This updated episode of CRACKCast covers Rosen’s Chapter 32 (9th Ed.) on back pain. This common complaint can be hard to evaluate, and this review will provide you with a framework to help.
Shownotes – PDF HERE
[bg_faq_start]Rosen’s in Perspective:
Back pain is the most common MSK complaint that we see in the ED. 85% of patients with acute low back pain (<6 weeks) are diagnosed with mechanical/nonspecific back pain, where no acute alternate diagnosis is found. Approximately 2% of patients will have an emergent diagnosis, such as AAA, cauda equina, SEA, cancer etc. The WHO defines nonspecific back pain as “back pain having no known underlying identifiable pathology and no apparent relative tissue damage.”
There are a multitude of causes of back pain. These can include vascular, visceral, infectious, mechanical and rheumatologic conditions. Pain may come from the spinal cord, nerve root, vertebral column, muscles, or have extraspinal/visceral origins. Low back pain often has no identifiable cause; possible explanations can include ligament/muscle injuries, degenerative disc disease and OA, and disc herniation.
So what is an emergency clinician supposed to do? The good news is that a thorough history and physical examination (and possible PVR) is all that is needed for the majority of low back pain patients. Labs and imaging are only indicated in a small subset of patients. We will give you an approach to acute back pain that will have you looking like a rock star next time you pick up one of these challenging patients on shift.
[bg_faq_end]Core Questions:
[bg_faq_start][1] List key historical red flags in a patient presenting with back pain.
- Recent Trauma
- History of cancer
- Anticoagulant use
- IVDU
- Prior prolonged steroid use
- Osteoporosis
- History of AAA
- Patient >50y
- Unrelenting night or rest pain
- Unexplained weight loss
- Recent bacterial infection
- Immunocompromised status
- Failure to improve after 6 weeks of conservative therapy
Mnemonic: TUNA FISH
This list was informed by Table 32.1 in Rosen’s 9th Edition. Refer to the text for further information.
[2] List red flags on physical examination of a patient with back pain.
- Abnormal vital signs (esp fever, hypotension)
- Unequal blood pressure readings in upper extremity
- Murmur of AI
- Pulse deficit or circulatory compromise of the lower extremities
- Pulsatile abdominal mass
- Urinary retention
- Urinary or stool incontinence
- Loss of rectal sphincter tone
- Severe or progressive neurologic deficit
- Focal lower extremity weakness
- New ataxia or difficulty walking
This list was informed by Table 32.1 in Rosen’s 9th Edition. Refer to the text for further information
[3] List key critical differential diagnoses for a patient presenting with acute back pain.

This table was informed by Figure 32.2 in Rosen’s 9th Edition. Refer to the text for further information
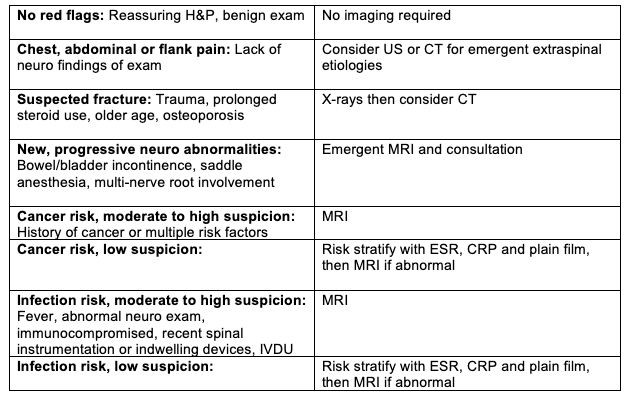
[4] Describe an ER diagnostic approach to the rapid assessment of a patient with acute lower back pain.

This table was informed by Figure 32.1 in Rosen’s 9th Edition. Refer to the text for further information
[5] Describe an approach to diagnosis and ancillary testing and imaging for critical causes of acute back pain.

This table was informed by Table 32.1 in Rosen’s 9th Edition. Refer to the text for further information
[6] List the sensory, motor, and screening tests for the lumbar nerve roots L3-S1.

This table was informed by Table 32.2 in Rosen’s 9th Edition. Refer to the text for further information
[7] Describe an overview of the management of acute low back pain.
This chart was informed by Figure 32.2 in Rosen’s 9th Edition. Refer to the text for further information
[bg_faq_end]Wisecracks:
[bg_faq_start][1] What are 4 variables associated with serious outcomes in patients with back pain
- Pain worse at night
- Decreased lower extremity sensation
- Use of anticoagulants
- Pain persisting despite appropriate treatment, appropriate disposition for these patients can often be a challenge.
[2] Differentiate between Conus Medullaris Syndrome and Cauda Equina Syndrome.
Conus Medullaris Syndrome
- Definition: Compression of the distal aspect of the spinal cord from T12 to L2.
- Typical site of lesion: L2 vertebral level (Differential diagnosis – disc herniation, spinal fracture, tumor)
- Symptoms: Back pain radiating to the legs, early and prominent sphincter dysfunction, flaccid paralysis of bladder and rectum, saddle anesthesia. May spare leg muscles and lumbar nerve roots
Cauda Equina Syndrome
- Definition: Compression of the nerves and nerve roots stemming from the distal end of the spinal cord.
- Typical site of lesion: L3-L5 nerve roots (L4/5 and L5/S1 disc herniation in 50% of cases)
- Symptoms: Bilateral radiculopathy, back pain radiating to legs, urinary retention (may present with overflow incontinence), fecal incontinence (with absent rectal tone), saddle anesthesia, lower extremity weakness.

[3] What physical exam or ancillary findings are most predictive of Cauda Equina Syndrome?
a. No clinical signs or symptoms are individually sensitive or specific enough to diagnose Cauda Equina Syndrome (or definitively exclude the diagnosis).
b. Using a post void residual of 200mL or more to risk stratify patients with CES has a sensitivity of 94% and an NPV of 98%. Normal PVRs are <50mL in young healthy patients, and <100mL in elderly patients.
c. If the diagnosis is suspected, pursue early consultation with spine surgery and MRI (gold standard) or CT myelogram if MRI unavailable. This is a time sensitive (potentially litigious) ER diagnosis.
Source: CJEM 2020;22(5):652–654
[4] How does Rosen’s differentiate between disc herniation and radiculopathy?
- Disc herniation is usually asymptomatic, and only occasionally causes symptoms.
- Radiculopathy is a clinical diagnosis of nerve root irritation and compression, with symptoms in the affected nerve root (numbness, weakness, and paresthesias). The most common causes of radiculopathy are disc herniation and degenerative foraminal stenosis.
This post was copyedited and uploaded by Tim Clark. www.timclarkmd.com



