You are dispatched to Sam, an 87-year-old who cut the base of his thumb while pitting an avocado approximately 30 minutes ago. The laceration is 3cm long and you can see fatty tissue in the wound. Sam’s wife asks whether you think he will need stitches. You think that he will, but you’ve been wrong in the past, so you’re not sure how to answer her question.
[bg_faq_start]About Sirens to Scrubs
Sirens to Scrubs was created with the goal of helping to bridge the disconnect between pre-hospital and in-hospital care of emergency patients. The series offers in-hospital providers a glimpse into the challenges and scope of practice of out-of-hospital care while providing pre-hospital providers with an opportunity to learn about the diagnostic pathways and ED management of common (or not-so-common) clinical presentations. By opening this dialogue, we hope that these new perspectives will be translated into practice to create a smoother, more efficient, and overall positive transition for patients as they pass through the ED doors.
[bg_faq_end]Objectives:
- Review the practical points of assessment and repair of lacerations.
How do we know if Sam’s cut needs to be closed?
Deciding whether a wound will require sutures (aka stitches) involves consideration of several factors, most important are the age and depth of the wound.1
As a rule, lacerations should be closed when the wound is deep enough to cause excessive or unsightly scarring.3 This usually occurs for lacerations that:
- Are >5mm long
- Are gaping
- Extend through the dermis (which you will know because that’s the layer that contains the blood vessels)
- Can be pulled apart to reveal fat, muscle, tendons or vessels
There are several situations in which wound closure is contraindicated.4 These contraindications mostly relate to infection risk, as closure of a contaminated wound can result in the trapping of pathogens and lead to infection. Examples of wounds that may be at higher risk of infection if closed include:
- Grossly contaminated wounds with foreign debris that cannot be completely removed
- Animal or human bites
- Deep puncture wounds in which the base of the wound cannot be visualized
- Delayed presentations
The goals of wound closure include; achieving hemostasis (stopping the bleeding), avoiding infection (by restoring the protective barrier of the skin), restoring the function of affected tissues (i.e. tendons or ligaments), and achieving an aesthetically pleasing scar.2
How late is too late to close a laceration?
Although specific timelines are disputed, generally, clean wounds can be closed up to 12-18 hours after the injury without an increase in infection risk.4 An exception to this rule is for facial wounds, which can be closed later than the 18-hour window if there are no signs of infection, if the patient is not at an increased risk for infection (i.e. on immunosuppressants), and if the edges can be approximated.3
What are the steps for wound closure?
- Ensure the area distal to the wound is neurovascularly intact by assessing: motor function of each of the muscles one by one, sensation of each of the nerves or nerve branches, and pulse or capillary refill
- Anesthetizing the area, usually by injecting lidocaine into the wound and surrounding tissues. For larger wounds, regional blocks can be used (injecting anesthetic near a nerve or nerve bundle proximal to the wound to block sensation to the skin region innervated by that nerve). Alternatively, topical anesthetics (gels) can be used in children or patients who cannot tolerate injections.1
- The wound is cleaned very well with lots of water or saline and scrubbed with gauze (remember, it’s been frozen already so this is not painful). Iodine solutions, hydrogen peroxide and detergents should not be used for irrigation, as these substances can be toxic to cells and may impair healing.1 After irrigation, any remaining visible foreign matter should be removed from the wound.
- The wound is closed with sutures, staples, tape, or glue.
Are sutures absorbable or do they need to be removed?
Generally, the choice between absorbable and non-absorbable sutures in wound closure is clinically-irrelevant in the ED. The strength of absorbable and non-absorbable sutures is similar, and they also have comparable cosmetic and infection outcomes.5 Absorbable sutures are often used more in children, whereas nonabsorbable sutures may be used more for laceration in areas under greater tension (for example along a joint).
Suture removal: timing of suture removal varies with the site of sutures, ranging from 5 days for the face to up to 14 days over joints.1,3
Will Sam need antibiotics?
Antibiotics are not indicated for all patients with lacerations! There is no evidence to support universal prophylactic antibiotic use for the prevention of infection in individuals who are healthy with minor wounds. However, prophylactic antibiotics may decrease the risk of infection in lacerations resulting from animal and human bites, fractures that break through the skin, wounds that extend into cartilage, joints or tendons, and injuries in the mouth. Some clinicians might supply prophylactic antibiotics for patients with excessive wound contamination, or for those who are immunocompromised.
Tetanus vaccination, on the other hand, must be given to all patients who haven’t been vaccinated recently. Tetanus vaccination will be given to patients unless the most recent of 3 doses is within the last 10 years for clean and minor wounds, or within 5 years for dirty wounds.
What other options does Sam have other than sutures?
Sutures are often chosen over other wound closure methods because they are among the strongest option and allow for the most accurate approximation of wound edges, minimizing the resulting scar.1
There are three common alternatives to sutures: staples, adhesive tapes, or glue. The choice of method takes several factors into consideration, including patient and wound characteristics. In terms of wound characteristics, important considerations for selection of method include amount of tension at the wound, and whether the wound is in a static or dynamic location (i.e. over a joint). If the wound is irregularly-shaped, sutures should be used as they allow for the greatest precision.6 Patient characteristics important to consider include age, ability to access follow-up care, and ability to adhere to treatment protocol.
Staples are quick and easy. However, they do not allow for much precision, so their use is often limited to straight lacerations in areas where cosmesis doesn’t matter. Staples are most often used for scalp lacerations because they do not require cutting the hair and are easier to find for removal compared to sutures. A handheld stapling device is used to set the staples while the edges of the laceration are approximated with forceps.6,7

Adhesive tapes (such as Steri-Strips) are the least invasive and the most cost effective. Their application is easy, quick and painless, and patients can remove the tape themselves. A limitation with adhesive tapes is that they tend to fall off when exposed to tension or moisture, so, their use is often limited to low-tension simple wounds, or closure of fragile skin.6
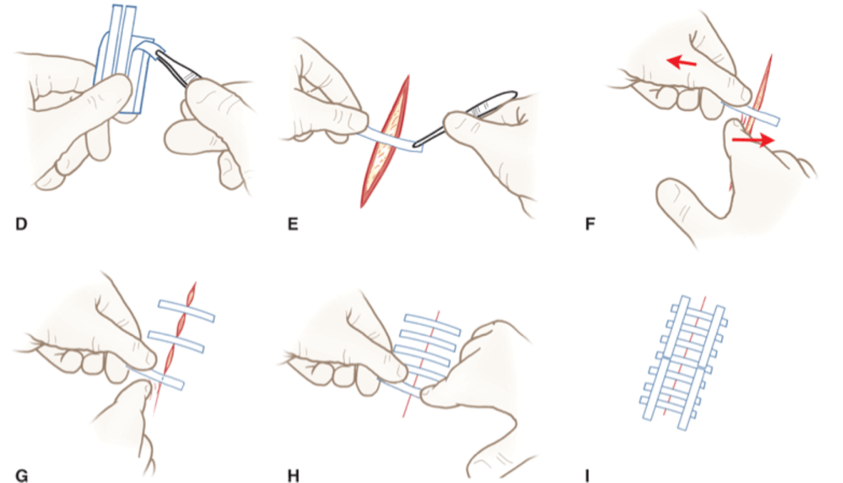
Glue is also quick and easy to apply, and relatively painless for the patient. They can be used for wounds <5cm that are not under tension and where the edges of the laceration are easy to bring together. They serve as a barrier to bacterial infiltration, and the adhesive sloughs off within 5-10 days. However, they are the weakest of the wound closure methods, and thus should not be used for lacerations under high tension, or in very dynamic locations (i.e. over a joint). The glue should cover the entire wound, and 5-10mm on either side of the wound edges.6

Table 1: Comparing wound closure methods6
| Technique | Ease of use | Speed | Requires anesthesia? | Advantages | Disadvantages |
| Sutures | Technically challenging | Time consuming | Yes | Most precise and least likely for the laceration to come apart before it heals | May require removal Greatest tissue reactivity Outcomes are provider-dependent Risk of needlestick injury |
| Staples | Relatively simple | Rapid | Yes | Low tissue reactivity | Requires removal Less meticulous closure Interferes with MRI/CT imaging |
| Steri-Strips | Simple | Rapid | No | Lowest infection rates No need for removal | Weak closure and the tape frequently falls off before the wound is closed. Both of these factors may cause the laceration to re-open Cannot be used around areas with hair Cannot get wet |
| Glue | Simple | Rapid | No | Resistant to bacterial growth No need for removal | Weak closure may cause the laceration to re-open Cannot get wet |
Case resolution
The emergency doctor decides that Sam’s laceration needs to be closed. There’s no tendon or nerve damage found on testing, so the wound is anesthetized, cleaned well, and sutured closed. He is advised to follow-up with his family physician in one week to have his sutures removed, and to see a physician sooner should he develop infection (the wound becomes red, hot, more painful rather than less painful, pus is seen at the wound, or he becomes systemically unwell with fevers/chills). He is also given a tetanus booster shot as he can’t recall his last one.
Authored by @MonBilic and edited by @SneathPaula
- 1.Forsch RT. Essentials of Skin Laceration Repair. American Family Physician. https://www.aafp.org/afp/2008/1015/p945.html. Published 2008.
- 2.Capellan O, Hollander JE. Management of lacerations in the emergency department. Emergency Medicine Clinics of North America. February 2003:205-231. doi:10.1016/s0733-8627(02)00087-1
- 3.deLemos DM. Closure of minor skin wounds with sutures. UpToDate. https://www.uptodate.com/contents/closure-of-minor-skin-wounds-with-sutures?search=closure%20of%20minor%20wounds%20with%20sutures&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H44. Published June 23, 2019. Accessed November 10, 2019.
- 4.Hollander J, Singer A. Laceration management. Ann Emerg Med. 1999;34(3):356-367. doi:10.1016/s0196-0644(99)70131-9
- 5.Holger J, Wandersee S, Hale D. Cosmetic outcomes of facial lacerations repaired with tissue-adhesive, absorbable, and nonabsorbable sutures. Am J Emerg Med. 2004;22(4):254-257. doi:10.1016/j.ajem.2004.02.009
- 6.Hollander J, Singer A. Laceration management. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. McGraw-Hill Education; 2016:268-281.
- 7.Iavazzo C, Gkegkes I, Vouloumanou E, Mamais I, Peppas G, Falagas M. Sutures versus staples for the management of surgical wounds: a meta-analysis of randomized controlled trials. Am Surg. 2011;77(9):1206-1221. https://www.ncbi.nlm.nih.gov/pubmed/21944632.

