This episode of CRACKCast covers Rosen’s Chapter 72, Otolaryngology. As a broad discipline, there are many common ENT presentations seen daily in the Emergency Department and a solid approach.
Shownotes – PDF Here
[bg_faq_start]Rosens in Perspective
- The Head and neck is home to some tres importante structures. Those painful ears are going to be a common presentation for any emergency room physicians’ practice. 80% of kids will have a case of AOM in their life, with 40% having up to three episodes by age 3.
[1] Define Otitis Media
- Acute – signs and symptoms of an infection with evidence of effusion
- Note: also called acute suppurative or purulent otitis media
- Chronic – Also called chronic suppurative OM, refers to chronic discharge from perforated TM.
- Recurrent – >3 episodes of AOM over 6 months or >4 in one year
Otitis Media with effusion is effusion WITHOUT signs and symptoms of infection. Also described as serous, non-suppurative, or secretory OM.
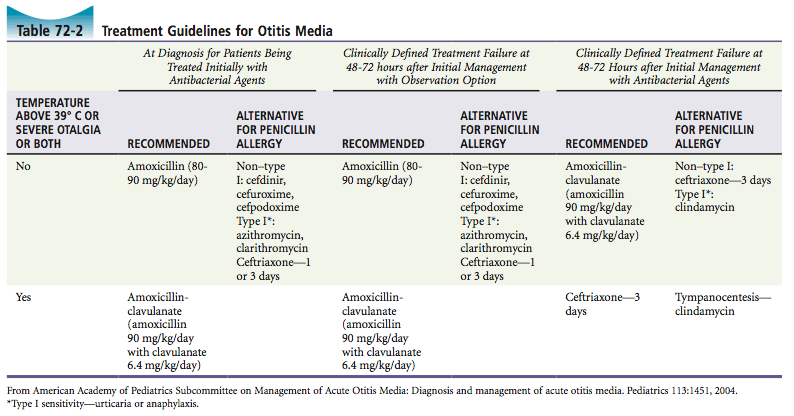
[2] Describe the diagnosis and treatment of Otitis Media
Acute Otitis Media Otitis Media Bullosa
Image: Labelled for reuse from Wikipedia Image: Labelled for reuse from Wikipedia
Essentially, the diagnosis requires two components:
- Signs and symptoms of middle ear inflammation
- Bulging of tympanic membrane
- Erythema
- Otalgia
- Fever
- Middle ear effusion
- TM opacity
- Lack of TM mobility
- Air-fluid level
- Otorrhea
[3] What are the complications of Otitis Media?
- Content supplemented with UpToDate: Otitis Media, check it out for more!
Intratemporal complications
- TM retraction with hearing loss
- Ossicular erosions
- Retraction pocket formation
- Balance and motor problems
- TM perforation
- Chronic suppurative otitis media
- Cholesteatoma
- An abnormal growth of squamous epithelium IN middle ear +/- mastoid, can lead to:
- Destruction of the ossicles
- Recurrent AOM
- Retraction pockets in the TM-cholesteatoma
- Mastoiditis
- An abnormal growth of squamous epithelium IN middle ear +/- mastoid, can lead to:
Intracranial complications
- Meningitis
- Epidural abscess
- Brain abscess
- Lateral sinus thrombosis
- Cavernous sinus thrombosis
- Subdural empyema
- Carotid artery thrombosis
[4] Describe the diagnosis and treatment of Otitis Externa?
Spectrum of disease: think cellulitis of the external auditory canal. Most likely causative agents include Pseudomonas and S. Aureus, but it can be polymicrobial (Swimmer’s ear is a form of OE).
Clinical diagnosis:
- Itchy, painful, red
- Swollen auditory canal
- Pain with tugging on auricle or tragus
- Associated adenopathy
- Otalgia
- Ear pressure / fullness
- Hearing loss
- Jaw pain
Treatment: regular cleansing and treat underlying infection
- Tap water, sterile saline, 2% acetic acid or Burows solution (aqueous solution of aluminum triacetate)
- Topical antibiotics: cure rate 80% within 10days.
- A combination of polymyxin B, neomycin, and hydrocortisone 3 or 4 drops to the affected ear 4x / day
- Ofloxacin (5 drops) or ciprofloxacin with hydrocortisone 3 drops given twice a day may be better, as less interval means more patient compliance. In Canada we have Ciprodex (ciprofloxacin and dexamethasone)
== This is different from malignant otitis externa ==
[bg_faq_start]Differentiate from malignant otitis externa
New name: Necrotising otitis externa.
- HIGH MORTALITY!!!
- High association with immunocompromised patients (elderly, diabetes, HIV/AIDS etc)
- Usual bugs – PSEUDOMONAS/S. aureus/ S. epidermidis/ Proteus mirabilis/ Klebsiella/ Aspergillus/ Salmonella
- Infection spreads from canal through floor of meatus via fissures of Santorini
- Can spread to cause skull-base osteomyelitis.
Think OE with Cranial Nerve/intracranial involvement or an ill appearing patient!
- Need to image (CT/MRI)
- Oral or IV cipro is the way to go: great penetration into bone. Treatment duration for 6-8weeks.
- Little evidence for hyperbaric treatment, but sometimes recommended as adjuvant.
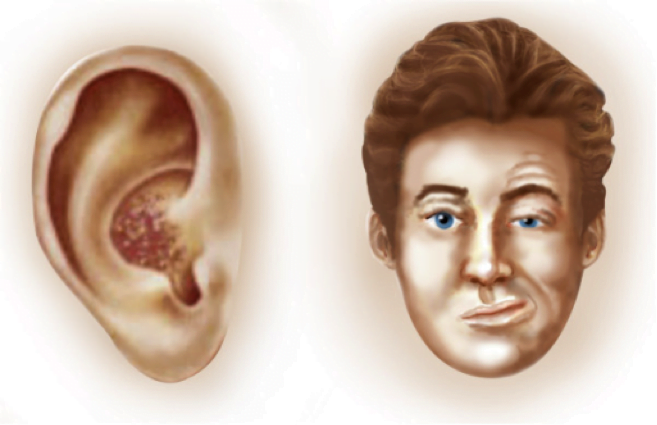
[5] What is Ramsay Hunt Syndrome? How is it treated?
Triad: Ipsilateral facial paralysis, ear pain, and vesicles in the auditory canal and auricle
This is Herpes zoster oticus. Think viral infection of the auricle. Classic reactivation of VZV in 8th cranial nerve, can lead to hearing and vestibular problems. Can involve the facial nerve (CN 7) leading to facial paralysis. Thought to be worse than Bell’s palsy from HSV.
Look for pain, swelling and vesicles. Note: vesicles can form 7-10 days after primary infection.
Ramsay-Hunt Syndrome
Image: Labelled for reuse from Wikipedia
Treatment: analgesia and antivirals (little evidence to support):
- Acyclovir 800 mg five times a day
- Valacyclovir 1000 mg three times a day
[6] Describe your approach to sudden hearing loss? How is it treated?
Here we are worried about sudden sensorineural hearing loss (SSNHL). Usually idiopathic hearing loss of >30db. This is an ENT emergency! Usually seen is 40s-50s, male:female.
- Can be simple as difficulty with conversation to complete hearing loss.
- Outcome is based upon severity of hearing loss. Look for accompanying tinnitus for a clue.
- Make sure you don’t miss a central (stroke) cause.
Examine tympanic membrane and auditory canal (cerumen impaction or FB). Solid neuro exam including weber and rinne’s test.
[bg_faq_start]WEBER and RINNE, Normal vs. Abnormal Hearing
From Wikipedia:
Weber: In the Weber test a vibrating tuning fork (Typically 256 Hz or 512 Hz used for Weber vibration test; 512 Hz used for Rinne hearing test) is placed in the middle of the forehead, above the upper lip under the nose over the teeth, or on top of the head equidistant from the patient’s ears on top of thin skin in contact with the bone. The patient is asked to report in which ear the sound is heard louder. A normal weber test has a patient reporting the sound heard equally in both sides. In an affected patient, if the defective ear hears the Weber tuning fork louder, the finding indicates a conductive hearing loss in the defective ear. In an affected patient, if the normal ear hears the tuning fork sound better, there is sensorineural hearing loss on the other (defective) ear.
Rinne’s: The Rinne test is performed by placing a high frequency (512 Hz) vibrating tuning fork against the patient’s mastoid bone and asking the patient to tell you when the sound is no longer heard. Once they signal they can’t hear it, quickly position the still vibrating tuning fork 1–2 cm from the auditory canal, and again ask the patient to tell you if they are able to hear the tuning fork.
Normal Hearing: Air conduction should be greater than bone conduction and so the patient should be able to hear the tuning fork next to the pinna (outer ear) after they can no longer hear it when held against the mastoid.
Abnormal Hearing:
- If they are not able to hear the tuning fork after the mastoid test, it means that their bone conduction is greater than their air conduction. This indicates there is something inhibiting the passage of sound waves from the ear canal, through the middle ear apparatus and into the cochlea (i.e., there is a conductive hearing loss).
- In sensorineural hearing loss the ability to sense the tuning fork by both bone and air conduction is equally diminished, implying they will hear the tuning fork by air conduction after they can no longer hear it through bone conduction. This pattern is similar to what is found in people with normal hearing, but patients with sensorineural hearing loss will indicate that the sound has stopped much earlier. This can be revealed by the investigator (with normal hearing) placing the fork close to their own ear after the patient indicates that the sound has subsided, noting that the sound from the fork is still loud and clear to a normal ear.
Treatment: Mainstay but unsupported by literature is antivirals and steroids.
Other treatments with mixed results include:
- Intratympanic steroids
- Hyperbaric oxygen
- Antiviral therapy
- Vasoactive
- Hemodilution therapies, dextran, and magnesium.
[7] Name 10 causes of epistaxis
[8] Describe your approach to treatment epistaxis
ABCs: resuscitate early. Make sure you document vitals and use of anti-platelets and anticoagulants!
a) Anterior bleeds – Little’s area or Kesselbach’s plexus
Photo: Rosen’s Emergency Medicine
Treatment:
- Silver nitrate (bad with active bleeders)
- Cautery (don’t use longer than 10-15 seconds can perforate) start peripheral to central
- Bilateral septal cautery not advised
- Can use gelfoam or surgical
- Rhino rockets / rapid rhino or epistats (leave in for 48-72hrs)
- Traditionally patients with packing are placed on antibiotics to prevent risk of toxic shock syndrome, this practice is controversial
b) Posterior bleeds – large bleed despite adequate anterior packing
- Commercially available (epistat) or the good old foley
- REMEMBER NEED TO APPLY TRACTION
- Pack both nares with foley, blow up balloon partially with sterile water (saline can crystallize and cause deflation issues later), tug until well seated, apply traction (I use the green umbilical clamps). Can add a little more fluid to balloon.
- Leave packs in for 2-5days as per ENT. Antibiotics here are important (Keflex or Amox-Clav)
- Refractory cases may need CT and IR
[9] What is the differential diagnosis of neck masses?
[10] What is sialolithiasis? How is it treated?
Stone in a salivary gland: 85-90% of cases involve the submandibular gland: less common is parotid or sublingual.
Differential diagnosis is:
- Infections, inflammation, and granulomatous and neoplastic processes.
- Most common viral pathogen is mumps.
- Most common Bacteria are: Staphylococcus, Streptococcus viridans, S. pneumoniae, and H. influenzae
Clinical exam with palpation is the mainstay, can CT and U/S for supportive imaging and characterize size and location of stone.
Treatment:
- Massage/heat
- Sialagogues (ex lemon candies to promote salivation)
- Antibiotics if infection suspected (fever, increasing pain, purulent d/c)
- Lithotripsy as per ENT
- Treatment failure may end with surgical removal of entire gland
ENT F/U important immediately if stone cannot be removed in ED, or within 4-5 days if it can be.
[bg_faq_end]
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)