This episode of CRACKCast covers Rosen’s Chapter 35, Back Pain. This chapter covers a diagnostic approach to a common ED complaint, with emphasis on the red flags you cannot miss, as well as an approach to treatment.
Shownotes – PDF Here
[bg_faq_start]1) List 10 historical red flags for back pain
Red flags on History and Physical Exam
- History
- Fracture risks:
- Trauma history
- Prolonged steroid use
- Frail, old, osteoporotic, over 70 years with or without MINOR trauma
- Smoking guns (historical)
- Syncope
- Children
- Acute onset with flank, testicular, or abdominal/back pain
- Diaphoresis
- Neurological deficits
- Cancer risks:
- Cancer history, weight loss, constitutional symptoms
- Worse at night or at REST
- Infection risks
- Immunocompromised, IVDU
- FEVER
- Fracture risks:
- Physical exam
- Vitals
- Hypo or hypertension, tachycardia, fever
- Unequal blood pressures in extremities
- Stethoscope
- Aortic insufficiency murmur – diastolic
- Palpation
- Circulatory compromise in lower extremities or pulse deficits
- Pulsatile abdominal mass
- Focal bony tenderness
- Neurological exam
- Urinary retention
- Loss of rectal sphincter tone (incontinence)
- Focal lower extremity weakness
- Vitals

2) List 6 emergent causes of back pain
See box 35-1 in Rosen’s (listed below)
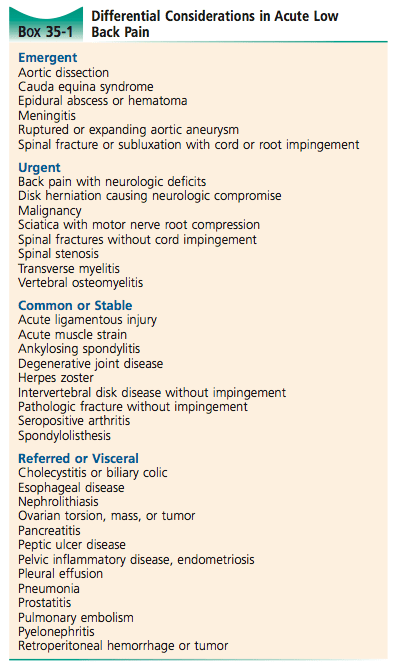
Emergent causes of back pain:
- Aortic dissection
- Cauda equina syndrome
- Epidural abscess / HEMATOMA
- Meningitis
- Ruptured or expanding abdominal aortic aneurysm
- Spinal fracture with subluxation causing CORD or ROOT impingement
Wisecracks
[bg_faq_start]1) Describe the most common sites of disc protrusion with their associated neurologic findings
Disc Protrusion and Signs:
Pathophysiology
- Systems involved:
- Vascular
- Visceral
- Infectious
- Mechanical
- Rheumatologic
- Anatomy to think through: spinal column, cord, root, muscles,
- Spinal cord ends at L1
Disc herniation
Normally the nucleus pulposus (gelatinous) is enclosed by the annulus fibrosus. With aging the annulus thins posteriorly which can lead to HERNIATION.
- Protrusion — extrusion — sequestration
- 95% of herniation occur at L4-S1 spaces – with associated radicular symptoms
- L5: decreased sensation to first webspace in foot
- Weak extension of the great toe and NORMAL reflexes
- S1
- Decreased sensation to lateral foot and small toe
- Weak plantar flexion and +/- ankle jerk reflex loss
- Disk extrusion – is usually symptomatic, the others usually are NOT
- L5: decreased sensation to first webspace in foot
- ⅔ resolve in 6 months on MRI
- 75% of people’s symptoms improve in 6 weeks
- If spinal stenosis, it worsens over time
- Imaging is NOT indicated unless cauda equina suspected / other risks / long course
- Compression above L1 = UMN findings
- Compression below L1 = LMN findings
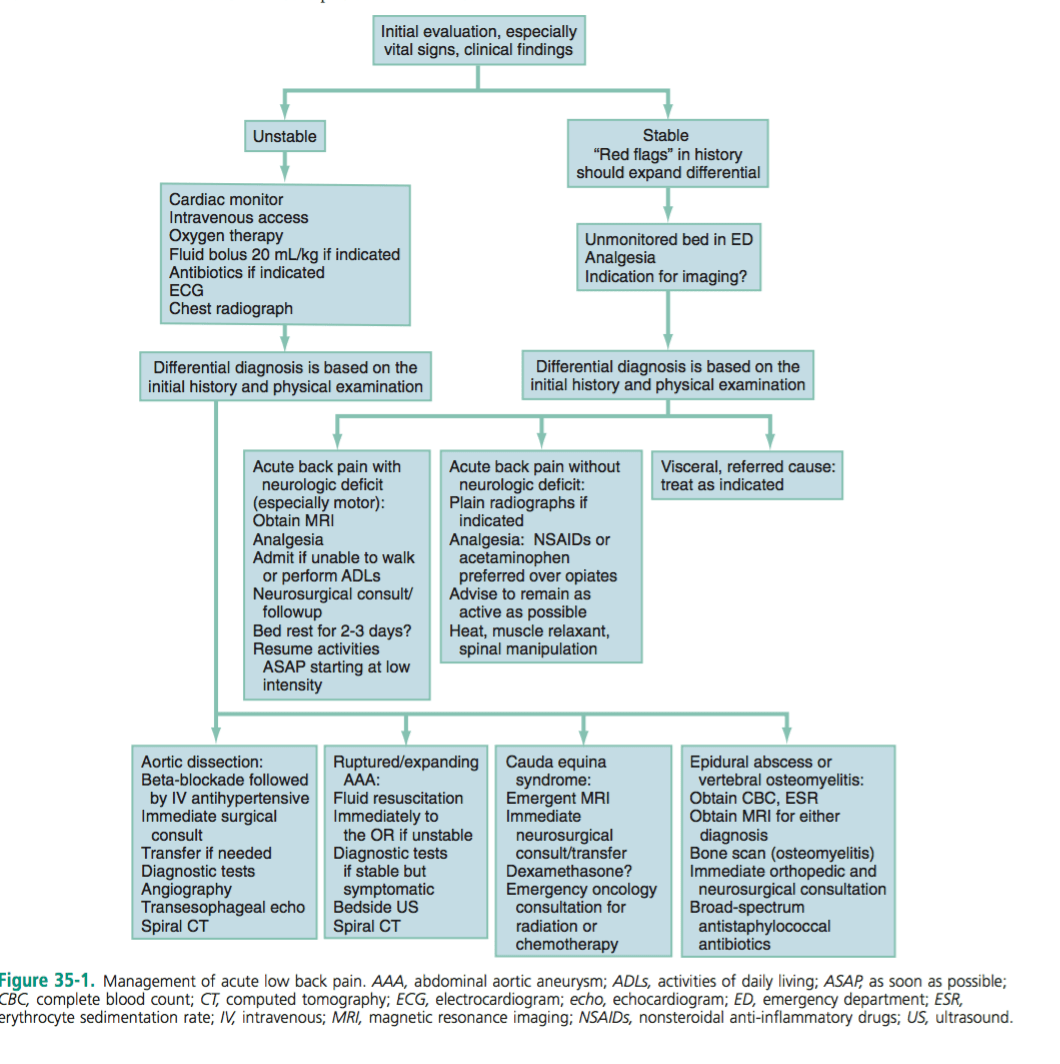
2) Outline your approach to acute undifferentiated back pain
3) Describe your treatment approach for acute musculoskeletal low back pain
Empirical management
- Depends on presenting vitals signs and degree of illness – see fig 35-2
- If unstable: based on fig 35-1
- If stable:
- Severe pain:
- IV narcotics
- With transition to PO narcotics
- Moderate pain
- Tylenol and advil
- NSAIDS are NOT superior to tylenol and risks must be considered (patient factors!)
- IV narcotics
- Severe pain:
- Benzo’s:
- “Anxiolytic and sedative properties may promote sleep and synergize pain relief…”
- But dangerous
- Muscle relaxants:
- NO credible evidence supporting muscle relaxants or antispasmodic agents
- Methocarbamol or cyclobenzaprine
- Heat, spinal therapy, acupuncture, TENS
- Other therapies through family doctor:
- Gabapentin, TCAs, injections
- NEED a multidisciplinary approach to acute on chronic spells of back pain!
- NO credible evidence supporting muscle relaxants or antispasmodic agents
This post was uploaded and copyedited by Colin Sedgwick (@colin_sedgwick)


