This episode of CRACKCast covers Rosen’s chapter 84, Hypertension. Often thought to be a problem better handled by family physicians, hypertension is a frequent encounter in the ED where decision making between intervening and doing nothing is often the main hurdle.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
- HTN is common, and is on the rise in prevalence
- Definition:
- > 140/90 in the general population
- Cut off of 135/85 mmHg in patients who have their BP measured using automated BP devices in a relaxed, quite, alone environment.
- > 130/80 for people with chronic kidney disease or diabetes mellitus
- > 140/90 in the general population
- Cardiovascular mortality doubles with each 20/10 mmHg rise above the normal 115/75
- There are definite differences in HTN incidence and morbidity between ethnic groups (African American patients being more affected)
- Our job in the ED:
- To differentiate between people with asymptomatic elevated BP from those with symptomatic elevated BP (acute vasculopathy)
- Recent trends to shift away from cosmetic BP reduction, to focus on interventions based on actual clinical disease (e.g. end organ dysfunction).
- Hypertensive crisis, urgency, malignant HTN are now obsolete
[1] Define the three classes of hypertension relevant to emergency medicine practice
- Hypertensive emergency: “acute target-organ dysfunction, manifesting with newly developed clinical sequelae or consequential diagnostic test abnormalities”
- Poorly controlled chronic HTN: known HTN patient with asymptomatic elevated BP without end organ dysfunction
- Watch out for the following drugs as they can muddy the waters by increasing BP: NSAIDS/steroids/decongestants/appetite suppressants/over-the-counter stimulants/oral contraceptives/TCAs or rebound from short-acting antihypertensives (eg clonidine)
- Elevated BP without prior history of HTN: can’t be diagnosed with HTN in Ed (think white coat) but 70% of these patients go on the be diagnosed after appropriate w/o by GP or outpatient clinic
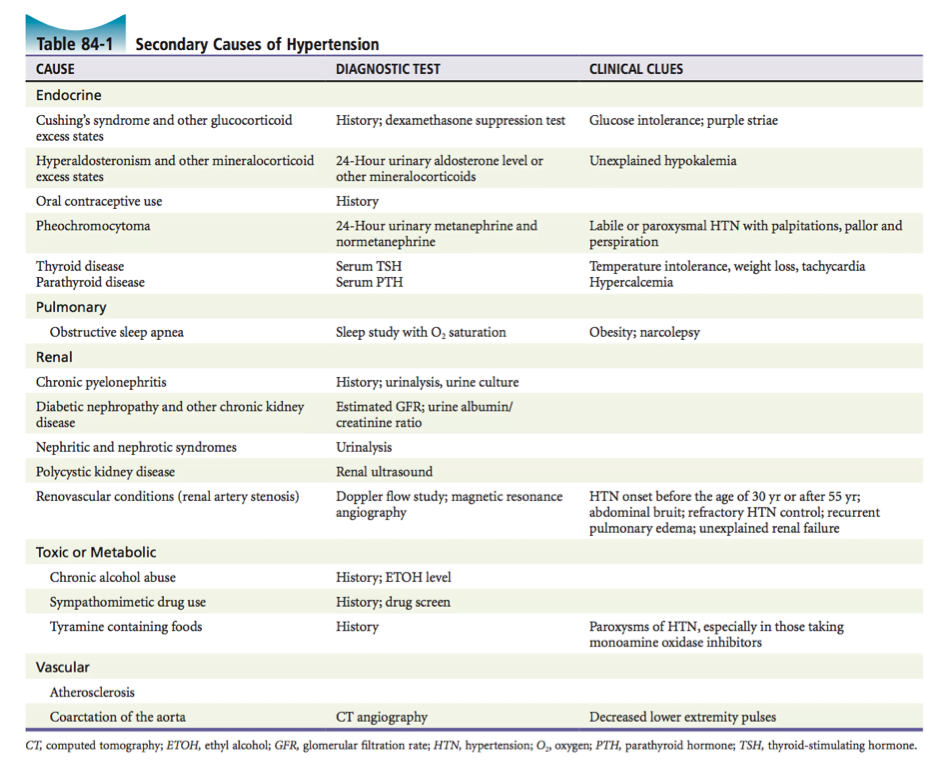
[2] List 10 possible etiologies for hypertension.
- Remember that hypertension – is either primary or secondary.
- We always need to think “why” are they HTNsive:
Here are some secondary causes:
[3] What is the pathophysiology of target-organ damage?
- Macrocirculation
- High SVR (due to peripheral arteriole back up from SNS and RAAS activation) increase LV mass
- LVH – Diastolic dysfunction
- Elevated LA end diastolic pressures
- Acute SVR rise = Flash pulmonary edema
- Chronic = leads to LVH – leads to ischemia (outgrowing blood supply) and eventual thinning of myocardium
- Thus end with big floppy bag of systolic dysfunction
- Microcirculation
- Critical luminal narrowing – occlusion and ischemia
- “Silent” ischemic episodes lead to primary cause of chronic end organ damage
- Lumen thinning – aneurysm and rupture
- Results in tissue edema, fibrinoid necrosis, and microangiopathic hemolytic anemia
Now, Hypertensive emergencies get a little more crazy (typically pressures > 180/110)
- Abrupt rise in pressure overwhelms autoregulation = endothelial injury
- Post injury, a major vascular smooth muscle relaxant (Nitric Oxide) in decreased
- This leads to further increase of SVR = downward spiral that maintains elevated BP
- Left unchecked, this leads to terminal arteriole dilation and rupture = badness
[4] How does hypertensive encephalopathy occur?
THIS IS A TRUE EMERGENCY!!!!
- People presenting with severe headaches, vomiting, altered mental status, seizures, coma, blurred vision, neurologic deficits in multiple nerve distributions (due to diffuse cerebral dysfunction.
- These people have normal CT heads (or no new interval changes) + markedly elevated BPs + papilledema. BUT A REAL THING CALLED PRES.
- Failure of autoregulation
- Leads to vasospasm -> ischemia -> increased vascular permeability -> punctate hemorrhages -> interstitial edema
NET RESULTS: Diffuse vasogenic cerebral edema. You worry about exploding heads with shifting Na too fast, this is the same thing in the end. Don’t let your patient’s heads blow up in front of you…(to exaggerate!)
[5] List 6 hypertensive emergencies; their management goals; the optimal agents for BP control and any relevant caveats
First lets talk injury pattern: see 84-2:
A couple caveats:
- Symptoms like headache, epistaxis, dizziness in and of themselves DON’T in isolation mean that patient is having a hypertensive emergency!
Next the meat and potatoes:
A little more about ER diagnostics in the hypertensive patient (depending on clinical suspicions):
- CBC (look for MAHA)
- Metabolic panel with creatinine and GFR
- Urine – for urine albumin to creatinine ratio and proteinuria / vs. active urine sediment?
- To assess for subclinical renal disease!
- CXR
- ECG
- +/- troponin / BNP***(many caveats!)
- CT
- Fundoscopic findings may be absent in up to 30% of people!
Goal of this testing is to help further evaluation and future patient management.
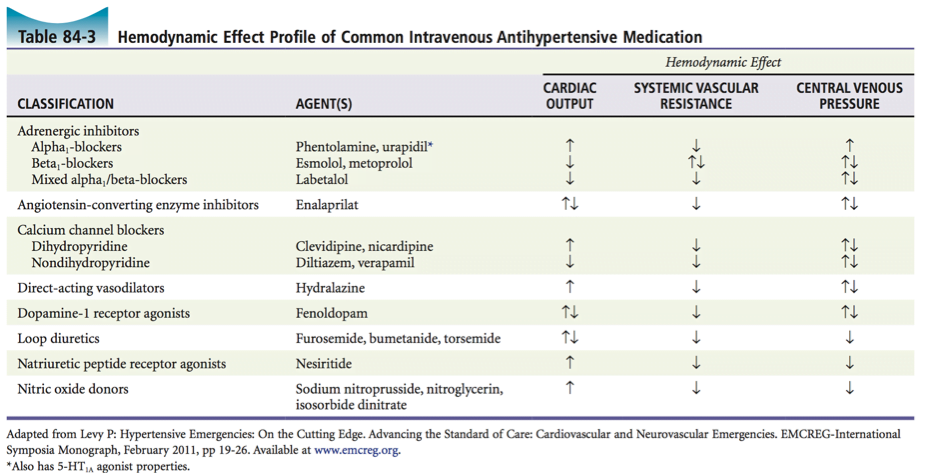
[6] List five intravenous antihypertensive medications and their mechanism of action.
[7] Describe the ER management of poorly controlled HTN
Depends on patient’s follow-up:
- If they have a GP or internist = nothing to be done in ED
- If they don’t have follow-up, Rosen’s suggest initiating antihypertensive agent and arranging follow-up is possible
However, quote from Rosen’s : “Acute BP reduction in the ED provides absolutely no benefit to patients with chronic HTN and exposes them to unnecessary risk of potential hypoperfusion in regions where blood flow has been governed by long-standing autoregulation.”
If non-compliant with meds: restart them. Arrange F/U.
Wisecracks – What are the management targets / indications for treatment in the following patients:
[bg_faq_start][1] 57 yo male with ICH and no signs of ↑ ICP
- According to Rosens: (based upon INTERACT and ATACH trials) SBP should be targeted between 160 and 180 mm Hg
- According to ATACH II (SEE SGEM here) no benefit of aggressive management, so we will stick with SBP goal of 140 -179
- “SGEM Bottom Line: Intensive blood pressure reduction (SBP 110-139 mm Hg) does not provide benefit over standard blood pressure reduction (SBP 140-179 mm Hg) in patients with acute intracerebral hemorrhage.”
- Esmolol / labetalol / Nicardipine are good choices. NO donors (Nitro, Nitroprusside) should be avoided as they can increase ICP
[2] 58 yo female with acute ischemic stroke
- 185/110 mm Hg if thrombolysis planned
- 220/120 mm Hg if no thrombolysis. NOTE: decrease BP by 15 % in 24hrs gradually, otherwise can worsen ischemic penumbra
[3] 39 yo female with SAH in the ED
- According to Wikiem here consensus guidelines:
- Avoid hypotension: Maintain MAP>80 (CPP of 60 as long as ICP<20)
- Give IVF / Give pressors if IVF ineffective
- Avoid hypotension: Maintain MAP>80 (CPP of 60 as long as ICP<20)
- Hypertension: AHA/ASA has no formal recommendations but states that decreasing to SBP <160 is reasonable
- Rapid SBP lowering <140 has been advocated with early research showing improved functional outcome, but more recent work has found no difference between SBP <140 and <180 (our Neurosx usually say <150 mm Hg if unsecured)
- Ensure appropriate pain control and sedation before adding antihypertensives
- Discontinue/reverse all anticoagulation
- Coumadin → (Prothrombin complex conc or FFP) + vitamin K
- Aspirin → DDAVP
- Plavix → Platelets (controversial now with PATCH trial showing no benefit and possible harm)
- Dabigitran (Pradaxa) → Idarucizumab (Praxbind): 5 grams IV
- Nimodipine: Only CCB studied that has been shown to prevent vasospasm (associated with improved neuro outcomes and decreased cerebral infarction)
- Give 60mg q4hr PO or NGT only (never IV) within 96hr of symptom onset. NNT 13 to prevent one poor outcome
- Keep an eye on BP for fluctuations
- Magneisum sulfate: Controversial; prevents vasospasm acting as NMDA antagonist and a calcium channel blocker; maintain between 2-2.5 mmol/L
- Seizure prophylaxis: Controversial; 3 day course may be preferable
- Phenytoin, levetiracetam, carbamazepine and phenobarb. Phenytoin can be associated with worse neurologic & cognitive outcome
- Glucocorticoid therapy: Controversial; evidence suggests is neither beneficial nor harmful
- Glycemic control: Controversial; consider sliding scale if long patient stay in ED while awaiting ICU bed
- Keep head of bed elevated
- Aneurysm treatment
- Surgical clipping and endovascular coiling are definitive treatment
- Antifibrinolytic – Controversial; if delayed aneurysmal treatment, consider short term therapy (<72 hrs) with TXA or aminocaproic acid
[4] 22 yo female with eclampsia
- If they still have a baby inside, DELIVERY IS DEFINITIVE MANAGEMENT
- Still can present post delivery
- Aggressive BP management is Key, SBP <160 or until they stop seizing
- Magnesium sulfate is first line therapy
- May need to add Hydralazine / labetalol
- Can add Nicardipine if no effect
[5] 66 yo female with ACS
- Don’t forget primary goal is reperfusion
- Need to lower afterload / augmentation index (that peripheral BP pulse wave back to the central circulation)
- Titrate to symptom resolution, avoid dropping beyond 120/80 (increases complications)
- NO donors (nitroglycerin infusion) are first line but don’t use with concurrent PDE5 inhibitors (Viagra, Cialis)
- Avoid betablockers in early treatment before reperfusion as can precipitate cardiogenic shock by dropping CO
[6] 57 yo male with aortic dissection
- THINK LOW AND SLOW
- Goal is to drop Sheer force and wall tension IE HR / CO / SVR
- In other words drop dP/dT (lv ejection sheer force over rate)
- SBP <110 or titrate to mentation
Check out this great EMCases post here –> As they put it:
1st: Pain control to counter sympathetic contribution to elevated heart rate and blood pressure
- Fentanyl 25-50 mcg boluses
2nd: HR control to a goal of 60 bpm
- Esmolol 0.5mg/kg bolus then 50-300 mcg/kg/min or Labetalol 10-20mg bolus then 0.5-2mg/min or Warning: giving a vasodilator without concomitant reduction in ionotropy may cause progression of dissection
3rd: BP control to a goal of SBP = 110
- Nitroprusside 0.25-0.5 mcg/kg/min then titrate or Nicardipine 5mg/hr
- Warning: Beware of pseudohypotension! of the bilateral BPs use the higher BP reading.
[6] 62 yo female with ICH, ↓ GCS, shift on CT scan
- Standard herniation syndrome tx stuff
- HOB elevated
- Do not occlude vascular structures (collars / neck compression / head midline)
- SBP 140-160
- MAP >80 or CPP >55 if measured ICP
- Treat w/ Mannitol or Hypertonic
- Hyperventilation to PCO2 30-35
- Neurosx Stat
- Reverse anticoags
[7] 55 yo female with multiple vague complaints (dizziness, headache, weakness, and hand numbness)
- According to Rosen’s there is NO evidence that acutely lowering BP in people with probably chronic HTN benefit from acute BP reduction.
- Observe in a quiet area (…doesn’t anyone know of such a place in the ER?). Then reassess. There is not target BP that dictates a safe discharge, and acutely lowering the BP with a drug such as a hydralazine is “without rationale or benefit.”
- R/O HTN Emergency or PRES (see LITFL post here )
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)