This episode of CRACKCast covers Rosen’s Chapter 63, Thermal Burns. These patients are often the sickest in the department and many are on their way to the ICU. There are life-saving interventions that are begun in the emergency department with significant impacts on morbidity and mortality, and many are discussed in this episode.
Shownotes – PDF Here
[bg_faq_start]Rosen’s in Perspective
- Tissue destruction caused by contact with heat, electrical current, radiation, or chemical agents
- Temperatures below 44 C are generally tolerated for long periods of time without injury
- Temperatures above 60 C cause protein denaturation in tissue
- Burn progression is a result of both necrosis and apoptosis of damaged cells
- The necrosis – passive process denaturing the lipid bilayer and ATP enzymes. Leading to cell swelling, loss of energy stores, and massive release of inflammatory mediators.
- Let’s talk epidemiology!
- Young and old have thinner skin and fewer sweat glands/hair follicles – hence more susceptible to injury
- 450,000 burn injuries treated in the United States each year, 3500 deaths
- Most commonly from residential fires
- 5% – 35% of patients hospitalized with burns will have inhalational injury
- 44% from flame exposure, 33% from scalding, 9% direct conductive burns from hot objects, 4% electrical burns, and 3% chemical burns.
- Overall survival rate 95%.
- Most commonly affected are upper extremities (41%, think grabbing), then lower extremities (26%), and head and neck (17%)
[1] List zones of burns
Three concentric zones of a burn used to explain the pathophysiology of a burn.
Listed from the center out they are:
- Irreversible coagulation and necrosis, formed immediately.
- Ischemia with impaired microcirculation. This tissue is at risk of subsequent necrosis – this is what we want to increase the perfusion to! Unfortunately none of the researched therapies have proven to be beneficial in Vivo….yet!
- Transient hyperemia
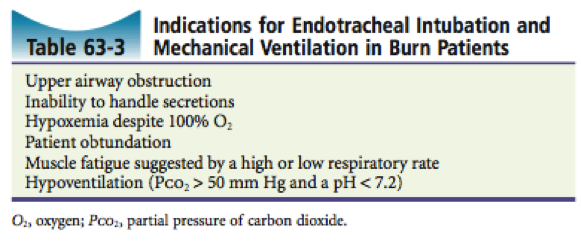
[2] List 6 indications for intubation in the burn patient
- Upper airway obstruction
- Inability to handle secretions
- Hypoxemia despite 100% O2
- Patient obtundation
- Muscle fatigue suggested by high or low respiratory rate
- Hypoventilation (PCO2 > 50 mmHg and pH < 7.2)
- Direct thermal injury – rarely happens below the vocal cords, but the smoke byproducts (chemical injury) lead to V/Q mismatch and pulmonary edema.
- Both cause upper and lower airway edema
- Shedding necrosis of the mucosa leading to a cascade of dysfunction in all parts of the pulmonary system leading to ARDS
- Consider intubating early in patients who may look otherwise well but who are at high risk of developing complications of airway burns.
- e., patients with oropharyngeal swelling and a hoarse voice
- Remember that circumferential neck eschar can compress the neck, and hence neck vessels and trachea. Escharotomy may be necessary prior to intubation.
- Both cause upper and lower airway edema
[3] List and describe 2 formulas for fluid resuscitation
- Rosen’s lists 8 different fluid resuscitation formulas in Table 63-5.
- Parkland formula – most commonly known, probably over-resuscitates patients
- Lactated Ringers 4cc/kg/% TBSA burned
- Give ½ of the fluid in the first 8 hours, remainder in the next 16 hours
- Over the following 24 hours, 20-60% of patient’s plasma volume, titrating to maintain urine output of 0.5-1.0 cc/kg/hr (target 1.0 cc/kg/hr in children)
- The modified parkland uses the same formula, but gives the fluid over a 24 hr period
- In BC we use a modification of the Parkland formula:
- Ringer’s lactate 3 ml/kg/% TBSA – and give the first ½ over 8 hours:
- In addition, the Lund-Browder estimation chart is used rather than the rule of nines
- http://www.bcmj.org/articles/provincial-clinical-practice-guidelines-management-major-burn-trauma
- Galveston formula – preferred for pediatrics
- Lactated Ringers at 5000 cc / m2 TBSA burned + 2000 cc/m2 BSA
- g. 10% TBSA burns in a 100 cm child, weighing 15 kg has a body surface area of: 0.64 m2
- 5000 cc/m2 TBSA burned x 0.64 m2 TBSA x 10% burned = 320 cc
2000 cc/m2 TBSA x 0.64 m2 = 1280 cc
So give LR 320 cc + 1280 cc = LR 1600 cc total
- Give ½ of the fluid in the first 8 hours, remainder in the next 16 hours
- 800 cc in 8 hrs = 100 cc / hr for 8 hours
THEN
800 cc in 16 hrs = 50 cc / hr for 16 hours
- 800 cc in 8 hrs = 100 cc / hr for 8 hours
- Use a tool to estimate skin surface area
- Over the following 24 hours, 3750 cc/m2 TBSA burned + 1500 cc/m2 TBSA
- Lactated Ringers at 5000 cc / m2 TBSA burned + 2000 cc/m2 BSA
- Pearls:
- Infants should also receive 5% glucose in their maintenance fluid as the lack carbohydrate reserves.
- Colloids are usually started after the initial 12-24 hrs
- Some studies suggest that non-shocky adult patients with < 20% TBSA can be treated with oral fluids only
- Inhalational injuries need 30-60% more fluid
- Remember that the goal is: organ perfusion!
- This can be indirectly assessed by vital signs, level of consciousness, cap refill, urine output goal of 1 ml/kg/hr
[3] Describe depth classification for burn injuries

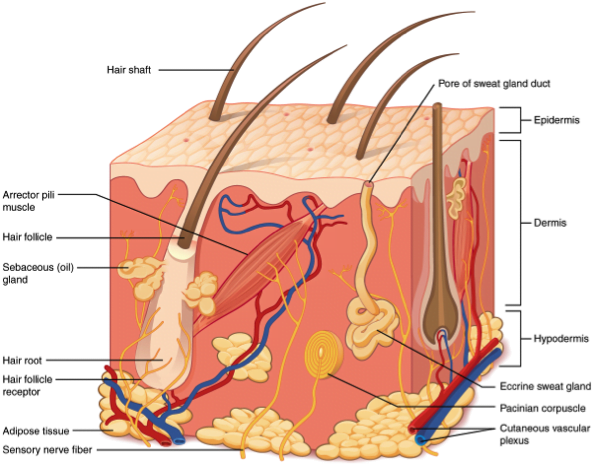
Image from Wikipedia: Skin Layers
- First Degree
- Limited to epidermis
- Painful, erythematous, dry surface
- Heal in days
- The skin’s ability to heal is limited to ~1cm from the uninjured epidermis and the degree of damage to sebaceous glands/hair follicles
- Second Degree: “moist, painful”
- Involves epidermis and extends into dermis
- Superficial Second Degree
- Involve only the papillary dermis
- Painful, erythematous, blisters, blanches with pressure, moist surface
- Heal in 2-3 weeks
- Deep Second Degree
- Extends into reticular dermis
- Painful, white or only mild erythema, hemorrhagic blisters, minimal blanching, dry or moist surface
- Heal in 3+ weeks, or can progress to 3rd degree burns
- In Kids: these can lead to severe scarring and contractures – and need excision and skin grafting if not healed by day 21.
- Third Degree
- Full-thickness – extend through entire dermis
- Stiff, white or tan colour, dry, leathery and insensate
- Require excision +/- grafting
- Fourth Degree
- Extend full-thickness and through subcutaneous fat to involve muscle or bone
- Stiff, charred skin
- ****Accuracy in ED of establishing burn depth is 50-75%. Patients need serial exam and monitoring.****
- Burn progression is dynamic and can worsen.
[5] List indicators of upper airway and lower airway burns
Be aware, these signs are only moderately sensitive or specific.
Upper airway (supra-glottic):
- Soot in and around nose/mouth
- Charring
- Mucosal inflammation or necrosis
- Edema
Lower airway (subglottic):
- Wheezing
- Crepitations
- Hypoxemia
- Abnormalities on chest x-ray
- V/Q mismatch, decreased lung compliance, microatelectasis -> ARDS
The classic: facial burns, singed nasal vibrissae, carbonaceous sputum and history of a burn in an enclosed space are neither highly sensitive/specific.
- The true dx requires: direct visualization with fibroscopy before / after intubation….showing:
- Soot, charring, mucosal inflammation, edema, necrosis
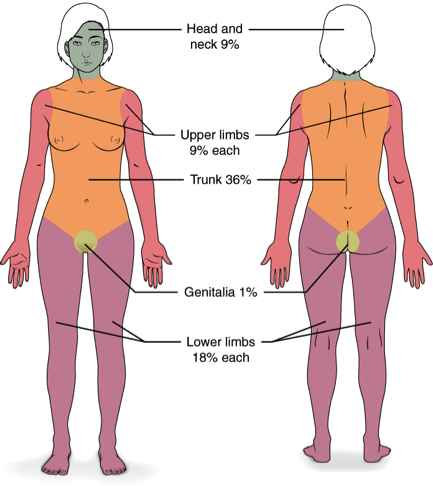
[6] What is the Rule of 9’s and how is it modified in pediatrics
- Back in the day, most people died from hypovolemic shock and renal failure
- Major extravasation into the interstitial spaces
- Rule of 9s is used to quickly estimate TBSA burned.
- Some studies have shown that patients with less severe burns have their TBSA overestimated, while patients with more severe burns have their TBSA underestimated.
- Small burns can be estimated as 1% TBSA for each area burned the size of the patient’s hand (palm and fingers)
- May be better to sit down and use a burn chart, measuring carefully, if time permits.
Images from Wikipedia:
- % TBSA is allocated as:
- 18% for front of trunk (9% torso, 9% abdomen)
- 18% for back of trunk (9% upper back, 9% lower back)
- 18% for an entire lower extremity
- 9% for the entire head
- 9% for each upper extremity
- 1% for the perineal area
- Children have relatively larger heads, smaller thighs, and smaller lower legs
- A Lund-Browder chart can be used to estimate TBSA burned in children

[7] List criteria for transfer to burn unit
- Large burns (> 20% TBSA burned in adults, > 10% TBSA burned in children or elderly)
- Deep burns (> 5% full-thickness)
- High-voltage burns
- Burns over sensitive areas (e.g. face, ears, joints, perineum, hands, feet)
- Escharotomy required
[8] Describe basic burn dressing management
- ABC’s
- Analgesia, analgesia, analgesia
- Prevent hypothermia!
- Assume burns are contaminated: clean and debride gently
- Tetanus toxoid booster if eligible (>5 years since last)
- If the patient did not complete primary series, TIG
- Leave blisters intact, debride ruptured blisters
- Dressings for partial-thickness burns
- Clearly infected, purulent wounds should be managed in an ‘open’ manner
- Topical antimicrobials (e.g. neomycin, mupirocin, silver sulfadiazine)
- Nonadherent dressing
- Daily dressing exchange and gentle cleansing with water and soap
- The second method for burn management is with occlusive dressings
- Support a moist wound-healing environment
- Less pain as dressings are not exchanged daily
- Most appropriate for superficial partial-thickness burns with no signs of infection
- Dressing such as Mepilex or a nano-crystaline silver-containing occlusive dressing should be applied and left in place for approximately 1 week
- Avoid silver sulfadiazine if transferring patient to a burn center as it can alter the appearance of the burn
- Clearly infected, purulent wounds should be managed in an ‘open’ manner
[9] List 5 burn prevention strategies
- Flame burn prevention
- Secure matches and lighters where they are inaccessible to children
- Safety device around fireplace
- Create home escape plan and practice with family
- Check that smoke detectors are functional
- Scald prevention
- Use splash guards on stove
- Use thermometer on bathwater
- Lower hot water heater maximum temperature to 49-54 C
Wisecracks
[1] What are the indications for an escharotomy
- Circumferential chest or neck burns with:
- Increased airway pressures
- Hypoxemia
- Difficulty with ventilation
- Circumferential extremity burn with:
- Decreased doppler signal distally
- Pulse oximetry of less than 90% distally in the limb (one study)
- Pain, loss of sensation, delayed cap refill (early signs)
[2] What are the primary considerations in mechanical ventilation of burn patients
- Intubation
- RSI unless there is suspicion of airway obstruction
- If there is concern of airway obstruction, awake intubation with analgesia and sedation should be performed
- While succinylcholine is commonly avoided in burn patients, recall from Chapter 1 that it is only contra-indicated in patients who are 5 or more days post-burn
- Mechanical Ventilation
- Avoid barotrauma – limit plateau pressure to 35 mmH2O
- This may mean permissive hypercapnia, maintain pH > 7.25
- PEEP can be helpful
- Minimize FiO2, maintaining an SpO2 of > 92%
- Low tidal volume ventilation (6-8 cc/kg IBW)
- Avoid barotrauma – limit plateau pressure to 35 mmH2O
- Adjuncts
- Bronchodilators can be helpful in wheezing patients
- Chest physiotherapy and airway suctioning for secretion management
- Don’t forget about concomitant CO and cyanide intoxication!
This post was uploaded and copyedited by Riley Golby (@RileyJGolby)