Does that condition really require investigation? Recognizing the Tragedy of the Commons in healthcare, we need to improve resource utilization. This post examines five commonly performed investigations (CT in head injury, CXR in chest pain, and investigations in Syncope/AFib/Renal Colic) in the Emergency Department (ED) to determine if the evidence exists to support current practice patterns.
[bg_faq_start]Minimal / Minor Head Injury: Does it require investigation?
The vast majority of literature examining the utilization of imaging in patients with head injury is focused on patients with minor head injury [1].
Minor head injury is defined as a loss of consciousness, definite amnesia or witnessed disorientation in patients’ with a GCS 13-15.
In all cases of head trauma, it is the role of the ED physician to rule out intracranial pathology. Fortunately, the Canadian CT Head Rules (CCHR) helps to provide further clarification on who requires neuroimaging in patients with minor head injury [1]. Notably, the vast majority of patients presenting to the ED after head injury do not meet the inclusion criteria for minor head injury, but rather, have suffered a minimal head injury.

Canadian CT Head Rule
The CCHR has a sensitivity of 100% and specificity of 68.7% to identify patients requiring neurosurgical intervention following minor head injury. While it was anticipated that neuroimaging would decrease following implementation, a multicentre prospective implementation study found that imaging actually increased from 63-68% to 74-76%, despite adequate promotion and education of the decision aid [2].
So what gives? Why so many more scans, despite a decision rule providing us with the utility to decrease imaging? A number of studies have evaluated this, but physician practice habits are difficult to study, however, it appears that the CCHR are being erroneously applied to patients with minimal head injury, or that features from the CCHR are being inappropriately incorporated into physician “gestalt”.
There are no decision rules to help us with what to do with minimal head injury patients. Fortunately, the vast majority of minimal head injury patients are unlikely to have pathology, so it is important to determine which high risk patients do require further investigation.

Minimal Head Injury
One of the largest studies on patients with minimal head injury was a prospective cohort study on over 1100 patients following head injury, and they found that [3] :
- Without any risk factors present
- 1.8% had an intracranial finding
- 0.4% required neurosurgical intervention
- With risk factors present*:
- 5% had an intracranial finding
- 0% required neurosurgical intervention
*Risk factors [4]:
- Persistent nausea and vomiting
- Suspected child/elder abuse
- Seizure
- Palpable depressed skull fracture
- Anticoagulation or bleeding diasthasis
- Age <2 or >65 WITH severe headache, nausea/vomiting
- Extracranial injuries that alone require admission
The authors ultimately concluded that a minority of patients with minimal head injury will have pathology, and that there is clearly a need for guidelines to help minimize the over-utilization of imaging in these patients.
Scandinavian Guidelines
Since then, only guidelines created to help us in the management of the patient with minimal head injury come from the working group that created the Scandinavian Guidelines [5,6]. A robust systematic review led the working group to recommend:
“that adult patients after minimal and mild head injury with GCS 15 and without risk factors (loss of consciousness, repeated (≥2) vomiting, anticoagulation therapy or coagulation disorders, post- traumatic seizures, clinical signs of depressed or basal skull fracture, focal neurological deficits) can be discharged from the hospital without a CT scan (moderate quality, strong recommendation).” [5]
These guidelines have subsequently undergone an validation study at 6 ED’s in New York/Pennsylvania in the form of an retrospective nested cohort study, and found that in 662 patients presenting with head injury, 93 met their inclusion criteria for minimal head injury without risk factors and 0% of patients had findings on CT head [6].
Bottom Line:
Ultimately, it appears that patients without significant neurological risk factors and minimal head injury are unlikely to have significant pathology, so do not likely require neuroimaging. However, the more important point is to remember not to erroneously apply the Canadian CT Head Rule to these patients. The individual who falls down and hits their head, but doesn’t lose consciousness, is fully alert/with a normal neurological exam, and no other complaints is unlikely to have significant pathology. To help develop a more conservative imaging strategy, the utilization of these high risk features may help you determine who ultimately requires further imaging.
What if the patient is anticoagulated?
In the majority of studies looking at head injury, patients are typically excluded if they are anticoagulated or have a bleeding diathesis, so these patients can present a diagnostic dilemma when presenting with minor or minimal head injury. In one historical cohort study over two years, patients were included if they had minor head injury or minimal head injury in the setting of anticoagulation use with a primary outcome of intracranial bleeding. They excluded any patients with an INR < 1.5, penetrating injuries or with a focal neurological deficit [8].
Of 176 patients enrolled, 89.2% had a CT head, and of these 15.9% had an intracranial bleed.
- 21.9% of the minor head injury group had intracranial bleeding
- 4.8% of the minimal head injury group had a rate of bleeding
This evidence suggests that anticoagulated patients, even with minimal head trauma, can have significant morbidity and mortality, and correlates well to existing literature on the topic [9,10]. We should maintain a low threshold for neuroimaging in these patients. It should also be noted that patients on plavix also have an elevated bleeding risk, and we should maintain caution around these patients with head injury [11].
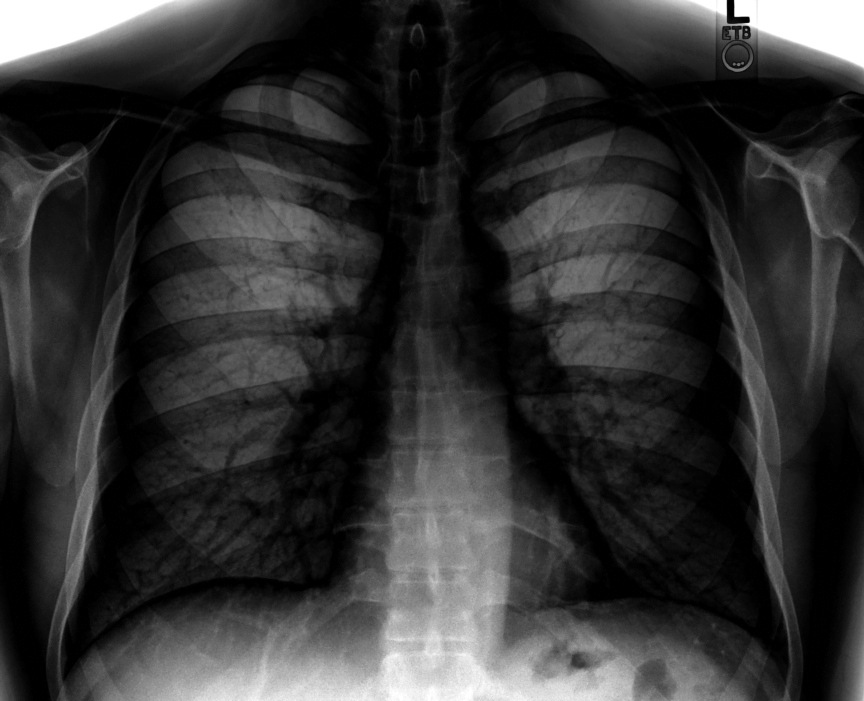
[bg_faq_end][bg_faq_start]Chest pain: Does it require a CXR?
Patients’ presenting to the ED with chest pain often undergo chest radiography. However, there is surprisingly little data supporting this. The data available found that consistently low proportions (2-6%) of CXR’s have clinically significant pathology in chest pain patients, yet CXR’s represent about 50% of diagnostic studies performed in the ED [12-15].
Patients who do have pathology are typically [13]:
- Older
- Have chest pain with associated shortness of breath
- Significant past medical history
- Tachypneic
Based on this, a decision rule was derived to help determine which patients do not require CXR’s when presenting with chest pain [14]. This derivation paper found that only 2.1% of patients presenting to the ED had CXR’s with clinically relevant pathology, and that the decision rule identified these patients with a sensitivity of 100% and specificity of 36.1%, allowing us to forgo imaging in an significant number of patients. Unfortunately, this decision rule subsequently failed validation and the amended rule derived from the validation cohort lacked the specificity to be recommend for implementation. However, once again the small proportion (6%) of patients with abnormal CXR’s requiring intervention were older, had shortness of breath/tachypnia, and had a significant past medical history [16]. The validation paper likely had a higher rate of pathology, as it was conducted at the Mayo clinic, which tends to see patients with a higher degree of comorbid conditions. Additionally, examining “clinically relevant” outcomes in these studies, it is not clear that many outcomes were very significant. For example, many of the suggested CXR findings were ‘pulmonary edema’, which is arguably a clinical diagnosis, and when not suspected clinically – is probably not an significant finding.

If there are clinical concerns of pneumonia/effusion/pulmonary edema in a chest pain patient, then they certainly require an CXR. However, those conditions diagnosed on CXR can be diagnosed in other ways as well. Pulmonary edema is typically a clinical diagnosis, and emerging literature suggests that PoCUS is highly sensitive for aiding in this diagnosis. Additionally, PoCUS has been demonstrated to be highly sensitive for detecting pneumothorax.
[bg_faq_end][bg_faq_start]Ultimately, CXR should be restricted to patients’ in which there is a particular clinical question that the X-Ray may answer, and should not be used as a screening test.
Syncope: Does it require investigation?

The vast majority of literature and recommendations on syncope in this post, are based upon the well patient who has a syncopal event and is now well again. The differential diagnosis in this scenario is actually fairly limited, as there are not many things that do this beyond cardiac and vasovagal syncope (and potentially GI bleeding, but historical features will aid you there).
CT Head
In a prospective study across 6 Canadian tertiary ED’s, adult patients with syncope were analyzed for a primary outcome of clinically important and new findings on CT head. Over 1000 patients were included, with a mean age of 63 and a fairly standard distribution of medical cormorbidities [17].
Within this cohort, only 3.4% of patients had the primary outcome of a new or clinically important finding on CT head, and these patients had; elevated INR, low GCS or head injury. It should therefore, not be surprising that ACEP also does not recommend CT head in asymptomatic syncope patients without trauma and a normal neurological exam [18].

Investigations
The literature on investigations in syncope is fairly sparse, but from what currently exists it appears that the yield in the workup of syncope patients is quite low (collated from a few studies) [19,21]:
- Blood work: 4.5%
- ECG: 4-6.7%
- CXR: 0%
- Holter monitoring: 1-16%
- Troponin: 0.6-0.62%
* It is important to note that this is the yield of these investigations contributing to a diagnosis in all syncope patients, not just those that have a syncopal episode, and are well again.
One study did isolate a potential ‘low risk cohort’ (age <50, with a vasocagal predisposition and no known cardiac disease), and found that the above investigations did not contribute to the diagnosis in any of these patients [21]. Subsequently, it seems that there is low potential yield of investigations in patients with syncope, and those with positive results are not likely to be well afterwards, or will have significant medical comorbidities.

There have been a multitude of decision rules released to help us in our approach to the patient with syncope, however, the vast majority of these have had significant issues associated with their potential use, and have therefore not been widely disseminated.
- San Francisco Syncope Rule (SFSR): Examined the prediction of serious adverse events (SAE’s) but performed poorly on external validation.
- Risk Stratification of Syncope (ROSE): Predicted SAE at 30 days, but performed sub-optimally on external validation and requires the utilization of BNP.
- Short term Prognosis in Syncope (StEPS): identified risk factors for death and therapeautic interventions at 10 days, but predictors of concomitant trauma and male sex make it fairly impractical to use.
- Boston Syncope Criteria: A long list of 25 plausable predictors for SAE makes it fairly impractical to use in clinical practice.
- Anatolian Rule: 39 SAE predictors, again, making it fairly impractical to use.
So… is there anything we can use? On an recent edition of EMRAP (Canadian edition) Dr. Thiruganasambandamoorthy discusses the recent acceptance of his paper on the ‘Canadian Syncope Risk Score’. In brief, this multi-centre, prospective cohort study enrolled over 4000 adult patients with a primary outcome of serious adverse events at 30-days and created a risk score. They ultimately identified that a vasovagal predisposition was negatively associated with SAE; supporting what has previously been demonstrated in the literature (stay tuned for more specifics upon publication!).
Bottom Line:
In the well patient who has syncope and is well again, with a vasovagal predisposition (or where the ED physician suspects the diagnosis is vasovagal syncope), the only diagnostic requirement is an ECG. If these are normal no further investigation is required.
Atrial Fibrillation: Does it require investigation?
In Canada, patients often present to the ED with recurrent exacerbation of pre-existing atrial fibrillation, undergo cardioversion, and are discharged home. However, the majority of these patients have imaging or blood work, resulting in prolonged ED stays and increased resource utilization. International guidelines do not specify what testing should be performed during ED evaluations for patients presenting with these exacerbations. So, what does the evidence say about workups for patients who are having recurrence of known (and previously investigated) paroxysmal atrial fibrillation?
Labs
There is a paucity of evidence in the literature examining this question but bloodwork does not seem to add to the management of these patients. A prospective cohort study evaluating atrial fibrillation patients presenting to the ED [20] found that 0% of patients with recurrent atrial fibrillation requiring cardioversion had clinically significant findings (CBC, electrolytes, troponin, CXR). This helps give credence to similar evidence that has suggested a low yield of investigations in patients previously worked up, presenting with a symptomatic exacerbation of their paroxysmal atrial fibrillation [20,21].
Given these findings, the utility of investigations in atrial fibrillation seems to be limited in those presenting with an exacerbation of known symptomatic paroxysmal atrial fibrillation.
What about troponin?
Perhaps the most important consideration in the workup of atrial fibrillation is frequent ordering of cardiac enzymes. The unnecessary use of cardiac markers in patients with atrial fibrillation may contribute to increased resource utilization, prolonged ED stays and unwarranted cardiac investigations for positive enzymes of unknown significance [22,23].
In a retrospective chart review examining patients with atrial fibrillation presenting to the ED [24] 13.7% had a positive troponin and 4.9% were treated as ACS. Notably, all of the patient’s treated as ACS had chest pain.
A subsequent prospective cohort study performed in the United States for atrial fibrillation patients admitted to ‘Rule out MI’ found that [25] 5.5% of patients were diagnosed with ACS and 100% of these patients had chest pain and 100% of these patients had ST elevation or depression >2 mm.
Given this literature, the use of troponin in patients with known paroxysmal atrial fibrillation in patients who do not have chest pain or ischemic ECG changes is questionable.

Bottom line
In patients’ with uncomplicated recurrence of atrial fibrillation requiring cardioversion (having had previous investigations and workup for this condition) the only investigations that are required are pre and post-cardioversion ECGs. Additionally, in the absence of chest pain, there is no role for cardiac enzymes in these patients.
Renal Colic: Does it require investigation?
Renal colic patients are common place in the ED, frequently undergo ultrasound or CT imaging – resulting in prolonged ED stays, significant radiation and exposures, and often undergo multiple scans as a result of their disease process.
CT:
In a large retrospective chart review adults with a presentation suggestive of renal colic were evaluated to examine CT utilization in this group [26]. A total of 356 patients were enrolled, with 74% of patients undergoing CT examination. Within this cohort, 38% of patients had normal imaging, 58% demonstrating urolithiasis and only 2% had an urgent or emergent cause of symptoms identified. The scope of this study was over a span of ten months, and during this time 79% of patients had two or more CT scans.
Another study examined whether repeated CT scanning subsequently changes diagnosis in patients presenting with renal colic, and they ultimately found that only 6.5% of patients had an alternative diagnosis identified as a result of repeat CT with a past history of renal colic demonstrated on imaging [27]. The majority of these diagnosis (chole, AAA, appendicitis) were suspected clinically prior to the CT being performed.
Who should get imaging?
Patients should get imaging for their first presentation of suspected renal colic because alternative diagnoses are identified in 33.1% of these patients (47% of which are clinically significant and 9% which change management). Similarly, it is reasonable to image those with diagnostic uncertainty, or potential alternative pathology.[28]
Given the low utility of repeat CT scans in patients with known/documented renal colic, ACEP has proposed the following as a Choosing Wisely guideline:

Bottom line
Healthy patients under the age of 50, with a known history of renal colic and an uncomplicated presentation of renal colic (no pyuria, fever, intractable pain, no solitary kidney, baseline creatinine, no past history of obstructive stone) do not require imaging in the ED. PoCUS or outpatient ultrasound to risk stratify for hydronephrosis is entirely appropriate.
References
- Stiell I, Wells G, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357(9266):1391-1396.
- Stiell I, Clement C, Grimshaw J, et al. A prospective cluster-randomized trial to implement the Canadian CT Head Rule in emergency departments. CMAJ. 2010;182(14):1527-1532.
- Ibañez J, Arikan F, Pedraza S, et al. Reliability of clinical guidelines in the detection of patients at risk following mild head injury: results of a prospective study. J Neurosurg. 2004;100(5):825-834.
- Stein S, Spettell C. The Head Injury Severity Scale (HISS): a practical classification of closed-head injury. Brain Inj. 1995;9(5):437-444.
- Undén J, Ingebrigtsen T, Romner B, Scandinavian N. Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults: an evidence and consensus-based update. BMC Med. 2013;11:50.
- Undén L, Calcagnile O, Undén J, Reinstrup P, Bazarian J. Validation of the Scandinavian guidelines for initial management of minimal, mild and moderate traumatic brain injury in adults. BMC Med. 2015;13:292.
- Easter J, Haukoos J, Claud J, et al. Traumatic intracranial injury in intoxicated patients with minor head trauma. Acad Emerg Med. 2013;20(8):753-760.
- Alrajhi K, Perry J, Forster A. Intracranial bleeds after minor and minimal head injury in patients on warfarin. J Emerg Med. 2015;48(2):137-142.
- Brewer E, Reznikov B, Liberman R, et al. Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. J Trauma. 2011;70(1):E1-5.
- Inui T, Parina R, Chang D, Inui T, Coimbra R. Mortality after ground-level fall in the elderly patient taking oral anticoagulation for atrial fibrillation/flutter: a long-term analysis of risk versus benefit. J Trauma Acute Care Surg. 2014;76(3):642-9-50.
- Nishijima D, Offerman S, Ballard D, et al. Immediate and delayed traumatic intracranial hemorrhage in patients with head trauma and preinjury warfarin or clopidogrel use. Ann Emerg Med. 2012;59(6):460-8-7.
- Ng J, Taylor D. Routine chest radiography in uncomplicated suspected acute coronary syndrome rarely yields significant pathology. Emerg Med J. 2008;25(12):807-810.
- Al Z, Al-Senawi R, Al R, Al-Zakwani I, Nemeth J, Perry J. Predictors of positive chest radiography in non-traumatic chest pain in the emergency department. Oman Med J. 2009;24(1):22-26.
- Hess E, Perry J, Ladouceur P, Wells G, Stiell I. Derivation of a clinical decision rule for chest radiography in emergency department patients with chest pain and possible acute coronary syndrome. CJEM. 2010;12(2):128-134.
- van W, Langhout M, Ly F, et al. Diagnostic performance and comparative cost-effectiveness of non-invasive imaging tests in patients presenting with chronic stable chest pain with suspected coronary artery disease: a systematic overview. Curr Cardiol Rep. 2014;16(10):537.
- Poku J, Bellamkonda-Athmaram V, Bellolio M, Nestler D, Stiell I, Hess E. Failure of prospective validation and derivation of a refined clinical decision rule for chest radiography in emergency department patients with chest pain and possible acute coronary syndrome. Acad Emerg Med. 2012;19(9):E1004-10.
- Viau A, Mukarram M, Arcot K, Soo-Min K, Thiruganasambandamoorthy V. Yield of Computed Tomography of the Head Among Adult Emergency Department Syncope Patients: A Prospective Cohort Study.
- Langer-Gould A, Anderson W, Armstrong M, et al. The American Academy of Neurology’s top five choosing wisely recommendations. Neurology. 2013;81(11):1004-1011.
- Vanbrabant P, Van O, Knockaert D, Gillet J. Diagnostic yield of syncope investigation (initiated) in the emergency department: a pilot study. Acta Clin Belg. 2011;66(2):110-115.
- Barrett T, Abraham R, Self W. Usefulness of a low CHADS2 or CHA2DS2-VASc score to predict normal diagnostic testing in emergency department patients with an acute exacerbation of previously diagnosed atrial fibrillation. Am J Cardiol. 2014;113(10):1668-1673.
- Johnson P, Ammar H, Zohdy W, Fouda R, Govindu R. Yield of diagnostic tests and its impact on cost in adult patients with syncope presenting to a community hospital. South Med J. 2014;107(11):707-714.
- Ng S, Krishnaswamy P, Morrisey R, Clopton P, Fitzgerald R, Maisel A. Mitigation of the clinical significance of spurious elevations of cardiac troponin I in settings of coronary ischemia using serial testing of multiple cardiac markers. Am J Cardiol. 2001;87(8):994-9; A4.
- Gupta S, de L. Use and misuse of cardiac troponins in clinical practice. Prog Cardiovasc Dis. 2007;50(2):151-165.
- Meshkat N, Austin E, Moineddin R, et al. Troponin utilization in patients presenting with atrial fibrillation/flutter to the emergency department: retrospective chart review. Int J Emerg Med. 2011;4(1):25.
- Zimetbaum P, Josephson M, McDonald M, et al. Incidence and predictors of myocardial infarction among patients with atrial fibrillation. J Am Coll Cardiol. 2000;36(4):1223-1227.
- Broder J, Bowen J, Lohr J, Babcock A, Yoon J. Cumulative CT exposures in emergency department patients evaluated for suspected renal colic. J Emerg Med. 2007;33(2):161-168.
- Goldstone A, Bushnell A. Does diagnosis change as a result of repeat renal colic computed tomography scan in patients with a history of kidney stones? Am J Emerg Med. 2010;28(3):291-295.
- Ha M, MacDonald R. Impact of CT scan in patients with first episode of suspected nephrolithiasis. J Emerg Med. 2004;27(3):225-231.
Reviewing with Staff
Modern medicine’s overdependence and overemphasis on testing is clearly very profound and constantly reinforced in various ways, both subtle and not so subtle. In particular, trainees in academic centres witness this excessive testing and are very likely to incorporate that approach in their own practice and propagate over-testing for the rest of their career. The bottom line is that - for a long list of reasons - doctors love tests, but the dirty secret is that we often don’t fully understand the properties of these tests very well and therefore are likely to erroneously use them, at least part of the time.
So what’s the harm? There is well-documented evidence that over-testing and overtreatment can be harmful, both at the individual patient level and at the system level. Harm can occur at three levels and in many instances is subtle and difficult to quantify, yet very real:
1) Individual patient harm – radiation risk, complications from IV contrast, increased downstream testing of incidental findings, psychological harm from incidental findings, over-treatment of clinically unimportant findings (ie isolated subsegmental PEs)
2) Harm to the ED environment – crowding is an ever-present reality. Ordering unnecessary tests increases that crowding by prolonging ED stays by hours for our patients who otherwise could be discharged home and free up beds and nursing resources for new patients, as well as shorten the diagnostic imaging queues for those patients who actually need imaging. The resultant delays to care for other patients potentially leads to poorer outcomes for some of them, yet are difficult for individual physicians to detect on their shift. While a physician might feel that, with their thoroughness, they have done their duty for the patient who is in front of them, they probably do not fully appreciate the potential trade-off that is created … the resultant bed blocking and diversion of resources might leave an untreated patient in the waiting room for longer periods of time, potentially increasing their morbidity.
3) Harm to the entire health care system – So far, physicians have had unfettered and unlimited access to most testing without having to justify their decisions. That lack of accountability to the health care system, with its finite and limited resources, seems rather preposterous. Physicians have a responsibility to taxpayers to be judicious guardians of the trust that has been bestowed upon us. Unnecessary use of testing prolongs wait times for those who actually do need the services and diverts finite resources from another area which might otherwise yield a higher benefit.
In this post, Dr. Syed explores five specific scenarios where there is clear over-testing in our EDs. Physicians can feel comfortable incorporating the advice given in the post as much of it is well supported by published evidence and has face validity. By adopting these practice suggestions, we are taking necessary and important baby steps to combat the culture of reflexive testing without clear rationale, with its myriad of negative effects and to re-establish our responsibility to our EDs and to the health care system as a whole.