This episode of CRACKCast covers Rosen’s Chapter 71, Ophthalmology. Part A of this episode will open your eyes to the essentials of eye anatomy, diagnosis of pathology and approach to treatment of a wide variety of eye complaints.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
- You gotta know eye anatomy
- You should review our previous podcasts on the eye (Episodes 21 and 22)
- Check out the eye exam on Episode 22: VVEEP + slit lamp + fundoscopy
- And ALWAYS ask about contact lens use
1) Differentiate between alkaline and acid ocular burns – What is the treatment?
Chemical burns
- Alkali burns – liquefactive necrosis
- Drain cleaners, chemical detergents, solvents, lime, etc.
- Rare to cause injury unless pH >12
- Acid burns — coagulation necrosis
- Rare to cause injury unless pH <2
- Treatment
- Irrigation for at least 30 mins
- With or without morgan lens
- May need topical anesthetics
- Irrigate until pH is NORMAL
- Remove particulate matter from the fornices
- After irrigation
- Cycloplegic
- 5% erythromycin ointment QID
- Pain management
- Check IOP
- Severity of injury judged by corneal cloudiness
- Long term: scarring, symblepharon, glaucoma, cataracts
- Irritants, solvents, detergent, super glue, mace exposures are treated just like chemical burns
- Superglue: only need referral if eyelids are inverted and lashes scratching the eyeball
- Irrigation for at least 30 mins
2) What is the treatment of UV keratitis?
Radiation burns
- Ultraviolet keratitis (tanning booths, sunlamps, high altitude, welder’s arc)
- Latent period of 6-10 hrs then:
- Foreign body sensation, tearing, intense pain photophobia, blepharospasm
- Signs
- Decreased VA, conjunctival injection
- Treatment
- Cycloplegic
- Topical broad spectrum abx (weak evidence for this)
- PO analgesics
- Symptoms should resolve in 24 hrs
3) What is ophthalmia neonatorum? In which time-frame are each bacteria expected to be causative? What is the treatment?
Ophthalmia neonatorum
- “Conjunctivitis in the first month of life” transmitted from the mother’s birth canal
- Viral / bacterial / chemical causes
- Need to rule out N. gonorrhoeae or chlamydia
- gonorrhoeae shows up 2-4 days after birth
- Chlamydia appears 5-15 days after delivery
- May need a full septic workup
- Treatment:
- Ceftriaxone IM 50 mg/kg
- Topical polymyxin B
- Saline washes
- Topical erythromycin ointment (empiric treatment of choice)
- May need dual therapy (oral erythromycin and topical) if chlamydia is highly suspected
- SYSTEMIC extension of the infections require IV abx
4) Describe typical features of conjunctivitis and management options
Conjunctivitis
- #1 cause of a red eye
- Symptoms:
- Redness, FB sensation, lid swelling, eye crusting, drainage
- NO photophobia, NO visual loss
- Caseus:
- Viral, bacterial, mechanical, allergic, toxic
- Called KERATOconjunctivitis when the cornea is involved as well
- Most commonly viral
- Bacterial causes:
- Pneumoniae, H. influenzae, Staph, Moraxella, Neisseria gonorrhoeae, Klebsiella, Pseudomonas,
- Treatment:
- Warm compresses
- Topical ophthalmic antibiotics
- ***usually self-limiting without abx but they can lead to improved remission rates
- Trimethoprim/polymyxin; ciprofloxacin;
erythromycin x 7 days - AVOID steroids
- Culture only in cases of treatment failure
- Complications
- Corneal ulcers
- Keratitis
- Corneal perforation
- Key diagnoses not to miss:
- Neisseria Gonorrhoeae: Rapidly progressive pain and copious discharge (17-16B)
- Need IV abx
- Irrigation
- Topical abx
- Treat for chlamydia as well
- Viral causes:
- #1 cause of conjunctivitis (Adenovirus, and others)
- Symptoms:
- MORE redness and itching and eye irritation
- Watery –> purulent d/c
- Pre-auricular lymphadenopathy
- Concurrent viral illness
- Very contagious up to 12 days post onset
- Treatment:
- Artificial tears
- Cool compresses
- Handwashing
- Use ABX if NO improvement of symptoms after 72 hrs
- Neisseria Gonorrhoeae: Rapidly progressive pain and copious discharge (17-16B)
- Treatment:
- Pneumoniae, H. influenzae, Staph, Moraxella, Neisseria gonorrhoeae, Klebsiella, Pseudomonas,
- Allergic conjunctivitis
- IgE mediated
- To any allergen (chemical, cosmetics, environmental)
- Symptoms:
- Bilateral eye itching
- Glassy chemosis
- IgE mediated
- Watery discharge
- Treatment:
- Artificial tears
- Cool compresses
- Topical ocular decongestants, antihistamines, topical NSAIDS
5) Define pterygium and pinguecula
See YouTube video: https://youtu.be/8CcPA9WxEig
- Pterygium:
- Wedge shaped area of conjunctival fibrovascular tissue on the NASAL side of the sclera extending onto the cornea
- Risks
- Exposure to UV light (tropical areas)
- Surfer’s eye
- Symptoms:
- Eye irritation, visual changes
- Pinguecula:
- White/yellow flat/raised tissue next to the cornea
- Doesn’t extend into the cornea
- Treatment
- Protection from wind, sunlight, dust
- Also:
- Artificial tears
- Short course of topical NSAIDs if irritated
- Non-emergency referral to optho
- Surgery if extends
- Steroid drops?
- Memory aid:
- “t” crosses the line
- “i” doesn’t cross
- White/yellow flat/raised tissue next to the cornea
- Risks
- Wedge shaped area of conjunctival fibrovascular tissue on the NASAL side of the sclera extending onto the cornea
6) List 4 causes of SPK – and describe the management of each
Superficial punctate keratitis
- Superficial, multiple, pinpoint corneal defects.
- Symptoms:
- Pain, redness, photophobia, FB sensation
- Etiology
- UV burns (welders, sunlamps), conjunctivitis, topical drug eye drop toxicity, drugs with preservatives, minor trauma, contact lens use, dry eyes, blepharitis, mild chemical injury, etc.
- Treatment
- Remove underlying cause
- Non preserved artificial tears
- Tobramycin
- Cycloplegics
“Patients with a significant contact lens–associated superficial punctate keratitis should be advised to stop wearing their contact lenses and should be treated with a topical fluoroquinolone or tobramycin drops during the day, ointment at night, and ophthalmologic follow-up the next day.”
[bg_faq_end][bg_faq_start]7) Compare HSV keratitis and Herpes Zoster Infection – What is Hutchinson’s sign?
Herpes simplex
- May be primary or a re-activation
- Symptoms:
- FB sensation, tearing, photophobia, clear discharge, decreased vision
- Signs:
- Red eye, vesicles near eye,
- Superficial punctate keratitis, ulcer, or dendritic pattern on slit lamp exam

- Treatment
- Antiviral agents:
- Trifluridine 1% q 2hrs x 14 days
- Antibiotics prophylactically:
- Erythromycin 0.5% q 4 hrs
- Cyclopentolate
- NO topical steroids
- Optho follow up
- Antiviral agents:
Herpes zoster
- “Herpes zoster keratoconjunctivitis”
- Virus reactivation along the ophthalmic division of the trigeminal nerve
- Rash involves forehead and upper eyelid
- +++ pain
“Involvement of the nasociliary branch of the trigeminal nerve, which manifests with zoster lesions on the tip of the nose (Hutchinson’s sign), is associated with a 76% risk of ocular involvement versus a 34% risk if the nerve is not involved. Ophthalmic herpes zoster accounts for approximately 10 to 20% of all zoster cases and necessitates emergent ophthalmologic consultation. If not treated and recognized immediately, herpes zoster of the eye may result in acute necrotizing retinitis and vision loss.” – Rosen’s 7th Ed.
- Involvement of the nasociliary branch —> Hutchinson’s sign
- Vesicles on the tip of the nose
- 75% risk of ocular involvement
- ***If not recognized leads to acute necrotizing retinitis and vision loss***
- Treatment:
- Antivirals: acyclovir/valacyclovir/famciclovir
- ideally within 72 hrs
- Topical steroid agents
- Topical antibiotics (prevent secondary infection)
- Analgesia
- Cool compresses, lubrication
- Optho follow up
- Antivirals: acyclovir/valacyclovir/famciclovir
- PO acyclovir as effective as IV acyclovir for vitreous penetration
8) Define and manage
a) Hordeolum, aka “Styes” / Chalazion
- Localised, nodular, inflammatory processes
| Hordeolum | Chalazion | |
| Etiology | Begins as a diffuse swelling and erythema of eyeLID margin
Inflammation of glands of Zeis or HAIR follicles — Staph. species
| Obstructed Meibomian gland — > Swelling within the lid surface.
***lid margin is NORMAL*** |
| Symptoms | Pain, swelling redness | “” |
| Treatment | Warm compresses for 15 mins six times per day
Topical erythromycin rarely needed unless resistant to watchful waiting or signs of blepharitis | Rarely need I+D, if so need referral to optho |
b) Dacryocystitis / Dacryoadenitis
Dacrocystitis
- Infection of the lacrimal sac
- Due to nasolacrimal duct obstruction
- Caused by Staph. Aureus
- Symptoms:
- Pain, tenderness, swelling, erythema
- Treatment:
- Topical ocular and oral antibiotics (amox-clavulin)
- Warm compresses
- Gentle massage to express pppus
Blepharitis
- Thickened, mattered red eyelid margins with pronounced blood vessels
- NOT an infection., just an inflammation
- VERY common!
- Symptoms:
- Eye burning, itching, tearing, FB sensation, morning crusting
- Treatment:
- Rubbing eyelid margins with mild shampoo + cloth
- Warm compresses QID
- Severe: topical abx
9) Compare periorbital and orbital cellulitis PEX and treatment
— See Episode 22 —
Orbital Cellulitis
| Etiology | Symptoms | Important differences to periorbital cellulitis |
| Maxillary/ethmoid sinusitis Orbital trauma Dental Infection Need CT to rule out abscess | Eyelid swelling / redness Warmth of skin overlying orbit Tenderness over bone Palpebral injection/chemosis of the conjunctiva | Fever Ill / Toxic appearance Blurred vision Proptosis Painful or limited extraocular movements Binocular diplopia Edema of optic disk Venous engorgement of the retina |
| Further Work Up: | Treatments: |
| Measure IOP, if >20 may need surgery Blood cultures CT orbits to rule out: Foreign body Emphysema Hematoma Abscess Osteomyelitis Cavernous sinus thrombosis Consider lumbar puncture Admission to hospital | IV Antibiotics for skin and sinus flora: Pip-Tazo 4.5g IV plus Vancomycin 15-20mg/kg IV |
| Complications: Meningitis Cavernous sinus thrombosis |
Periorbital Cellulitis
| Etiology | Symptoms | Considerations |
| Bug bite Trauma Sinusitis | Lid erythema, warmth, tenderness, and swelling Low grade fever | Mostly in children RARELY leads to orbital cellulitis Usually strep/staph species |
| Treatments MILD CASES
MODERATE-SEVERE CASES or <1 year old
|
10) Describe the pathophysiology and PEX of acute angle closure glaucoma
Glaucoma
- Background:
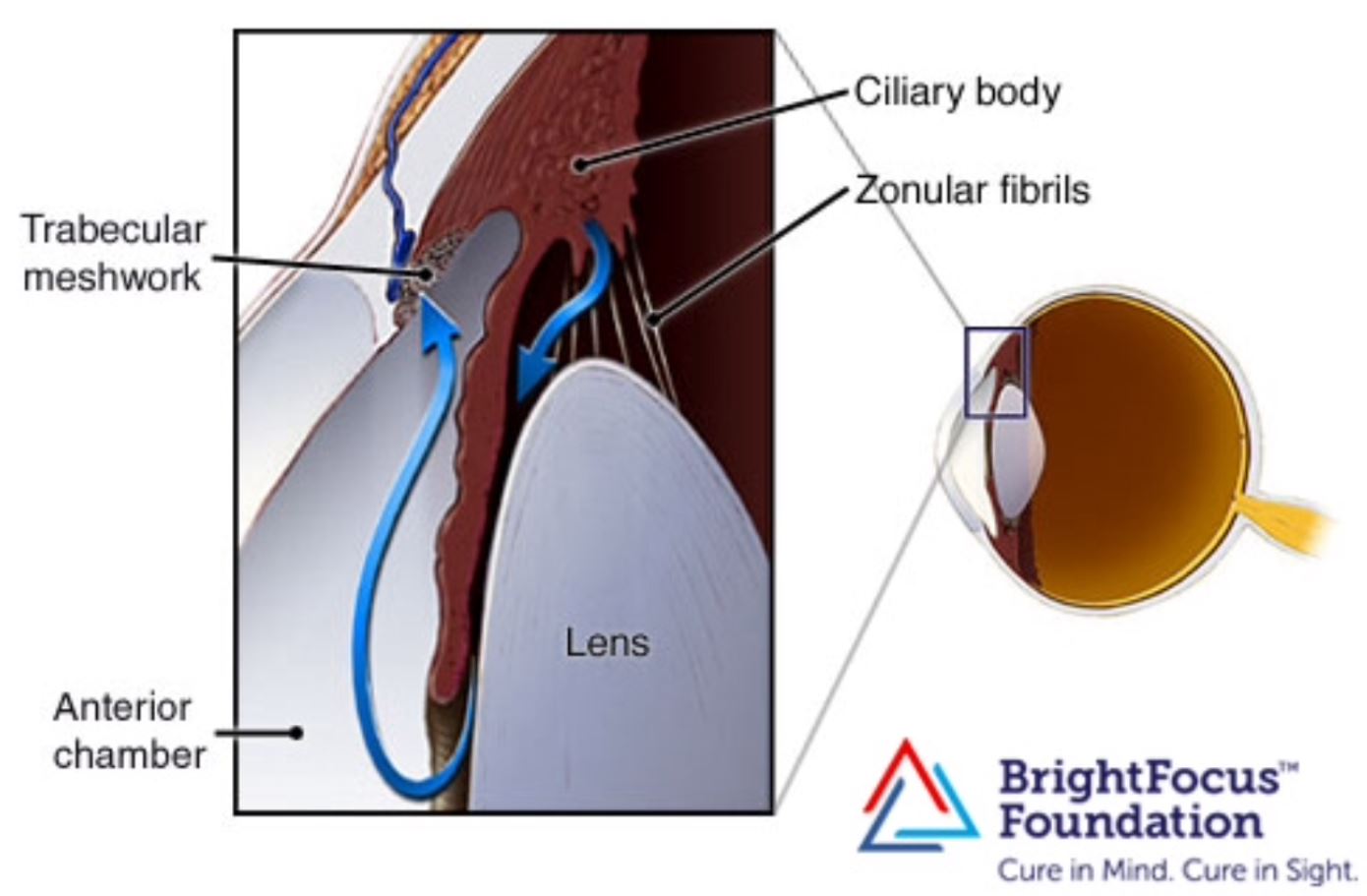
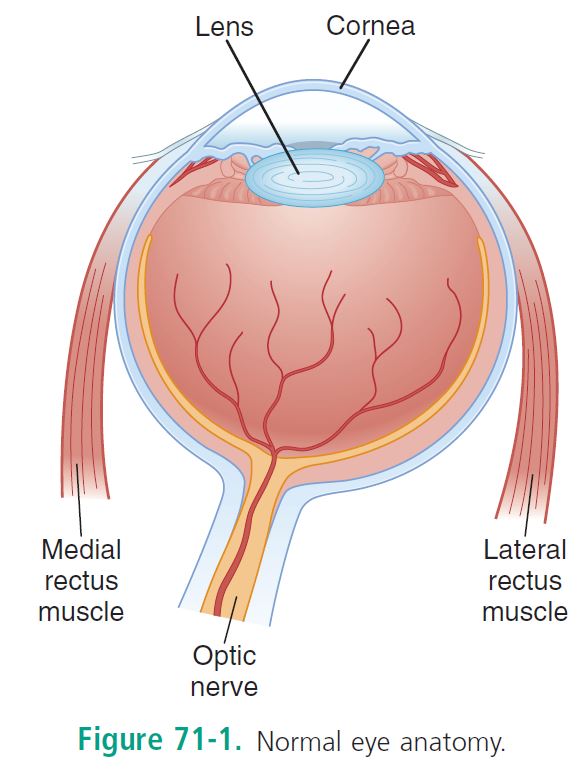
- Aqueous humour produced by ciliary processes
- Provides structural support
- Delivers oxygen and nutrients to the avascular cornea and lens
- Aqueous humour:

- Passes from the posterior chamber (ciliary body) —-> zonular fibrils –>pupillary aperture –> anterior chamber —> trabecular meshwork (one-way valve) –> canal of schlemm –> episcleral veins
- IOP determined by rate of aq. humour production to rate of outflow = 10-20
- “Glaucoma” is an optic neuropathy caused by increased IOP
- Classified as primary (unknown cause) or secondary
- May be open or closed (anterior angle is narrowed, preventing aq. humour outflow)
- Classified as primary (unknown cause) or secondary
- Aqueous humour produced by ciliary processes
Primary Open Angle Glaucoma
- #1 cause of blindness in USA
- Increased resistance to outflow of AQ humour through trabecular meshwork
- Insidious, slowly progressing, chronic, bilateral, painless
- Advance disease before symptoms occur
- Symptoms:
- Peripheral to central visual field loss
- Change in optic cup ratios
- Treatment:
- Argon laser trabeculoplasty
- Filtration surgery
- Topical BB
- Selective alpha 2 receptor agonists
- Carbonic anhydrase inhibitors
- Prostaglandin agonists
- Miotics
- Sympathomimetics
- Complications:
- Systemic side effects from eye meds
- BB –> asthma, heart block, CHF, depression, hypoglycemia
- Adrenergics–>HTN, dysrhythmias,
- Carbonic anhydrase inhibitors–>renal calculi, hypokalemia
- Systemic side effects from eye meds
- Symptoms:
Secondary Open Angle Glaucoma
- Etiology:
- Lens induced
- Inflammatory
- Exfoliative
- Steroid induced
- Traumatic
- Ocular tumor
11) List 7 therapies for acute angle closure glaucoma
Primary Angle Closure Glaucoma
- Risk factors:
- Anatomically small and shallow anterior chambers
- Age 55-70
- Results from “pupillary block”
- Lens and iris touch: flow of AQH from posterior to anterior chamber is stopped
- Triggered by events of pupil dilation (including sympathomimetic/anticholinergic drugs
- Iris bulges forward–>***obstructs the trabecular meshwork*** decreases flow
- Second mechanism occurs without pupillary block:
- Flat iris folds and bunches over the angle
- Symptoms:
- Sudden severe eye pain, blurred vision, headache, N/V, abd. pain
- Halo around lights
- Signs:
- Hazy cornea, mid-dilated pupil
- Conjunctival injection, steamy cornea, dec. VA, inc. IOP
Treatment:
- Decrease production of Aqueous Humour- Timolol 0.5% 1 drop, then repeat in 30 minutes
– Apraclonidine 1% 1 drop once
– Acetazolamide 500 mg PO – to reduce aqueous humour production
– Methazolamide 50mg PO instead of acetazolamide of the patient has sickle cell disease
- If IOP>30 (emergency)- Constrict pupil (Pilocarpine 4% 1 drop, then repeat in 15 minutes)
– Establish an osmotic gradient (Mannitol 2g/kg IV)
- Decrease IOP (other treatments)- Head of bed at 30 degrees
– Anti-emetics for prevention of N/V and prevent coughing
– Analgesics
- Decrease inflammation:- Prednisolone 1% 1 drop q 15 minutes
Just to recap:
- Timolol
- Pilocarpine
- Acetazolamide
- Head of bed at 30 degrees, prophylactic anti-emetics, and analgesics
TPAa…
Timolol, pilocarpine, acetazolamide, apraclonidine, anti’s
Surgery if these therapies ineffective
Secondary Angle Closure Glaucoma
- Pupillary block caused by a swollen or dislocated lens/post. synechiae due to adhesions
- Untraocular tumors
- ***CRVO***
- Post-op
- Treat:
- Fix underlying cause
In summary, (again!)
- The order of timolol, apraclonidine, and acetazolamide doesn’t matter
- Usually after two rounds of drops a third round doesn’t make any difference
- If IOP > 50, consider:
- Drugs to cause diuresis
- Use IV osmotics (mannitol 1 g/kg IV) and acetazolamide (carbonic anhydrase inhibitor – 250 mg IV) and regular drugs
- If IOP < 50
- Timolol 0.5% (dec. AQ production)
- Pilocarpine 1% (miotic agent)
- Apraclonidine 1% (alpha 2 agonist–dec. AQ humor production)
- Prednisolone 1%
12) List 10 ddx for acute painless visual loss
- Usually only affects one eye
- Sudden or over days
Let’s go through the “list”
- Vascular occlusion
- Central retinal artery occlusion – CRAO
- Central retinal vein occlusion – CRVO
- Retinal detachment
- Vitreous hemorrhage
- Posterior vitreous detachment
- Hemianopsia due to stroke
- Pituitary tumour
- Macular degeneration
- Non-arteritic ischemic optic neuropathy
- Toxic – metabolic causes
- Ethylene glycol, methanol, thiamine deficiency
- Hysteria
**Probably helpful to think through this using VITAMIN C-D or from front to back anatomically
Vitreous hemorrhage
- Bleeding into the preretinal space
- Etiology:
- Diabetic retinopathy
- Retinal tears
- Sickle cell disease
- Age related macular degeneration
- Symptoms
- Floaters, “cobwebs” in the visual field, painless
- Signs
- Black or red haze on ophthalmoscopy
- NO RAPD
- Treatment
- Bed rest, elevated head of bed
- NO anticoagulation
- May need laser photocoagulation or retinal tear repair
Macular Disorders
- ERP’s role is to recognize macular disease
- Degenerative, radiation related, vascular, infectious, idiopathic
- #1 cause : age related macular degeneration
- Symptoms:
- “Loss of central vision” with preserved peripheral vision
- Gradual to rapid visual loss
- Signs
- Scattered drusen leading to scar and detachments
- Treatment
- Intraocular antivascular endothelial growth factor
- LASER photocoagulation
- Infectious or inflammatory causes need URGENT ophtho referral
13) List 8 RFs for and describe the management of CRAO
Central Retinal Artery Occlusion
- PAINLESS, loss of vision over SECONDS
- Internal carotid –> ophthalmic artery (first intracranial branch of the internal carotid artery)–> Central retinal artery (first infraorbital branch).
- 50-70 yr old. with carotid artery disease,
- HTN, Cardiac dz, diabetes, collagen dz, vasculitis, valvular heart disease, sickle cell disease, glaucoma, retrobulbar hematoma (IIOP), endocrine exophthalmos,
- Signs:
- Reduced VA, prominent RAPD, pale edematous fundus with a CHERRY RED SPOT
- Treatment:
- Digital global eye massage in the ED (10-15 sec. of pressure, then release — to dislodge the clot)
- ? inhaled carbogen (95%o2, 5% Co2) to cause retinal artery vasodilation
- Timolol 0.5% eye drops
- Acetazolamide to lower intraocular eye pressure and increase retinal blood flow
- ? role for IV tPa – variable but trendingly positive evidence
- Treat underlying thrombotic disease
- ? local intra-arterial thrombolytic therapy in less than 6 hrs of onset
- bottom line: conflicting evidence for thrombolytics–used depends on clinical situation
- Intraocular paracentesis of the anterior chamber by optho?
Central Retinal Vein Occlusion
- Painless loss of vision
- “blood and thunder’
- Usually unilateral
- Vision loss ranges:
- 20/40 –> hand motion
- Two types:
- Ischemic
- Marked vision loss with RAPD
- Non-ischemic
- Less severe visual loss
- Treatment:
- Lower IOP
- Topical steroids
- Intraocular anti vascular growth factor
- LMWH
- Ischemic
14) List 6 RFs for retinal detachment
Retinal breaks / Detachment
- Retina: two layers
- Inner neuronal retina
- Outer retinal pigment epithelial layer
- Both can be separated by aqueous humour
- Three mechanisms:
- Rhegmatogenous
- #1 cause: tear or hole in the neuronal layer leading to fluid from the vitreous cavity to leak between the layers
- Common in >45 yr olds. men> women
- Exudative retinal detachment
- Fluid or blood leakage from vessels within the retina to cause tear
- HTN, Toxemia of pregnancy, CRVO, glomerulonephritis, papilledema, vasculitis, choroidal tumour
- Traction retinal detachment
- Fibrous band formation in the vitreous and contraction of these bands from prior vitreous hemorrhage
- Symptoms:
- Flashes of light (traction on the retina)
- Floaters (vitreous blood and pigmented debris)
- Visual loss “filmy, cloudy, curtain-like”
- PainLESS
- Visual field cuts with varying visual loss
- Signs
- CANNOT be ruled out by fundoscopy
- Needs indirect ophthalmoscopy
- Bedside U/S
- Treatment:
- Optho CALL!
- Needs urgent surgical repair especially to prevent further macular detachment
- Ideally in 24-48 hrs
- Exudative retinal detachment needs photocoagulation
- Fluid or blood leakage from vessels within the retina to cause tear
- Rhegmatogenous
Posterior vitreous detachment
- In >60 yr olds
- Vitreous gel pulls away from the retina
- Similar symptoms to retinal detachment and vit. hemorrhage and retinal breaks
- Treatment
- No specific treatment unless associated with retinal detachment or vitreous hemorrhage
- Need referral to differentiate between these entities
15) Describe the presentation of optic neuritis and its management
Optic neuritis
- Acute monocular vision loss caused by focal optic nerve demyelination
- 15-45 yrs
- Symptoms:
- Progressive loss of vision over several hours to days
- Ocular PAIN with eye movement
- Ranging visual loss: minimal to blindness
- Signs
- +RAPD
- Swollen optic disc or normal
- 30% develop multiple sclerosis in 5 years
- Treatment
- IV or PO steroids temporarily improve vision in a few weeks but have NO impact on long term outcome or visual acuity
- Observation = treatment with steroids
16) Describe the presentation of temporal arteritis and its management
Ischemic Optic Neuropathy
- Most common cause of visual loss in later age
- Related to giant cell arteritis (TA)
- Wt loss, fevers, jaw pain, scalp tenderness, malaise, headache, visual loss, painless visual loss, age >50, hx of PMR,
- Or idiopathic
- Related to giant cell arteritis (TA)
- Often have a history of amaurosis fugax
- Signs:
- RAPD
- Visual loss,
- Visual field defect
- Pale optic disc,
- Tests:
- Elevated ESR
- Corrected for age (age/2 ; age+10/2 for women)
- Temporal biopsy
- Elevated ESR
- Treatment
- High dose steroids as soon as the diagnosis is suspected
- Better outcomes with IV methylprednisolone
- Bx within 1 week of diagnosis
- High dose steroids as soon as the diagnosis is suspected
Non-arteritic Ischemic Optic Neuropathy
- Much more common than optic neuritis
- No classic symptoms of Giant Cell Arteritis, normal ESR
- Most people have
- Systemic vascular dz ; diabetes; HTN ; younger
- Signs & Symptoms
- Painless visual loss, RAPD, disc swelling,
- Treatment
- Mixed results with steroids, as improvement normally occurs in 1/3 of pts
17) What are the classic visual field defects in chiasmal and post-chiasmal lesions?
Neuro-ophthalmic Visual Loss
- Any visual loss not readily explained by an abnormal physical examination
- Disease distal to the retina
- Divisions:
- Reduced visual acuity or visual field loss
- Zones:
- Pre-chiasmal
- Decreased VA or visual field loss on the affected side
- OPTIC NERVE PROBLEM
- Swinging flashlight test = an afferent pupillary defect on the side involved unless there is a bilateral process
- Optic neuritis, ischemic optic neuritis, compressive optic neuritis, toxic/metabolic optic neuritis.
- Decreased VA or visual field loss on the affected side
- Chiasmal
- Bitemporal hemianopsia
- Post-chiasmal
- A left occipital lesion will result in RIGHT bilateral visual field blindness
- Pre-chiasmal

Chiasmal Visual Loss
- Due to pituitary tumors or meningioma
- Progressive and gradual visual loss
- “Bi-temporal ” classically
- But most compress the optic chiasm and optic nerves asymmetrically
Post-Chiasmal Visual Loss
- Due to infarction, tumor, AVM, migraine disorders
- Usually unable to perform a specific task
- Classically “homonymous hemianopsia” –e.g. bilateral right sided visual field loss
- Also may present with cortical blindness (usually have another neurologic deficit) due to bilateral occipital infarction
- Often incorrectly ASSUMED to be functional in nature
18) What is Anton’s syndrome?
“Anton’s syndrome is characterized by bilateral blindness, normal pupillary reflexes, bilateral occipital lesions, and, interestingly, denial of blindness. It is this denial of blindness that may be incorrectly assumed to be evidence for a functional process.” – Rosen’s
They actually have bilateral occipital lobe lesions!
[bg_faq_end][bg_faq_start]19) Differentiate between visual loss from hysterical conversion and malingering. What are two tests to discern between these and organic causes?
Functional Visual Loss
- 1) Hysterical conversion reaction – non deliberate
- Flat affect, no emotional disturbance despite blindness
- 2) Malingerer: usually overly emotional reaction to vision loss
- Normal pupillary reflexes, no RAPD, normal fundoscopy
- Test:
- Hesitant to oppose index fingers
- Write their names in an obviously disorderly fashion (a blind person can write their names neatly)
- Mirror test: having the person follow their eyes as the mirror is tilted
- Optokinetic nystagmus
20) List 5 DDx for anisocoria. Which are greater in dark, and which are greater in light?
Anisocoria
- Clinical features:
- In the setting of trauma or dec. LOC : requires immediate neuro-imaging or intervention — > inc. ICP
- In lighted setting: the problem pupil is the LARGER one
- In a dark setting: the problem is the the SMALLER one
- In a normal afferent visual system – there is likely an iris defect
- Can occur in the setting of seizures as well
| Condition
| ADIE’s Tonic pupil syndrome | Pharm. induced Mydriasis | Third Nerve palsy | Physiologic anisocoria | Horner’s syndrome |
| Clinical features
| blurred near vision, normal far vision. young women – 70% reduced DTR’s | inadvertent phenylephrine/cocaine: atropine/scopolamine | need neuroimaging “more obvious in light” | 20% of people > 0.4 mm may be transient, or alternate | ipsilateral: PTOSIS, MIOSIS, Facial ANHIDROSIS |
Notes | poor accommodation to close vision (trouble reading) caused by a viral or bacterial infection of the parasympathetic system. Triad: anisocoria, loss of knee or ankle DTR’s, impaired sweating Treated by optho with cholinergic agent therapy | ****Look for transdermal scopolamine patches used for motion sickness!!***** diagnosed when 1% pilocarpine has NO miosis effect on pupil size. | Increases in light, usually have: ● PTOSIS ● EOM DYSFUNCTION ● DIPLOPIA when 1% pilocarpine instilled the pupil constricts! | increases in darkness NO dilation lag NO loss of vision NO Diplopia | YES dilation LAG–up to 15 secs caused by: ● strokes ● tumors ● lung CA ● thyroid adenomas ● pancoast’s tumours ● headache syndrome ● carotid dissection ● herpes zoster ● otitis media ● trauma to brachial plexus during delivery Inadvertent anesthetic administration into carotid sheath during dental block…! |
21) What is Horner’s syndrome? List 8 DDx.
| Horner’s syndrome: Due to an interruption of sympathetic innervation |
| Ipsilateral: PTOSIS, MIOSIS, Facial ANHIDROSIS |
| YES dilation LAG of the pupil– needing up to 15 secs to dilate with light Caused by: ● strokes ● tumors ● lung CA ● thyroid adenomas ● pancoast’s tumours ● headache syndrome ● carotid dissection ● herpes zoster ● otitis media ● trauma to brachial plexus during delivery Inadvertent anesthetic administration into carotid sheath during dental block…! Requires a fairly comprehensive workup; urgency is determined by patient clinical status |
22) What are the fundoscopic findings of papilledema? List 8 DDx
- Swelling of the optic nerve head
- Blurring of the disc margins
- Hyperemia
- Loss of physiologic cupping

Abnormal optic disk
- Papilledema:
- Increased ICP
- The subarachnoid space is continuous with the optic nerve sheath
- SAH
- Tumor
- Idiopathic intracranial hypertension
- Brain abscess
- Meningitis
- May have normal vision
- May have NO headache!
- Usually a bilateral process
- The subarachnoid space is continuous with the optic nerve sheath
- CRVO
- Hypertensive retinopathy
- Optic disk vasculitis
- Increased ICP
23) List 7 DDx for binocular diplopia
- Basilar Artery Thrombosis / enlarging aneurysm – V
- Botulism / Basilar Meningitis – I
- Vertebral Dissection – T
- Myasthenia Gravis / MS / Graves disease / Miller-Fisher Syndrome – A
- Wernicke’s Encephalopathy – M
- Orbital myositis / Ophthalmoplegic migraine – I
- Orbital Apex Syndrome / Cavernous Sinus Process / Brainstem Tumour- N
24) Describe the findings in CN III, IV, and VI palsies + list 2 causes for each
Disorders of EOM
- Report DIPLOPIA
- LR – 6 (lateral movement)
- SO – 4 (contralateral down and in)
- CN 3 all the rest
- Monocular
- Less severe
- Causes
- Refractive errors
- Dislocated lens
- Iridodialysis
- Feigned
- Binocular
- ***Disappears with either eye covered***
- Causes:
- Hematoma
- Orbital floor fractures
- Abscess
- ****#1 cause: palsy of cranial nerve 3,4, or 6***
- Usually decreased LOC, focal findings
- 3rd nerve palsy
- Ptosis, unable to turn eye inward/upward
- Mydriasis (II into brain, III out to eye)
- Non-ischemic optic neuropathy (due to diabetes); orbital apex mass/tumour
- 4th nerve palsy
- Diplopia worse with downgaze
- Head tilt the opposite way
- Trauma or vascular disease (aneurysm)
- 6th nerve palsy
- MOST common
- Esotropia worse with lateral gaze
- Turning of head towards paretic side
- Wernicke’s, aneurysms, neoplasm, vascular disease, trauma, MS, meningitis, thyroid disease, increased ICP
- Thyroid disease
- Progressive ophthalmoplegia
- EOM muscle fibrosis
- MS
- Myasthenia gravis
This post was uploaded and copyedited by Colin Sedgwick (@colin_sedgwick)