This episode of CRACKCast covers Rosen’s Chapter 75, Upper Respiratory Tract Infections (URTI). This spectrum of disease involves a range of management strategies, all the way from supportive care to life-saving interventions.
Shownotes – PDF Here
[bg_faq_start]Rosens in Perspective
For these questions, see “CC E023 – Sore Throat”
- List 4 Centor criteria and how management proceeds
- Describe 3 diagnostic tests for infectious mononucleosis
- Describe the management of GABHS
[1] List potential causes of pharyngitis; List 5 viral and 5 bacterial etiologies of pharyngitis
Emergent Diagnoses for Sore Throat
Diseases not to miss:
- Primary HIV
- Epiglottitis
- Bacterial tracheitis
- Corynebacterium Diphtheriae
- Ludwig’s angina
- Epstein barr virus
- Cancer
- Gonorrhea / Herpes Simplex
- Foreign body
- Angioedema
- Peri-tonsillar abscess
- Retro-pharyngeal abscess
The most common viral, bacterial, and non-infectious causes of sore throat (list at least 8)
Viral – MOST common cause of acute pharyngitis
- Rhinovirus
- Adenovirus
- HSV 1&2
- Influenza
- CMV
- EBV
- Varicella-zoster virus
- Hepatitis virus
Bacterial
- Group A beta-hemolytic streptococcus
- Non-group A strep.
- Neisseria gonorrhoeae
- Neisseria meningitidis
- Mycoplasma pneumoniae
- Chlamydia trachomatis
- Corynebacterium diphtheriae
- influenzae
Non-infectious causes:
- Systemic disease: Kawasaki’s, SJS, cyclic neutropenia, thyroiditis
- Trauma – retained foreign body, laryngeal #, hematoma, CAUSTIC exposure, POST-tonsillectomy eschar
- Tumours – tongue, larynx, thyroid, etc
[2] What are the indications for steroids in a patient with pharyngitis?
Complex issue!
Cochrane review in 2012 concluded that symptoms were improved, but recurrence rates did not change. The study was also underpowered for complication, and not enough children were included for analysis.
- ***infectious mononucleosis, peritonsillar abscess, and post-tonsillectomy patients were excluded, as these patients usually are managed with steroids.***
Check out: http://www.thennt.com/nnt/steroids-for-pharyngitis/
The plot thickens with a recent publication in JAMA, which showed no difference in intervention versus placebo with complete resolution of symptoms at 24hrs, but did show a reduction in symptoms at 48 hours. ***This is only in Adults***
Article from JAMA Here:
In summary, indications for steroids according to UpToDate:
- Only severe symptoms and inability to swallow
- Airway obstruction
- Infectious mononucleosis
- Peritonsillar abscess
- Post-tonsillectomy patients
[3] List causes of epiglottitis
Background:
- Despite the decreasing incidence of pediatric epiglottitis, adult epiglottitis remains prevalent
- What it is:
- Localized cellulitis of the supraglottic structures: base of the tongue, vallecula, aryepiglottic folds, arytenoids, lingual tonsils, epiglottis
- The term supraglottitis is probably more anatomic
Causes:
- Influenzae Type B
- Staph.
- Strep.
- Viruses
- Thermal injury
Presentation:
- Classically:
- Adult, male, smoker with a “benign” URTI for the past few days who complains of dysphagia, odynophagia, and “sore throat/pharyngitis” with a “normal” oropharynx/tonsil exam
- Alternatively:
- People can come with a prodrome of 7 days or as short as a few HOURS of sore throat!
- Watch out for the rapidly progressive sore throat in the immunocompromised
- Dysphonia, ear pain, muffled voice
- Fever is absent in 50% of cases
- Tenderness to palpate the anterior neck (hyoid) or pain with larynx manipulation side to side
- Watch out for the patient who is unable to swallow their own saliva, drooling, or spitting up into a cup
Management:
- Ensure the patient’s airway remains patent and protected
- Consider preventative intubation in anyone who has rapidly progressive symptoms over 6 hrs or less
- Have a lower threshold for the diabetic or immunocompromised
- IV Abx:
- Ceftriaxone
- Cefotaxime
- Septra
- Maybe?
- Steroids
- Racemic epinephrine (in preparation for intubation)
- Analgesia
- Humidified oxygen
- Observation in a high-acuity area
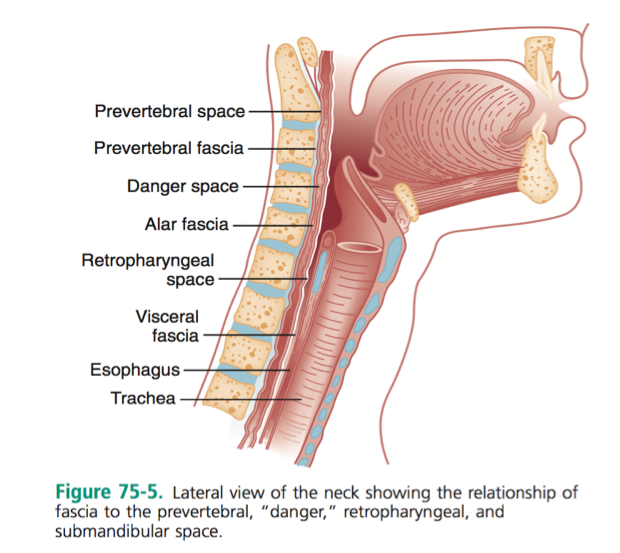
[4] What are the deep spaces of the neck? List 4 deep space infections of the neck
- Submandibular space: sublingual and submaxillary spaces. Think Ludwig’s Angina here
- The parapharyngeal space contains the carotid artery, the jugular vein, the cervical sympathetic chain, and cranial nerves IX through XII
- The retropharyngeal space lies in the midline and extends from the base of the skull to the superior mediastinum (level of T2)
- Danger space Posterior to the retropharyngeal space lies this “danger” space, which extends from the base of the skull to the diaphragm
- The prevertebral space extends from the base of the skull to the coccyx
[5] What are the typical bacterial causes of deep space infections? What are the different syndromes called?
- Most frequently isolated organisms are streptococci, staphylococci, and Bacteroides species.
- β-Lactamase– producing organisms are isolated in ⅔ of cases.
- Other organisms include H. influenzae, Pseudomonas aeruginosa, Klebsiella species, and Candida albicans
[6] What are the potential complications of deep space neck/face infections? List 5.
- Airway Obstruction
- Trismus
- Lemierre’s syndrome
- Carotid aneurysm
- Cavernous sinus thrombosis
- Retropharyngeal abscess
- Empyema/pneumonia
- Sepsis/ acute respiratory distress syndrome
- Necrotizing fasciitis
- Mediastinitis
- Peri-myocarditis
- Osteomyelitis of the mandible, cervicothoracic necrotizing fasciitis
[7] When do the sinuses typically develop?
- Fully develop by age 10.
[8] What the pathophysiology of sinusitis? What are the typical pathogens?
- A healthy sinus – is sterile; with free air exchange and mucous drainage
- Ostial obstruction leads to sinusitis:
- Due to:
- Viral / allergic / ciliary paralysis (smokers)
- Leads to bacteria introduction by coughing, nose blowing → then overgrowth and infection
- Other causes of obstruction:
- Immunocompromised
- Septal deviation
- Nasal polyps
- Tumors
- Trauma
- Rhinitis medicamentosa
- Barotrauma foreign bodies
- Cocaine abuse
- NG tubes
- Due to:
- Pathogens:
- Pneumoniae
- Non-typable H.influenzae
- M. catarrhalis
- Pseudomonas
- Strep.
- Staph.
- Fungi
[9] Describe the management of acute rhinosinusitis and list 6 predisposing factors
Risk Factors:
- immunocompromised status
- nasal septal deviation and other structural abnormalities
- nasal polyps
- tumors
- trauma and fractures,
- rhinitis medicamentosa (rebound rhinitis from overuse of decongestants)
- rhinitis secondary to toxic mucosal exposure
- barotrauma
- foreign bodies
- nasal cocaine abuse
- instrumentation (including nasogastric and nasotracheal intubation)
*Goal is symptomatic therapy*
- Neti Pot
- Local decongestant – Topical agents should not be used longer than 5 days, or increase risk of rhinitis medicamentosa
- Oral decongestants are no better than topical, and should only be used if patients cannot use topical. (e.g., phenylpropanolamine or pseudoephedrine) Avoid in poorly controlled hypertension or concurrent use of tricyclic antidepressants, monoamine oxidase inhibitors, or nonselective beta-adrenergic blockers.
- If allergic component: loratadine 10 mg daily
- Antibiotics for febrile or immunocompromised patients, or patients or families with children at daycare. The choice of antibiotics should consider β-lactamase production and multidrug-resistant pneumococci. High-dose amoxicillin, 1 g (or 90mg/kg) three times a day administered for 7 to 10 days as first line
- Penicillin-allergic patients – trimethoprim- sulfamethoxazole or a macrolide antibiotic. A 3-day course of trimethoprim-sulfamethoxazole or azithromycin and decongestants may = 10-day antibiotic course
WiseCracks
[1] List 5 suppurative and 5 non-suppurative complications of GABHS
Suppurative
- Tonsillopharyngeal cellulitis or abscess
- Otitis media
- Sinusitis
- Necrotizing fasciitis
- Streptococcal bacteremia
- Meningitis or brain abscess, a rare complication resulting from direct extension of an ear or sinus infection or from bacteremic spread
- Jugular vein septic thrombophlebitis
Non Suppurative
- Acute rheumatic fever (ARF)
- Scarlet fever
- Streptococcal toxic shock syndrome
- Acute glomerulonephritis
- Pediatric autoimmune neuropsychiatric disorder associated with group A streptococci (PANDAS)
[2] List 4 findings on lateral neck X-ray of epiglottitis
- Remember the true dx is done with laryngoscopy; but radiographs have a Rosen’s reported 90% sensitivity — so missing 10% of people with this killer diagnosis isn’t bueno
- Findings:
- Obliteration of the vallecula
- Swelling of the arytenoids and aryepiglottic folds
- Edema of the prevertebral/retropharyngeal soft tissues
- Ballooning of the hypopharynx and mesopharynx
- Edematous epiglottis
- Rule of 8 for Epiglottis: >8mm = bad
Case courtesy of Dr Andrew Ho, Radiopaedia.org. From the case rID: 22906
Edematous Epiglottis/ Aryepiglottic Folds / Thumb Print Sign
Case courtesy of Dr Gagandeep Singh, Radiopaedia.org. From the case rID: 8414
Ballooned / Overdistended Hypopharynx
****Normal soft tissue plain films do not exclude the presence of adult epiglottitis*****
In Summary:
- Think of supraglottitis in anyone with:
- Severe throat pain
- Altered voice
- Dyspnea
- Inability to swallow secretions
[3] Describe an approach to airway management in deep space neck infections
- Be ready to call a friend or two (ER colleague, anesthesia, **otolaryngology** for surgical airway and drainage) if the patient needs to be intubated
- These are difficult airways – you should have a double setup and plan to use awake flexible bronchoscopic intubation with gentle airway topicalization
- Don’t lay them down flat – keep them in the sniffing position
- IV antibiotics
- IV steroids (for some cases)
- Those with deep space neck cellulitis – often resolve with antibiotics alone, abscesses need COLD STEEL
- May want to consider involving infectious diseases – especially in cases of vertebral osteomyelitis
Check out these links for more:
- https://emcrit.org/podcasts/awakeintubation/
- https://canadiem.org/missing-awake-intubation-kit-episode-2/
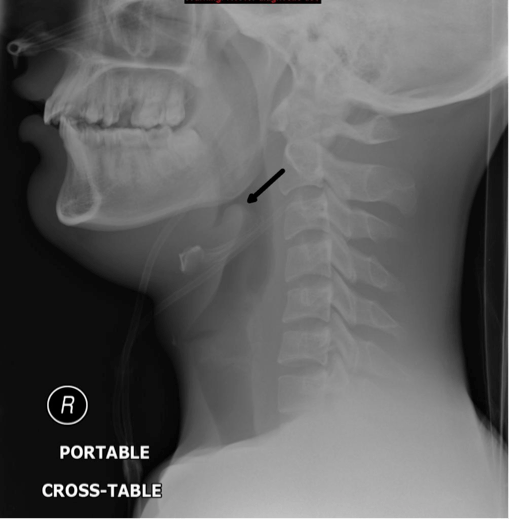
[4] What are lateral neck X-ray findings suspicious for RPA?
A few rules of thumb for the lateral soft tissues of the neck
- Ant-Post. Diameter of the soft tissues along C1-C4 should be less than 40% of the AP diameter of the vertebral body just behind it.
- If it’s bigger than this – suspect an abscess
A pathologic retropharyngeal space on a lateral neck x-ray should be suspected if:
- At C2 – > 7mm
- Applies to both children and adults
- At retrotracheal space (C6)
- > 14 mm in kids
- > 22 mm in adults
- Reversal of normal cervical lordosis
- Air fluid levels in the abscess
- Foreign bodies
- Vertebral body destruction
Need to make sure that they are true lateral films
- Neck fully extended during deep inspiration
- Measure distances from anterior, inferior aspect of the vertebral bodies
CT/MRI are much more reliable
[bg_faq_end]
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)