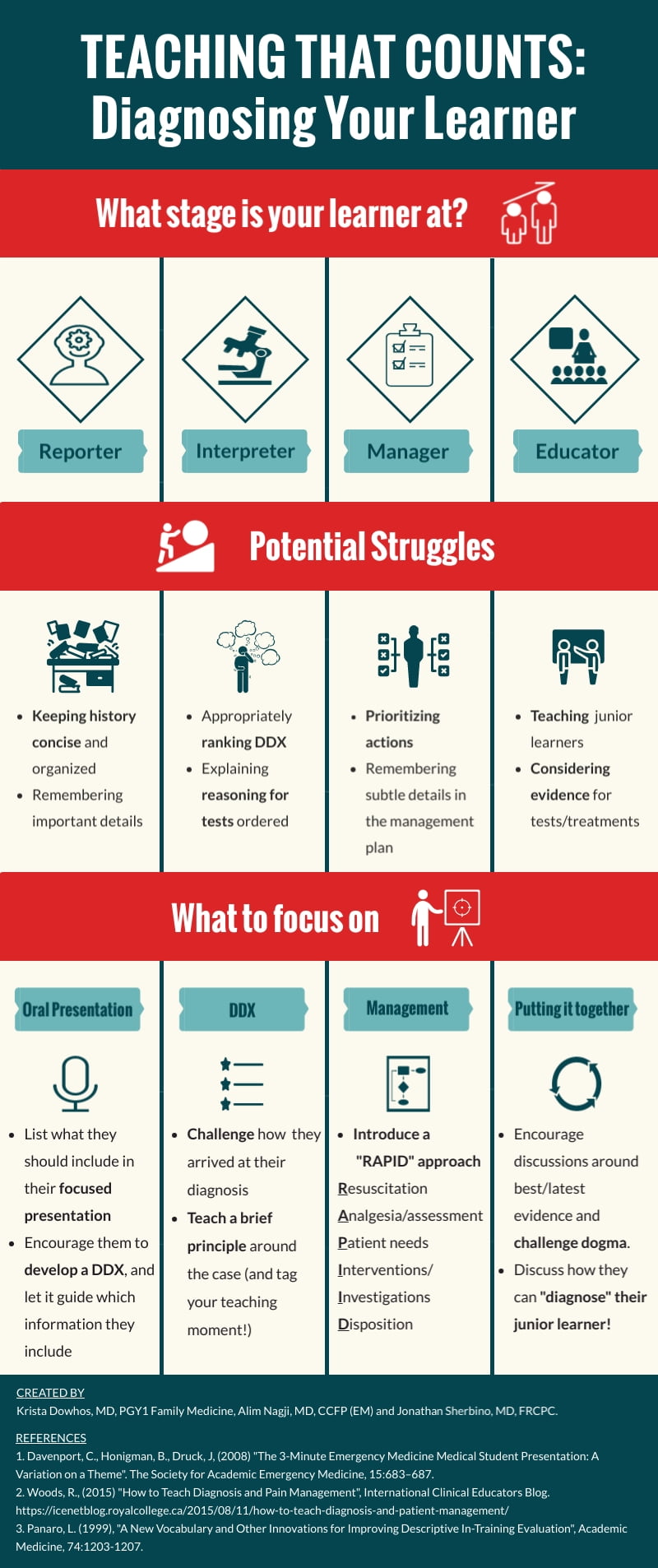
Gone are the days of a “one size fits all” model for assessing and teaching learners in medicine. We know now that learners at different stages in their training learn best from different clinical experiences and different modes of teaching. In our previous infographic “Tailoring Your Teaching to the Individual Learner” we provided you with some basic tips for getting an idea of what your learner knows, what they don’t know, and what they hope to learn so that you can tailor your teaching to their needs. In this infographic we depict the R.I.M.E model, which allows you to diagnose your learner and determine how they will learn best1.
R.I.M.E describes four performance levels existing on a continuum, through which learners progress throughout their training2. Not every learner at a certain training level will perform at the same level on the R.I.M.E continuum. For example, some PGY1s will be performing as a manager, and some will already be performing as an educator. Similarly, an individual learner may perform at different levels on the continuum for different tasks. For example, a 2nd year medical student may be able to perform as an interpreter when assessing an adult with abdominal pain, but is able to perform as a reporter when assessing decreased level of consciousness in an elderly patient. The R.I.M.E model goes beyond the basic questions we ask ourselves and our learner (e.g. “what is their level of training?”, “what would they like to learn today?”) to diagnose your learner and further tailor teaching to their needs.
The Reporter
In this stage, learners are expected to give a history, but may struggle with being concise. Often there is a discrepancy between what you consider useful information to gather from patients, and what information they report. It could be their first time working in the ED, where case presentations differ from those expected during a psychiatry or medicine rotation. It is helpful in these situations to outline what exactly you want from them in a case presentation3. What key features of the history you would like to hear? Roughly how long would you like their presentation to be? Challenge them to use their ideas of what might be going on with a patient to guide the information they include in their presentation.
The Interpreter
At this stage, the learner can formulate differential diagnoses, but their sense of which diagnosis is most likely might be off. Try to understand how they arrived at their diagnosis. For example, ask a question like “what key features in the history do you think increase the likelihood of an MI in this patient”. If they are stuck, teach a brief principle around the case (e.g. features of chest pain that increase the likelihood of ACS), and be sure to tag your teaching moment. An interpreter may also struggle with justifying their choice of investigations. If so, ask them questions like “what would you do if this investigation is abnormal?”, “how will it change the order of your differential diagnosis, if at all?”
The Manager
As a manager, the learner is able to formulate a diagnostic and therapeutic plan for the patients they see. Where they may struggle is prioritizing the actions they take in a patient’s care. For example, treating the patient’s pain prior to ordering investigations. They may overlook or require teaching around subtle details in the management plan. For example, choosing one induction agent over another during RSI. A useful tool to teach learners at this stage is the RAPID checklist4. This mnemonic can assist the learner in considering all aspects of a management plan, from initial resuscitation to disposition. It can decrease their cognitive load so that they don’t overlook the more nuanced aspects of care.
The Educator
If you diagnose the learner at this stage, you can start coaching them to juggle patient care with continuous learning, critical appraisal and teaching. Encourage them to challenge dogma and consider the current evidence for and against choosing investigations and treatments. At this level, you can start teaching the learn how to teach (by sharing this resource with them!).
For further discussion on how to diagnose your learner, listen to the MacEmerg podcast Episode 14!

- 1.Woods R. How to Teach “Diagnosis” and “Patient Management” . ICE Blog. https://icenetblog.royalcollege.ca/2015/08/11/how-to-teach-diagnosis-and-patient-management/. Published August 11, 2015. Accessed January 22, 2020.
- 2.Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Academic Medicine. November 1999:1203-1207. doi:10.1097/00001888-199911000-00012
- 3.Davenport C, Honigman B, Druck J. The 3-Minute Emergency Medicine Medical Student Presentation: A Variation on a Theme. Academic Emergency Medicine. July 2008:683-687. doi:10.1111/j.1553-2712.2008.00145.x
- 4.Woods RA, Trinder K, D’Eon M, McAleer S. Teaching the RAPID approach at the start of emergency medicine clerkship: an evaluation. CJEM. July 2014:273-280. doi:10.2310/8000.2013.131034