Alan Garner is a 38-year-old single, unemployed, Caucasian male, with a medical history of ADHD who has voluntarily arrived at the ED accompanied by friends Stu and Phil after being punched in the face while trespassing. Despite having a poor recollection of the night’s events, Alan and friends are certain that he received a sucker punch by none other than Mike Tyson, the former undisputed world heavyweight boxing champion.
Phil informs you that, after receiving a right hook to the left eye from Iron Mike, Alan fell to the floor from standing height. Stu notes that Alan became unresponsive once he hit the ground, however, regained consciousness within 1-2 minutes. He goes on to say, “at no point did Alan stop breathing” and that “Alan’s recovery was spontaneous and he’s pretty much back to his 14-year-old self… which is as good as it’s going to get.” Alan is complaining about his bruise which he says hurts a lot. He also notes that he has constant blurry vision in the left eye and double vision when he tries to look left or right. He does not have any other complaints and his vital signs are normal.
Physical Exam
On primary survey, you note Alan is speaking and breathing comfortably, he is alert, oriented, and responsive. His Glasgow Coma Scale score is E4V5M6 although his left eye responses cannot be recorded due to his localized injuries. His clothing is removed, and you offer him a gown and warm blankets but notice he is holding tightly to his purse. You politely ask him to put the purse aside and he yells at you “this is a SATCHEL mister”. His vitals are stable and within normal range. Heart sounds are normal with no murmurs. He has equal air entry bilaterally with no adventitious sounds. His left peri-orbit is markedly swollen and erythematous; however, no superficial bleeding is noted.
The secondary survey is largely unremarkable aside from his neurological and ocular examination which reveals a left relevant afferent pupillary defect, ophthalmoplegia and moderate proptosis of his left eye. Visual acuity in his left eye is 20/60.
What steps should be taken in the ED?
Discussion
Three percent of all emergency department visits are associated with traumatic eye injuries, however, in larger academic centres, trauma induced injury to the eye may represent up to 23% of all visits.1,2 Common causes of traumatic eye injury include assault, sports, industrial work, flying objects (bullets, darts, fireworks, bungee cords, etc.), and chemical splashes.3 40% of monocular blindness is associated with trauma, so it is important to recognize eye injury patterns and treat these patients efficiently and appropriately.4 It is also important to recognize that visual symptoms are often associated with traumatic brain injuries (TBI).5 In fact, amongst patients with mild TBI 74% had associated visual symptoms.6 For this reason, physicians should look for signs of head injury when patients present with ocular complaints of traumatic origin. Common signs of TBI can include feeling slowed down, difficulty concentrating, memory lapses, nausea, vomiting, and emotional changes.7
What is acute orbital compartment syndrome and why do we care?
It is crucial that Emergency Physicians be aware of acute orbital compartment syndrome (OCS).8 OCS is characterized by a swift increase in the intra-orbital pressure resulting in decreased perfusion to the retina and optic nerve.8,9 OCS most commonly occurs as a result of orbital haemorrhage secondary to trauma and can rapidly precipitate permanent vision loss.8,9 Less common causes of OCS are iatrogenic in nature and have been documented secondary to ophthalmic surgery as well as retrobulbar injections during anesthesia.10,11 Non-ophthalmic procedures such as sinus surgery, craniofacial surgery and neurosurgery can also bring about OCS.12–14 Other important aetiologies include orbital cellulitis, intraorbital abscess, orbital emphysema, foreign material within the orbit and tumours.8 The differential diagnoses include autoimmune orbital inflammation, thyroid ophthalmopathy, progressively enlarging masses and a ruptured dermoid cyst.8 Globe perforation commonly occurs with traumatic eye injury and dramatically alters management; therefore, it is important to rule out whenever OCS is suspected.8 Slit lamp findings suggestive of globe rupture include defects of conjunctiva, visible foreign bodies and lacerations. In addition, attention should be paid to pupil shape and peripheral sclera overlying extraocular muscle insertion, which is the most common point of rupture.15 Never measure IOP or perform lateral canthotomy and cantholysis in a patient with suspected globe perforation.8
When should I be suspicious of OCS?
OCS is a clinical diagnosis based on history, symptoms and signs rather than laboratory abnormalities and imaging.8,16 For this reason, recognizing the clinical presentation of OCS is crucial to diagnosing this ocular emergency. Hallmark findings of OCS are a relevant afferent pupillary defect (RAPD), reduced visual acuity, ophthalmoplegia, proptosis, and eye pain.8 When IOP is above 30mmHg, OCS is more likely, however, IOP by itself is not diagnostic for OCS and should not sway management as no consensus has been made.16–18 Palpation of the orbit reveals a tense orbit which resists globe retropulsion.16 Of note, OCS causes RAPD and not a fixed dilated pupil.16 RAPD is a key finding as it is indicative of optic nerve damage. Periocular tenderness, ecchymosis and edema may be marked.8 Fundoscopic examination may reveal optic disk or retinal oedema, retinal venous congestion, central retinal occlusion, or arterial pulsations.8
Should we request imaging for OCS?
The recognition and initial management of acute OCS in the emergency department should occur without imaging.1 Once primary treatment has occurred, thin-sliced helical orbital CT should be performed to identify the source of OCS and direct treatment.1,8
How do we treat OCS in the emergency department?
The most effective treatment occurs within 2 hours of injury onset and is best performed by an Ophthalmologist.16,19 If an ocular specialist is unavailable, Emergency Physicians should proceed with lateral canthotomy and cantholysis as this procedure is the most effective treatment for OCS.20,21 Lateral canthotomy and cantholysis can be performed at the bedside with local anaesthesia and, if performed correctly, results in immediate decrease of IOP as the eye moves forward.8,22,23 The major risks of lateral canthotomy and cantholysis include iatrogenic globe injury, damage to the lacrimal glands, lacrimal artery, and levator aponeurosis.23 Minor risks include bleeding, infection and iatrogenic ectropion.23
Required equipment for lateral canthotomy and cantholysis:
Sterile gauze, gloves and drapes. Antiseptic solution. Topical ocular anesthetic (0.5% proparacaine or tetracaine eyedrop), local anesthetic (1% or 2% lidocaine with epinephrine), small injection needles, small syringe, ophthalmic antibiotic ointment (erythromycin 0.5% or bacitracin), normal saline for irrigation, haemostat, toothed forceps and iris scissors.
Step by step description of lateral canthotomy and cantholysis:
- +/- Intravenous mannitol 20% 2g/kg OR acetazolamide 250mg OR methyl prednisone 250mg
- Irrigate area of lateral canthus
- Clean skin surrounding eye with antiseptic. Do not allow antiseptic to enter eye.
- Inject local anaesthetic into lateral canthal incision site
- Use haemostat to crush tissue from lateral canthus to rim of orbit (1-2cm). Hold for 1-2 minutes.
- Use iris scissors to cut from lateral canthus to rim of orbit. Note: Always aim scissors inferoposteriorly toward lateral rim
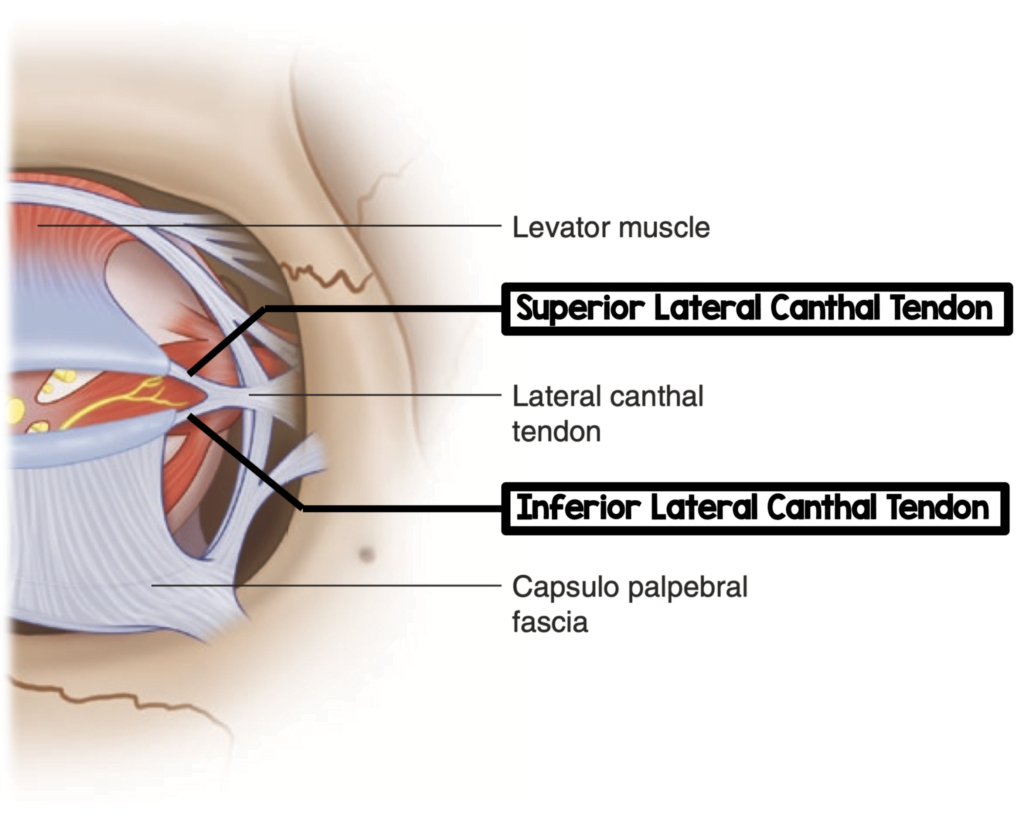
- Fold open lateral portion of lower eyelid to reveal underlying lateral canthal ligament.
- Cut the inferior crus of lateral canthal ligament. Note: This ligament can be identified by “strumming” with scissors pointed away from eye. Ligament will feel like a plucked guitar string. Always aim scissors inferoposteriorly toward lateral rim.
- Measure IOP
- If necessary, cut superior crus
- Apply antibiotic ointment to eye and cover with sterile dressing
In cases where surgical decompression is not possible or when increased IOP persists post decompression, physicians should consider the use of intravenous mannitol (20% 2g/kg), acetazolamide (250mg), and/or methyl prednisone (250mg) in consultation with ophthalmology.23,24 The ongoing usage of thrombolytic and/or anti-platelet/ anti-coagulants by the patient should be recorded and adjusted as appropriate based upon the risks and benefits to individual patients.8
Words are great, but I’m a visual learner! Lateral canthotomy procedural video
What will the Ophthalmologist do?
As retrobulbar haemorrhage is the most common cause of OCS, Ophthalmologists may need to perform anterior orbitotomy and drainage to evacuate a hematoma.8,23 Additionally, Ophthalmologists will ligate or cauterize bleeding vessels.24 A follow up appointment is usually booked several days post lateral canthotomy and cantholysis to close the incision and monitor the healing process.25
What else should be considered in this patient prior to discharge?
Recognizing the signs and symptoms of OCS, you inform Alan of your diagnoses. He agrees to undergo lateral canthotomy and cantholysis and the procedure is completed successfully under local anesthesia with no complications. He is given analgesics, antiemetics and empiric antibiotics and rushed to the imaging lab where a CT scan of his orbit was completed to determine the source of his OCS. In addition, the CT ruled out concomitant facial fractures which occur commonly in the presence of OCS secondary to trauma. Luckily for Alan, no fracture was noted on CT. Phil and Stu are shocked his brain appears normal on imaging. Having discussed the case with the Ophthalmologist, you are both satisfied with Alan’s outcome in the emergency department and arrange a follow up with the Ophthalmologist as an outpatient in 3 days. The boys thank you for your service and head off reeking of sweat, alcohol and smoke. You wonder if they’ll even remember this hospital visit.
Key-Points
- OCS is a clinical diagnosis
- Never measure IOP in patients with suspected perforated globe
- Never perform lateral canthotomy and cantholysis in patients with suspected perforated globe
- Lateral canthotomy and cantholysis should be performed within 2 hours of symptom onset to significantly decrease the risk of permanent vision loss
This post was copy-edited by @jamievanderende.
References
- 1.Lin KY, Ngai P, Echegoyen JC, Tao JP. Imaging in orbital trauma. Saudi Journal of Ophthalmology. Published online October 2012:427-432. doi:10.1016/j.sjopt.2012.08.002
- 2.Bord SP, Linden J. Trauma to the Globe and Orbit. Emergency Medicine Clinics of North America. Published online February 2008:97-123. doi:10.1016/j.emc.2007.11.006
- 3.Gudgel D, Barry Lee W. Recognizing and Treating Eye Injuries . American Academy of Opthalmology. Published March 4, 2021. https://www.aao.org/eye-health/tips-prevention/injuries
- 4.KUHN F, MORRIS R, MESTER V, WITHERSPOON C, MANN L, MAISIAK R. Epidemiology and socioeconomics. Ophthalmology Clinics of North America. Published online June 2002:145-151. doi:10.1016/s0896-1549(02)00005-6
- 5.Singman EL. Automating the assessment of visual dysfunction after traumatic brain injury. Med Instrum. Published online 2013:3. doi:10.7243/2052-6962-1-3
- 6.Cockerham GC, Goodrich GL, Weichel LED, et al. Eye and visual function in traumatic brain injury. JRRD. Published online 2009:811. doi:10.1682/jrrd.2008.08.0109
- 7.Peterson A, Xu L, Daughtery J, Breiding M. Surveillance Report of Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014. Centers of Disease Control and Prevention; 2019:24. https://www.cdc.gov/traumaticbraininjury/pdf/TBI-Surveillance-Report-FINAL_508.pdf
- 8.Lima V, Burt B, Leibovitch I, Prabhakaran V, Goldberg R, Selva D. Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol. 2009;54(4):441-449. doi:10.1016/j.survophthal.2009.04.005
- 9.McCallum E, Keren S, Lapira M, Norris JH. <p>Orbital Compartment Syndrome: An Update With Review Of The Literature</p>. OPTH. Published online November 2019:2189-2194. doi:10.2147/opth.s180058
- 10.Edmunds MR, Haridas AS, Morris DS, Jamalapuram K. Management of acute retrobulbar haemorrhage: a survey of non-ophthalmic emergency department physicians. Emerg Med J. Published online January 10, 2019:245-247. doi:10.1136/emermed-2018-207937
- 11.Burkat CN. Retrobulbar Hemorrhage. Arch Ophthalmol. Published online September 1, 2005:1260. doi:10.1001/archopht.123.9.1260
- 12.Neuhaus RW. Orbital Complications Secondary to Endoscopic Sinus Surgery. Ophthalmology. Published online November 1990:1512-1518. doi:10.1016/s0161-6420(90)32383-7
- 13.Dunya IM, Salman SD, Shore JW. Ophthalmic complications of endoscopic ethmoid surgery and their management. American Journal of Otolaryngology. Published online September 1996:322-331. doi:10.1016/s0196-0709(96)90019-8
- 14.Wladis EJ, Peebles TR, Weinberg DA. Management of Acute Orbital Hemorrhage With Obstruction of the Ophthalmic Artery During Attempted Coil Embolization of a Dural Arteriovenous Fistula of the Cavernous Sinus. Ophthalmic Plastic & Reconstructive Surgery. Published online January 2007:57-59. doi:10.1097/iop.0b013e31802c7e5a
- 15.Blair K, Alhadi S, Czyz C. Global Rupture . StatsPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK551637/
- 16.Belliveau MJ, Johnson D. Orbital compartment syndrome after head trauma. The Lancet Neurology. Published online February 2015:136-137. doi:10.1016/s1474-4422(14)70319-9
- 17.Mohammadi F, Rashan A, Psaltis A, et al. Intraocular Pressure Changes in Emergent Surgical Decompression of Orbital Compartment Syndrome. JAMA Otolaryngol Head Neck Surg. Published online June 1, 2015:562. doi:10.1001/jamaoto.2015.0524
- 18.Knoop K, Dennis W. Clinical Procedures in Emergency Medicine . 6th ed. Elsevier; 2014.
- 19.Ujam A, Perry M. Emergency management for orbital compartment syndrome—is decompression mandatory? International Journal of Oral and Maxillofacial Surgery. Published online November 2016:1435-1437. doi:10.1016/j.ijom.2016.08.001
- 20.Perry M. Acute Proptosis in Trauma: Retrobulbar Hemorrhage or Orbital Compartment Syndrome—Does It Really Matter? Journal of Oral and Maxillofacial Surgery. Published online September 2008:1913-1920. doi:10.1016/j.joms.2008.04.012
- 21.Fattahi T, Brewer K, Retana A, Ogledzki M. Incidence of Retrobulbar Hemorrhage in the Emergency Department. Journal of Oral and Maxillofacial Surgery. Published online December 2014:2500-2502. doi:10.1016/j.joms.2014.06.457
- 22.Yung C-W, Moorthy RS, Lindley D, Ringle M, Nunery WR. Efficacy of Lateral Canthotomy and Cantholysis in Orbital Hemorrhage. Ophthalmic Plastic & Reconstructive Surgery. Published online June 1994:137-141. doi:10.1097/00002341-199406000-00012
- 23.Iserson KV, Luke-Blyden Z, Clemans S. Orbital Compartment Syndrome: Alternative Tools to Perform a Lateral Canthotomy and Cantholysis. Wilderness & Environmental Medicine. Published online March 2016:85-91. doi:10.1016/j.wem.2015.09.002
- 24.McAllister AS. A clinical review of orbital anatomy and its relevance to retrobulbar anaesthesia. Cureus. Published online February 21, 2013. doi:10.7759/cureus.97
- 25.Vassallo S, Hartstein M, Howard D, Stetz J. Traumatic retrobulbar hemorrhage: emergent decompression by lateral canthotomy and cantholysis. The Journal of Emergency Medicine. Published online April 2002:251-256. doi:10.1016/s0736-4679(01)00477-2





