This updated episode of CRACKCast covers Rosen’s Chapter 34 (9th Ed.) on head trauma. This episode will outline the approach and details of the diagnosis and treatment for patients with Traumatic Brain Injuries. We also cover return to play guidelines for athletes.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective:
Head trauma is a relatively common and important clinical presentation that we see in the Emergency department. In the US, this accounts for approximately 1.5 million ED visits per year. TBI can be classified into mild, moderate and severe categories. Clinical presentations range from well patients with minor bumps, to critically injured multi trauma patients. A detailed knowledge of the TBI spectrum, as well as the management principles for the key injuries associated with TBI, are key. So sit back, grab a coffee or put on your running shoes, and get ready for a whirlwind tour through Chapter 34 – head trauma.
[bg_faq_end]Core Questions:
[bg_faq_start][1] Define Mild, Moderate and Severe TBI
- Severe: Post resuscitation GCS of 8 or lower
- Moderate = GCS 9-12
- Mild = GCS 13-15 with one of the following 4 manifestations of traumatic disruption of brain function
- Any period of LOC <30 min
- Amnesia immediately before or after the incident (post traumatic amnesia should last for <24h)
- Alteration in mental state at the time of the accident (ex. dazed, disoriented, confused).
- Focal neurologic deficits that may or may not be transient
This list was informed by Table 34.1 in Rosen’s 9th Edition. Refer to the text for further information.
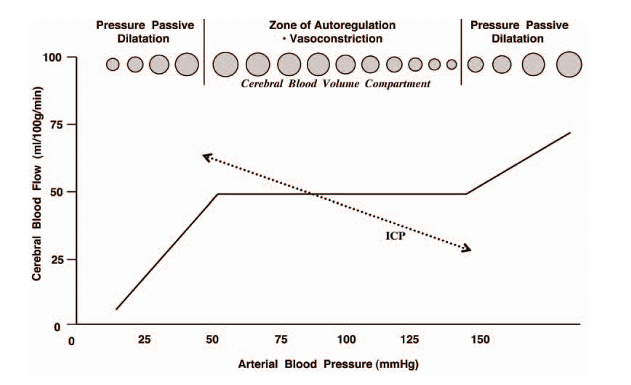
[2] Explain the concepts of cerebral autoregulation and CPP. Why is this clinically relevant?
A few equations first:
1. CPP = MAP – ICP
2. CBF = CPP/CVR
3. They can also be combined: CBF = CPP/CVR = (MAP – ICP)/CVR
Where CPP = cerebral perfusion pressure, CBF = cerebral blood flow, MAP = mean arterial pressure, ICP = intracranial pressure, and CVR = cerebrovascular resistance.
Remember the following factors:
a. Hypertension, alkalosis and hypocarbia promote cerebral vasoconstriction
b. Hypotension, acidosis, and hypercarbia cause cerebral vasodilation
c. Between PCO2 of 20-60, lowering PCO2 by 1mmHg transiently decreases the diameter of cerebral vessels by 2-3% (thus PCO2 is the single largest immediate contributing factor to CBF)
Conceptually, CPP describes the pressure gradient across the brain. CBF closely follows CPP in a brain that has normal autoregulation, which is the ability of the cerebral vasculature to maintain stable blood flow despite changes in CPP/MAP. This ranges between a MAP of 60-150mmHg. In an injured brain, ICP effects become important, and autoregulation can start to fail. If CPP falls below 40mmg, autoregulation is lost and causes tissue ischemia. Autoregulation also fails in the setting of severe hypo or hypertension. Rosen’s recommends a CPP target of 60-70mmHg in head injured patients.
The relationship between MAP, CBF, and cerebral vasodilation and vasoconstriction is worth taking a bit of time to go over. In a brain that can autoregulate, increases in MAP will directly cause vasoconstriction in the cerebral vascular bed, and will lead to a corresponding decrease in ICP. This response is lost below a MAP of 50 or greater than 150. These concepts explain why transiently hyperventilating the patient or increasing the MAP can both quickly lower the ICP.
[3] Differentiate between: Primary vs Secondary brain injury, and Direct vs Indirect brain injury
A. Primary vs Secondary
Primary brain injury is the mechanical damage that occurs at the time of head trauma and includes lacerations, hemorrhage, contusion and tissue avulsion. At the tissue level, mechanical cellular disruption and microvascular injury occurs. There is no intervention to repair the cellular damage caused by primary brain injury.
Secondary brain injury occurs after the primary insult, creates further damage to brain tissue and worsens outcomes of TBI. Preventing secondary brain injury is the key goal of emergency care of the head injured patient. These conditions include:
- Hypotension (associated with near doubled mortality rate)
- Hypoxia (doubles mortality)
- Hypocarbia and hypercarbia
- Anemia
- Hyperpyrexia (core body temp >38.5)
B. Direct vs. indirect brain injury
Direct head trauma occurs when the head is struck, or its motion is arrested by an object. Compression is another mechanism of direct injury. Consistency, mass, surface area and velocity of the object striking the head determine the degree of injury.
Indirect brain injury occurs when the brain is set into motion by something other than direct contact of the skull with another object. This includes acceleration-deceleration type injuries. This can cause shearing forces between cranial contents, resulting in injuries that range from concussion to SDH and DAI. Contrecoup injuries/concussions are caused by this mechanism.
[4] Describe the 4 herniation syndromes
- Uncal herniation – the uncus (anteromedial temporal lobe) herniates into the tentorial notch, compressing CN III and then the brainstem. Findings can include ipsilateral blown pupil, decreased consciousness, and contraleteral hemiparesis.
- Tonsillar herniation – posterior fossa herniation whereby the cerebellar tonsils herniate through the foramen magnum. Presents with irregular breathing, cardiac (bradycardia) and hypertension.
- Upward transtentorial herniation – occurs as a result of expanding posterior fossa lesion. Presents with decreased LOC, pinpoint pupils (compression of pons) and downward gaze.
- Central transtentorial herniation – caused by bilateral central pressure on the brain exerted by an expanding lesion at the vertex, frontal or occipital pole of the brain. Clinical manifestations include depressed LOC, bilateral weakness, and pinpoint pupils. As a result, pupils become midpoint and fixed, respiration is affected, and decorticate posturing may be observed.

[5] List the extra-axial brain injuries
- EDH – Epidural hemorrhage is bleeding between the inner layer of the skull and the outer dura. Usually caused by direct blow, often by a fracture overlying the site of the middle meningeal artery. EDH typically has a lentiform appearance on CT and is characterized by a lucid interval followed by rapid LOC.
- SDH – Subdural hemorrhage is bleeding between the dura and brain, usually caused by acceleration/deceleration injuries that injure bridging vessels. Brain atrophy, such as seen with elderly patients or alcoholics, is a risk factor for increased shearing force and injury to bridging vessels. These typically have a crescent-shaped appearance that spreads diffusely over the affected hemisphere.
- SAH – Subarachnoid hemorrhage is caused by bleeding with the CSF and meningeal intima; likely caused by tears of small subarachnoid vessels. This is the most common CT abnormality in head trauma (50%).
- Subdural Hygroma – Collection of xanthochromic fluid in the dural space. Uncertain cause, thought to be due to a tear the arachnoid membrane that allows CSF to escape.
[6] List the intra-axial brain injuries
- DAI and TAI (diffuse and traumatic axonal injury): Per Rosen’s, DAI is to be used in severe cases, and TAI for less severe cases. Axons are torn or stretched, leading to axonal swelling, disconnection and cell death. Clinically, this presents with persistent coma/LOC post trauma. Initial imaging may be normal, therefore MRI may be required for further characterization.
- Cerebral contusion: A bruise on the surface of the brain, typically caused by impact injury. Typical sites include the poles and inferior surfaces of frontal and temporal lobes as this is where the brain comes into contact with the bony prominences at the base of the skull.
- ICH (intracerebral hematoma): This is hemorrhage deep within the brain tissue usually caused by shearing or tensile forces that injure deep arterioles.
- Intracerebellar hematoma: Rare, typically occurs with a direct blow to the occipital area.
[7] Outline your approach to clinical assessment of a patient with a brain injury (including GCS and brainstem reflexes)
- Primary survey to address life threats
- Pupils, GCS, and gross motor movements assessed as part of “disability”
- Do not forget C spine precautions – concurrent C spine injury in up to 20% of severely head injured patients
- Secondary survey to evaluate for signs of head and neck trauma
- Scalp lacerations/contusions or hematomas may mask depressed skull fractures
- Examine for signs of basilar skull fractures including:
- Hemotympanum
- Blood in ear canal
- CSF rhinorrhea/otorrhea
- Battle’s sign (retro-auricular hematoma)
- Raccoon eyes (periorbital ecchymosis)
- Cranial nerve deficits
- Facial paralysis
- Decreased auditory acuity
- Dizziness
- Tinnitus
- Nystagmus
- Neurologic assessment
- Pupils
- Bilateral or fixed – central or upwards herniation. Consider toxicologic differential diagnosis as well (ex. Opiates or stimulants).
- Unilateral mydriatic pupil – traumatic mydriasis, impending uncal herniation, traumatic dissection
- Unilateral miotic pupil – traumatic Horner’s, iritis
- GCS
- Motor exam
- Traditionally – bulk, tone, strength, reflexes. Typically requires a cooperative patient.
- Decorticate posturing = flexion upper extremity, extension lower extremity (plantar flexion of foot). Signifies midbrain injury
- Decerebrate posturing = extension/adduction of arms with wrist flexion, internal rotation, flexion of neck, internal rotation/extension of lower extremities. Signifies caudal/brainstem injury.
- Brainstem exam
- Respiratory pattern
- Pupils
- Oculocephalic (doll’s eyes) maneuver to test integrity of pontine gaze centres. Rule out C spine injury first
- Oculovestibular response – assess with cold calorics (comatose patients no longer demonstrate nystagmus or tonic deviation of eyes toward noxious stimulus when cold water placed in ear canal). Ensure patent auditory canal
- +/- Gag (IX/X), facial symmetry (VII), corneal reflex (CN V/VII)
- Pupils
[8] Describe key imaging findings in the main types of traumatic brain injury
CT is the diagnostic standard for ED. Skull radiography is not useful for TBI assessment.
- Pneumocephalus – penetrating wound. Per Rosen’s: “All tangential GSWs should be evaluated with head CT secondary to the high incidence of intracranial injury”
- EDH – hyperdense, biconvex ovoid and lenticular density, with sharp margins. Does not cross suture lines. Typically located in temporoparietal region (5% in posterior fossa)
- SDH – crescentic hyperdensity that crosses suture lines and follows the contour of the tentorium
- SAH – increased density within basilar cisterns, interhemispheric fissures and sulci
- Subdural hygroma – crescent shaped density in extra-axial space (matching density of CSF). often bilateral
- DAI/TAI – Most common CT finding after severe head trauma. Often no direct CT evidence and MRI may be required. Findings include small petechial hemorrhages in proximity of third ventricle and corpus callosum. Intraventricular hemorrhage predicts CC DAI on MRI
- ICH – intracerebral hematoma – well defined hyperdense area of hemorrhage within brain parenchyma. Be aware of a subset of bleeds that occur in cerebellum = traumatic intracerebellar hematoma
- Cerebral Edema
- Bilateral compression of ventricles
- Loss of effacement of cortical sulci
- Effacement of basal cisterns
[9] Outline management priorities in the TBI with respect to the following: Initial Resuscitation, ICP management and hyperosmolar therapy, indications for seizure and antibiotic prophylaxis, reversal of anti-coagulation, and decompressive therapies
- Initial resuscitation
- C spine precautions
- Keep neck in neutral position, elevate HOB 30º, ensure collar not overly tight, avoid jugulars for venous access
- Early neuroprotective intubation and adequate sedation
- Target normocarbia overall (hyperventilation may transiently be used to decrease ICP)
- Prevent hypotension (target SBP ≥100 if possible – remember that increasing MAP can decrease ICP in a brain with some autoregulation intact).
- Prevent hypoxia
- Facilitate diagnostic evaluation with CT
- Target normoglycemia, normocarbia, avoid severe acidosis/alkalosis
- ICP management and hyperosmolar therapy
- Indication: Impending herniation suggested by deepening coma, asymmetric/fixed pupils, or development of other lateralizing signs
- HTS (3% Saline): 100cc over 10min, or 3mL/kg (?higher to 5cc/kg) over 30min with repeat doses q6h to max sodium of 160mmol/L (AEs = renal failure, central pontine myelinolysis, rebound ICP elevation).
- Mannitol 1g/kg q6h to a maximum serum osmolality of 320mosm/kg (AEs – hypotension, renal failure, or increased bleeding into a traumatic lesion by decompressing the tamponade effect of a hematoma).
- Indication: Impending herniation suggested by deepening coma, asymmetric/fixed pupils, or development of other lateralizing signs
- Indications for seizure and antibiotic prophylaxis
- Seizure prophylaxis in ED – penetrating TBI
- Antibiotic prophylaxis – penetrating TBI
- Don’t forget tetanus
- Reversal of anticoagulation
- Give specific reversal agents as indicated
- TXA use is controversial
- Decompressive therapies such as Burr hole (do AFTER imaging in consultation with Neurosurgery for possible EVD or decompressive craniectomy if in a tertiary centre.
[10] List the complications of TBI
- Seizures
- Early posttraumatic Seizures <24h – usually brief and caused by transient neurochemical changes within the brain. Not associated with worse outcomes.
- PTS within 24-48h post injury – caused by worsening cerebral edema, hemorrhage, or penetrating injury.
- Seizure prophylaxis in the ED is recommended for penetrating injuries
- CNS infections
- Brain abscess (penetrating injury)
- Antibiotic prophylaxis is indicated for penetrating TBI.
- Posttraumatic meningitis after basilar skull fracture
- Evidence is equivocal for antibiotic prophylaxis in patients with basilar skull fracture or CSF leak
- Cranial osteomyelitis
- Brain abscess (penetrating injury)
- Systemic complications of TBI
- DIC (specifically cerebral DIC)
- Neurogenic pulmonary edema (minutes to days after onset of head trauma) – likely related to systemic surges of catecholamines and pro-inflammatory mediators
- Cardiac dysfunction (likely due to increased catecholamines)
Wisecracks:
[bg_faq_start][1] What are the layers of the scalp?
S – skin
C – connective tissue
A – aponeurosis
L – loose areolar tissue
P – periosteum
So, you say to yourself, who cares? Well, if the aponeurosis is breached, the wound is likely going to gape and bleed profusely. Deep sutures will likely be required to approximate the aponeurosis prior to closing the skin.
[2] What is the Munro-Kellie doctrine?
The sum of the volumes of brain tissue, CSF, and blood must remain constant, assuming the skull is a closed space. Therefore an increase in one should cause a decrease in one or both of the remaining constituents.
[3] What is Cushing’s Reflex?
The Cushing reflex is a physiologic response to increased ICP resulting in a triad of increased pulse pressure (increased SBP, decreased DBP), bradycardia, and irregular respirations.
[4] List the clinic features of basal skull fracture
- Hemotympanum
- Blood in ear canal
- CSF rhinorrhea/otorrhea
- Battle’s sign (retroauricular hematoma)
- Raccoon eyes (periorbital ecchymosis)
- Cranial nerve deficits
- Facial paralysis
- Decreased auditory acuity
- Dizziness
- Tinnitus
- Nystagmus
This list was informed by Table 34.2 in Rosen’s 9th Edition. Refer to the text for further information
[5] Describe 3 clinic decision rules that apply to neuroimaging in mild TBI
1. Canadian Computed Tomography Head Rule (CCHR)
High-Risk Injury (May Require Neurologic Intervention)
- GCS score < 15 at 2 hours after injury
- Suspected open or depressed skull fracture
- Any sign of basal skull fracture (hemotympanum, raccoon eyes, CSF otorrhea or rhinorrhea, Battle’s sign)
- Vomiting ≥ two episodes
- Age ≥ 65 years
Medium-Risk Injury (May Have Important Brain Injury on CT)
- Amnesia before impact ≥ 30 min
- Dangerous mechanism: ex. pedestrian struck by vehicle, occupant ejected from vehicle, fall from elevation >3 feet (five stairs)
2. New Orleans Criteria (NOC)
- Headache
- Vomiting
- Age > 60 yr
- Drug or alcohol intoxication
- Persistent anterograde amnesia
- Trauma above the clavicle
- Seizure
3. NEXUS II Criteria
- Evidence of significant skull fracture
- Scalp hematoma
- Neurologic deficit
- Altered level of alertness
- Abnormal behaviour
- Coagulopathy
- Persistent vomiting
- Age ≥ 65 years
This List was informed by Table 34.4 in Rosen’s 9th Edition. Refer to the text for further information
[6] Describe a graduated return to play protocol as per Rosen’s
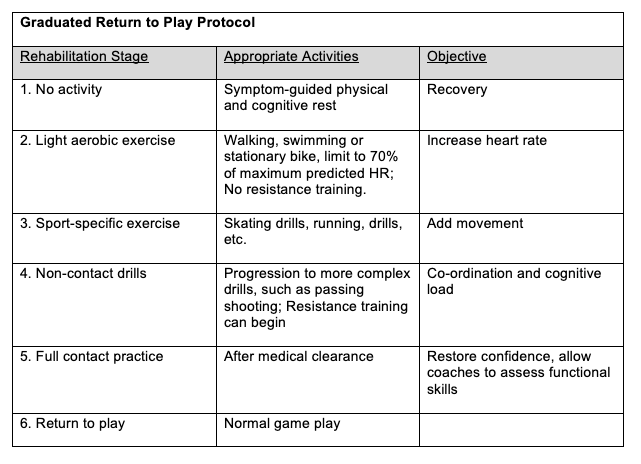
This table was informed by Table 34.3 in Rosen’s 9th Edition. Refer to the text for further information.
[bg_faq_end]This post was uploaded and copyedited by Tim Clark, www.timclarkmd.com



